Previous studies have shown the prognostic benefit of N-terminal pro–brain natriuretic peptide (NT–pro-BNP) in pulmonary arterial hypertension (PAH) at time of diagnosis. However, there are only limited data on the clinical utility of serial measurements of the inactive peptide NT–pro-BNP in PAH. This study examined the value of serial NT–pro-BNP measurements in predicting prognosis PAH. We retrospectively analyzed all available NT–pro-BNP plasma samples in 198 patients who were diagnosed with World Health Organization group I PAH from January 2002 through January 2009. At time of diagnosis median NT–pro-BNP levels were significantly different between survivors (610 pg/ml, range 6 to 8,714) and nonsurvivors (2,609 pg/ml, range 28 to 9,828, p <0.001). In addition, NT–pro-BNP was significantly associated (p <0.001) with other parameters of disease severity (6-minute walking distance, functional class). Receiver operating curve analysis identified ≥1,256 pg/ml as the optimal NT–pro-BNP cutoff for predicting mortality at time of diagnosis. Serial measurements allowed calculation of baseline NT–pro-BNP (i.e., intercept obtained by back-extrapolation of concentration–time graph), providing a better discrimination between survivors and nonsurvivors than NT–pro-BNP at time of diagnosis alone (p = 0.010). Furthermore, a decrease of NT–pro-BNP of >15%/year was associated with survival. In conclusion, a serum NT–pro-BNP level ≥1,256 pg/ml at time of diagnosis identifies poor outcome in patients with PAH. In addition, a decrease in NT–pro-BNP of >15%/year is associated with survival in PAH.
N-terminal pro–brain natriuretic peptide (NT–pro-BNP) concentrations have been shown to correlate with invasive pulmonary hemodynamics and outcome. Andreassen et al showed that NT–pro-BNP <553 pg/ml was related to better 6-month and 1-year survivals in 68 patients with pulmonary arterial hypertension (PAH) associated with scleroderma. Fijalkowska et al showed that NT–pro-BNP levels >1,400 pg/ml were predictive of 3-year outcome in 55 patients with severe PAH. Furthermore, NT–pro-BNP correlates with cardiac magnetic resonance imaging-derived measures of right ventricular function in pulmonary hypertension. These studies, however, have evaluated only the prognostic value of NT–pro-BNP at a single point. From left-sided heart failure it is known that serial measurements provide additional prognostic value compared to single values alone. Therefore, this study aimed to investigate in patients with PAH (1) the optimal cut-off value of NT–pro-BNP at time of original diagnosis in predicting mortality in a large patient population and (2) whether serial NT–pro-BNP measurements provide better information in addition to that of the value at diagnosis in predicting prognosis.
Methods
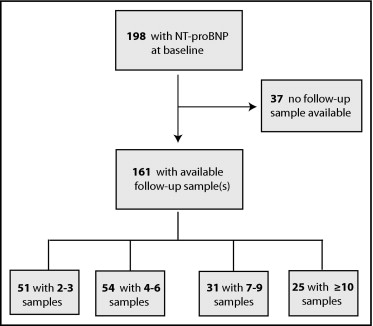
Serial cardiac biomarker measurement had been introduced at the department of pulmonology of VU Medical Center of Amsterdam (The Netherlands) since 2002 as part of routine clinical assessment. We retrospectively identified all patients who were diagnosed with World Health Organization group I PAH from November 2002 through September 2009. The study was approved by our institutional review board and ethics committee. All World Health Organization group I subgroups with ≥1 NT–pro-BNP measurement were included in this analysis (n = 198 patients). Thirty-seven of these had only a single measurement at baseline and these were not included in longitudinal analysis. Survival data were available for all patients until date of death or January 1, 2010. Follow-up was performed by regular visits to the outpatient clinic at 3- to 6-month intervals and by telephone contact.
Blood samples for NT–pro-BNP measurements were drawn from a peripheral vein in all patients while a patient was in a stable hemodynamic state before the 6-minute walk distance test was performed. Figure 1 shows available longitudinal data of NT–pro-BNP measurements for the 161 patients (determination at time of diagnosis). Because of the observational nature of this study the visiting patterns of the patients were rather variable. NT–pro-BNP plasma levels were analyzed with the Elecsys 1010 electrochemiluminescence immunoassay (Roche Diagnostics, The Netherlands) as described previously.
