The cardiovascular implantable electronic device (CIED) infection rate is rising disproportionately to the rate of device implantation. Identification of microorganisms that cause CIED infections is not always achieved using present laboratory techniques. We conducted a prospective study to determine whether device vortexing-sonication followed by culture of the resulting sonicate fluid would enhance microbial detection compared with traditional swab or pocket tissue cultures. Forty-two subjects with noninfected and 35 with infected CIEDs were prospectively enrolled over 12 months. One swab each from the device pocket and device surface, pocket tissue, and the CIED were collected from each patient. Swabs and tissues were cultured using routine methods. The CIED was processed in Ringer’s solution using vortexing-sonication and the resultant fluid semiquantitatively cultured. Tissue and swab growth was considered significant when colonies grew on ≥2 quadrants of the culture plate and device was considered significant when ≥20 colonies were isolated from 10 ml of sonicate fluid. In noninfected group, 5% of sonicate fluids yielded significant bacterial growth, compared with 5% of tissue cultures (p = 1.00) and 2% of both pocket and device swab cultures (p = 0.317 each). In infected group, significant bacterial growth was observed in 54% of sonicate fluids, significantly greater than the sensitivities of pocket swab (20%, p = 0.001), device swab (9%, p <0.001), or tissue (9%, p <0.001) culture. In conclusion, vortexing-sonication of CIEDs with semiquantitative culture of the resultant sonicate fluid results in a significant increase in the sensitivity of culture results, compared with swab or tissue cultures.
The cardiovascular implantable electronic device (CIED) implantation rate has markedly increased, largely because of expanding indications for device implantation. This has been accompanied by an increasing rate of device infections. Infection is a serious complication of CIED implantation that necessitates device removal through percutaneous or surgical approach that is associated with significant morbidity and mortality and considerable financial burden for the patient and the health care system. Current guidelines recommend generator pocket tissue Gram stain and culture and lead-tip culture for identification of the causative microorganism(s). However, Gram stain has been shown to have limited utility in the diagnosis of device-related infections, and cultures may be negative for a variety of reasons, including concentration of organisms in biofilms on the device surface and consequently not in the surrounding tissue and the presence of so-called “small colony variants” that may be more difficult to isolate by routine cultures. Vortexing-sonication of implants followed by culture of the resultant sonicate fluid is more sensitive and specific compared with conventional periprosthetic tissue culture for the diagnosis of prosthetic joint infection. Consequently, this technique has been adopted in clinical microbiology laboratories across the world for the diagnosis of prosthetic joint infection. On the basis of findings from these investigations, we hypothesized that vortexing-sonication, followed by culture of the resulting sonicate fluid, will enhance microbial detection compared with traditional swab or pocket tissue culture for the diagnosis of CIED infection.
Methods
The study was conducted at Mayo Clinic, Rochester, from November 2011 to November 2012. Potential subjects were identified using the institutional operating room census and by direct communication with the electrophysiology and cardiac surgical services. Written informed consent was obtained from all study subjects. For patients who consented for participation and underwent explantation of a CIED, the following samples were collected: (1) CIED; (2) device surface swab; (3) pocket tissue swab; and (4) pocket tissue (∼1 cm 3 in size). The Mayo Clinic Institutional Review Board approved the study protocol.
CIED infection was defined as the presence of inflammatory changes (erythema, warmth, fluctuation, or purulent discharge) at the generator pocket site, persistently positive blood cultures in the absence of any other defined focus of infection or pathologic analysis of pocket tissue demonstrating acute inflammation. CIED-related endocarditis was defined on the basis of modified Duke criteria. Device generator or leads that eroded through the pocket were also classified as infected. We concurrently enrolled subjects with no clinical or pathologic signs of infection, typically patients who underwent replacement of a generator for “end of battery life,” as noninfected controls.
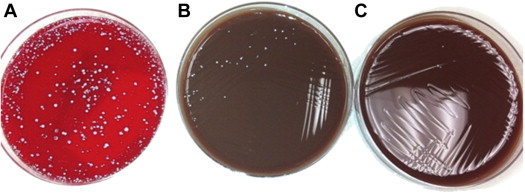
The swabs and tissues were subjected to routine microbiologic culture involving inoculation onto aerobic blood and chocolate agars, and in cases of tissues, onto anaerobic blood agar and into thioglycollate broth (BD Diagnostic Systems, Sparks, Maryland) as well. Aerobic and anaerobic sheep blood agar plates (BD Diagnostic Systems) were incubated at 35°C to 37°C in 5% to 7% CO 2 aerobically and anaerobically for 4 and 7 to 14 days, respectively. Cloudy thioglycollate broth was subcultured.
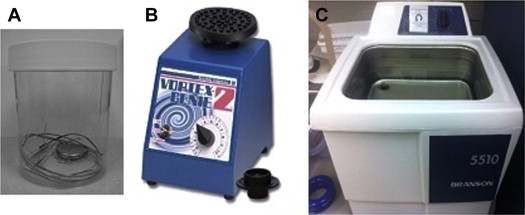
The cardiac device was sent to the laboratory in a sterile 1-liter, straight-sided, wide-mouthed polypropylene (Nalgene) jar. Four hundred milliliters of Ringer’s solution was added to the container. The container was vortexed for 30 seconds using a Vortex Genie (Scientific Industries Inc., Bohemia, New York) and then subjected to sonication (frequency 40 ± 2 kHz, power density 0.22 ± 0.04 W/cm 2 ) in 5510 model ultrasound bath (Branson Ultrasonics Corp., Danbury, Connecticut) for 5 minutes, followed by vortexing for an additional 30 seconds ( Figure 1 ). Fifty milliliters of sonicate fluid was placed into a conical tube and centrifuged at ×3,150 g for 5 minutes. The supernatant was aspirated leaving 0.5 ml remaining in the tube, 0.1 ml which was plated onto an aerobic and another 0.1 ml onto an anaerobic sheep blood agar plate which were incubated at 35°C to 37°C in 5% to 7% CO 2 aerobically for 4 days and anaerobically for 14 days. Microorganisms were enumerated and classified using routine microbiologic techniques ( Figure 2 ).
Host demographics, comorbidities, clinical signs and symptoms, laboratory parameters, and microbiologic results were collected using a data collection instrument and entered into a REDCap version 4.13.17 (Vanderbilt University, Nashville, Tennessee) database.
Sensitivity and specificity were calculated for device, swab, and tissue cultures, with infection status (gold standard) defined by clinical and pathologic criteria described previously. Device sonicate fluid cultures were classified as a positive versus negative result on the basis of a cut-off point of <20 colony-forming units/10 ml (CFU/10 ml) derived from a previous validation study of prosthetic joint infections at our institution. To test whether device sonicate fluid culture had greater sensitivity or specificity than each of the swab or tissue cultures for the diagnosis of CIED infection, McNemar test of paired proportions was used. A p value <0.05 was considered statistically significant. All analyses were performed using the SAS statistical software package version 9.3 (SAS Institute Inc., Cary, North Carolina).
Results
Ninety-three subjects were enrolled, of which 16 were excluded because of gross contamination of specimens during device extraction, specimen transportation delay of more than 12 hours, or failure to collect the requisite specimens. Of the 77 subjects included in the final analysis, 35 met the criteria for CIED infection and 42 were considered uninfected. There were no statistically significant differences in host, demographic, or clinical characteristics between these 2 groups ( Table 1 ) although infected subjects had marginally higher rates of diabetes (34 vs 17%, p = 0.074), chronic kidney disease (stage 3 or greater/glomerular filtration rate <60 ml/min/1.73 m 2 ; 29 vs 12%, p = 0.066), and previous history of CIED infection (14 vs 2%, p = 0.052).
| Demographic Characteristic | Infected ∗ (n=35) | Non-infected ∗ (n=42) | p-value |
|---|---|---|---|
| Age (in years) | 63.7±17.3 | 67.4±15.4 | 0.319 |
| BMI (kg/m 2 ) | 31.1±7.0 | 29.2±7.2 | 0.270 |
| Men | 24 (69%) | 25 (60%) | 0.411 |
| White | 33 (94%) | 41 (98%) | 0.588 ∗ |
| Hypertension | 21 (60%) | 24 (57%) | 0.800 |
| Hyperlipidemia | 23 (66%) | 30 (71%) | 0.590 |
| Diabetes Mellitus | 12 (34%) | 7 (17%) | 0.074 |
| Chronic Kidney Disease (GFR <60) | 10 (29%) | 5 (12%) | 0.066 |
| Immunosuppression | 4 (11%) | 1 (2%) | 0.109 |
| Coronary Artery Disease | 20 (57%) | 18 (43%) | 0.212 |
| Cerebrovascular Disease | 5 (14%) | 4 (10%) | 0.517 |
| Peripheral Vascular Disease | 2 (6%) | 1 (2%) | 0.588 ∗ |
| Chronic Obstructive Pulmonary Disease | 4 (11%) | 4 (10%) | 0.785 |
| Prosthetic Valve | 8 (23%) | 6 (14%) | 0.332 |
| Prior CIED Infection | 5 (14%) | 1 (2%) | 0.052 |
| Atrial Fibrillation | 9 (26%) | 17 (40%) | 0.173 |
| Heart Failure | 21 (60%) | 20 (48%) | 0.278 |
In the infected group, there were 12 cases of pocket cellulitis, 4 cases of device or lead erosion (without clinical signs of cellulitis around the pocket or positive blood cultures), 14 cases of bloodstream infection, presumably involving the intravascular portion of the lead(s), and 5 cases of CIED-related bloodstream infection simultaneously involving native or prosthetic heart valve(s) ( Figure 3 ). Twenty-nine (83%) subjects (4 with pocket infection and 2 with device erosion) had received antibiotic therapy before cardiac device extraction and specimen collection.