Differences in baseline covariates between survivors and nonsurvivors were tested with the Mann–Whitney U test. Multivariable Cox regression was used to assess the association between baseline log 10 (NT–pro-BNP) level and risk of death, adjusting for gender, age, New York Heart Association (NYHA) class, mRAP, and baseline eGFR.
To investigate the added value of serial NT–pro-BNP measurements, a 2-stage procedure was employed. In the first stage longitudinal information for each patient was summarized while accounting for the correlation in NT–pro-BNP serial measurements by a linear mixed-effects model with a random-intercepts and random-slopes structure. The aim of this model is to estimate the longitudinal evolution of NT–pro-BNP for each patient and account for biological variation. Typically, biomarker measurements such as NT–pro-BNP contain intrapatient “error,” which is also known as “biological variation.” More specifically, by biological variation we imply the fluctuations that are observed in the biomarker levels in human physiology. As shown in Figure 2 , patient B had a relatively stable profile of NT–pro-BNP levels over time; however, not all NT–pro-BNP measurements decrease exactly on the dashed line denoting this profile. Fluctuations of observed NT–pro-BNP levels around the profile denote biological variation. From a statistical point of view this variability should be taken into account to obtain optimal results because failure to account for this variation will lead to an underestimation of the effect size of NT–pro-BNP.

At the second stage the patient-specific intercepts (baseline value) and slopes were included as covariates in a similar multivariable Cox regression model as in the previous analysis, which also corrected for the effects of gender, age, NYHA class, mean right atrial pressure (mRAP), and baseline estimated glomerular filtration rate (eGFR).
Based on receiver operating characteristic curve analysis at 80 months, optimal cutpoints for baseline NT–pro-BNP and patient-specific intercept were determined as points for which the product of sensitivity and specificity attains its maximum. All analyses were performed in R 2.11.1 (2010) using JM 0.7, nlme 3.1, Survival 2.35, and Survival ROC 1.0.0 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Baseline characteristics of all 198 patients are presented in Table 1 . The population was predominantly women (71.2%) with a mean age of 54 ± 17 years. Fifty-six percent had idiopathic PAH and >58% were in modified NYHA/World Health Organization functional classes III and VI. PAH baseline therapies included prostacyclin analogs in 26 (13.1%), endothelin receptor antagonists in 118 (59.5%), and phosphodiesterase-5 inhibitors in 40 patients (20.2%). Eight patients received combination PAH therapies. Calcium channel blockers were used for PAH treatment in 5 patients (2.5%, data not shown).
| Variable | Total Population | Survivors | Nonsurvivors | p Value |
|---|---|---|---|---|
| (n = 198) | (n = 144) | (n = 54) | ||
| Age (years) | 54 ± 17 | 51 ± 17 | 63 ± 15 | <0.001 |
| Men/women | 49/149 | 31/113 | 18/36 | 0.1261 |
| Pulmonary arterial hypertension | ||||
| Idiopathic | 110 (56%) | 92 (64%) | 18 (34%) | 0.002 |
| Associated connected tissue disease | 58 (28%) | 35 (24%) | 23 (43%) | 0.021 |
| Associated portal hypertension | 11 (6%) | 6 (3%) | 5 (9%) | 0.290 |
| Associated human immunodeficiency viral infection | 6 (3%) | 5 (4%) | 1 (2%) | 0.889 |
| Drugs and toxins induced | 5 (3%) | 2 (1%) | 3 (6%) | 0.247 |
| Other | 7 (4%) | 5 (4%) | 3 (6%) | 0.791 |
| New York Heart Association functional class | ||||
| II | 82 (41%) | 71 (49%) | 11 (20%) | <0.001 |
| III | 94 (47%) | 67 (47%) | 27 (50%) | 0.773 |
| IV | 22 (12%) | 6 (4%) | 16 (30%) | <0.001 |
| 6-minute walk distance test (meters) | 387 ± 137 | 406 ± 137 | 326 ± 121 | 0.002 |