In the noninfected group, a number of culture plates yielded microbial growth, typically with low numbers of colonies (i.e., growth in the first quadrant/1 + growth/growth in broth only) of low-virulence organisms such as Bacillus sp., Corynebacterium sp., or Propionibacterium sp., which were likely representative of contamination. Moreover, comparing all specimens from each patient, none of the subjects had consistent growth of the same organism across all 4 specimens analyzed.
Because causative organisms (most commonly Staphylococcus aureus or Coagulase-negative Staphylococcus ) were known in cases of lead or valve endocarditis on the basis of persistently positive blood cultures, we analyzed the level of discordance between blood culture results and cultures of the specimens removed at the time of device removal. Of 19 cases of lead or valve endocarditis, sonicate fluid culture results were discordant with blood culture results in 3 subjects. Tissue and/or swab culture results were also discordant with the results of the blood cultures in 3 subjects. Results of both sonicate fluid and tissue/swab culture results were different from those of blood culture in 2 subjects, whereas 1 patient had discordant results exclusively with the sonicate fluid and another exclusively with the tissue/swab cultures.
Comparative results of sensitivity and specificity across different culture types are summarized in Table 2 . Although in noninfected subjects, 40% of sonicate fluids yielded any microbial growth on culture, compared with 33% of tissues (p = 0.366), 7% of pocket swabs (p <0.001), and 5% of device swabs (p <0.001), when disregarding minimal growth likely to represent contamination (i.e., <20 CFU/10 ml sonicate fluid and 1 + growth or growth in broth only for swab and tissue cultures, hereafter considered nonsignificant), 5% of sonicate fluids yielded a positive microbiologic result, compared with 5% of tissue cultures (p = 1.00) and 2% of both pocket and device swab (p = 0.317 each) cultures. Also based on significant positive growth, the overall sensitivity of sonicate fluid culture (54%) was greater than that of pocket swab (20%, p = 0.001), device swab (9%, p <0.001), and tissue (9%, p <0.001) culture.
| Test | Proportion | Sensitivity Rate, % (95% CI) | P-value ∗ | Proportion | Specificity Rate, % (95% CI) | P-value ∗ |
|---|---|---|---|---|---|---|
| Significant Growth | ||||||
| Device Swab | 3/35 | 9 (2-23%) † | <.001 | 41/42 | 98 (87-100%) | 0.317 |
| Pocket Swab | 7/35 | 20 (8-37%) † | 0.001 | 41/42 | 98 (87-100%) | 0.317 |
| Tissue | 3/35 | 9 (2-23%) † | <.001 | 40/42 | 95 (84-99%) | 1.000 |
| Sonicate Fluid | 19/35 | 54 (37-71%) | 40/42 | 95 (84-99%) | ||
| Any Growth | ||||||
| Device Swab | 10/35 | 29 (15-46%) † | <.001 | 40/42 | 95 (84-99%) † | <.001 |
| Pocket Swab | 15/35 | 43 (26-61%) † | 0.008 | 39/42 | 93 (81-99%) † | <.001 |
| Tissue | 16/35 | 46 (29-63%) † | 0.004 | 28/42 | 67 (50-80%) | 0.366 |
| Sonicate Fluid | 26/35 | 74 (57-88%) | 25/42 | 60 (43-74%) |
∗ p-value testing for a difference in performance rate relative to sonicate fluid culture via McNemar’s test.
† Value is significantly different from that by sonicate fluid culture (p <0.05 from McNemar’s test).
Subgroup analyses revealed evidence that the device sonicate fluid culture was generally more sensitive than the other tests in the infected subset with device erosion/pocket cellulitis and lead or valve endocarditis ( Table 3 ). For the 16 cases of device erosion/pocket cellulitis, sensitivity of either swab or tissue culture (based on significant positive growth) was only 38% (95% confidence interval [CI], 15% to 65%) compared with 69% (95% CI 41% to 89%) for device sonicate fluid culture (p = 0.059). For the 19 cases of lead or valve endocarditis, sensitivity of either swab or tissue culture (based on significant positive growth) was only 11% (95% CI 1% to 33%) compared to 42% (20% to 67%) for device culture (p = 0.014).