| Hemodynamics | ||||
| Heart rate (beats/min) | 79 ± 14 | 79 ± 15 | 82 ± 13 | 0.177 |
| Mean pulmonary artery pressure (mm Hg) | 45 ± 13 | 45 ± 10 | 46 ± 14 | 0.980 |
| Cardiac output (L/min) | 5.7 ± 2.3 | 5.9 ± 2.4 | 5.1 ± 2.1 | 0.039 |
| Pulmonary vascular resistance (mm Hg/L/min) | 607 ± 347 | 580 ± 344 | 676 ± 348 | 0.066 |
| Right atrial pressure (mm Hg) | 8 ± 7 | 7 ± 6 | 10 ± 8 | 0.049 |
| Pulmonary capillary wedge pressure (mm Hg) | 9.3 ± 6 | 9 ± 5 | 10 ± 3 | 0.554 |
| Blood gases | ||||
| Arterial oxygen saturation (%) | 93 ± 10 | 90 ± 11 | 94 ± 9 | 0.036 |
| Mixed venous oxygen saturation (%) | 66 ± 11 | 67 ± 10 | 65 ± 11 | 0.046 |
| N-terminal pro–B-type natruretic peptide (log 10 , pg/L) | 2.89 ± 0.69 | 2.75 ± 10 | 3.42 ± 0.63 | <0.001 |
| N-terminal pro–B-type natruretic peptide (pg/L) | 6,818 (287–3,039) | 610 (210–1,950) | 2,609 (872–5,335) | <0.001 |
During a mean follow-up period of 38 ± 23 months 54 patients (27.3%) died. Figure 3 shows the Kaplan–Meier estimate of survival function for the entire group. Overall survival estimates for our PAH population at 1 year, 3 years, and 4 years were 93% (95% confidence interval [CI] 90 to 97), 80% (95% CI 74 to 86), and 71% (95% CI 65 to 79), respectively. Pulmonary artery pressure and pulmonary vascular resistance (PVR) at baseline were similar for survivors and nonsurvivors. In contrast, those who died had significantly worse functional class and walked a significantly shorter distance in 6 minutes. Furthermore, their hemodynamic parameters (higher mRAP and lower cardiac output and mixed venous saturation) indicated more compromised right ventricular function.

Baseline NT–pro-BNP levels of survivors and nonsurvivors were significantly different ( Table 1 ). Plasma NT–pro-BNP increased significantly (p <0.0001, Kruskal–Wallis test) with severity of NYHA functional class ( Figure 4 ) . Of our patients 147 had diagnostic assessment and simultaneous NT–pro-BNP measurements at baseline. NT–pro-BNP was positively correlated with mRAP (Spearman correlation coefficient 0.26, p <0.001), serum creatinine (Spearman correlation coefficient 0.48, p <0.001), PVR (Spearman correlation coefficient 0.54, p <0.001), and heart rate (Spearman correlation coefficient 0.28, p <0.001), whereas negative associations were found with cardiac index (Spearman correlation coefficient −0.43, p <0.001) and mixed venous oxygen saturation (Spearman correlation coefficient −0.42, p <0.001).

An initial serum NT–pro-BNP cut-off value of 1,256 pg/ml (95% CI 811 to 1,700) for prediction of death was identified by receiver operating characteristic curve analysis (area under the curve 0.747). A serum NT–pro-BNP concentration of 1,256 pg/ml showed 63.5% sensitivity, 77.5% specificity, and a negative predictive value of 88.5% for a fatal outcome. Cox regression modeling confirmed that baseline NT–pro-BNP was highly significantly associated with mortality in our PAH patient population (p = 0.010; Table 2 ) adjusting for gender, age, NYHA functional class, mRAP and baseline eGFR. The hazard ratio for 1-U increase in baseline log 10 (NT–pro-BNP) was 1.92 (95% CI 1.01 to 3.64). Kaplan–Meier curves for survival in those with NT–pro-BNP levels >1,256 pg/ml and those with levels below this cutoff are shown in Figure 5 . Differences between the 2 groups were significant (p <0.0001, log-rank test).
| Baseline Measurement | Value | Hazard Ratio | SE | p Value |
|---|---|---|---|---|
| Female gender | 0.82 | 2.27 | 0.71 | 0.2473 |
| Age | 0.04 | 1.04 | 0.01 | 0.0004 |
| New York Heart Association class III | 0.33 | 1.39 | 0.39 | 0.3980 |
| New York Heart Association class IV | 1.09 | 2.97 | 0.46 | 0.0189 |
| Mean right atrial pressure | 0.02 | 1.02 | 0.02 | 0.4062 |
| Estimated glomerular filtration rate | −4.01 | 0.02 | 1.87 | 0.0324 |
| Log 10 (baseline N-terminal pro–brain natriuretic peptide) | 0.65 | 1.92 | 0.33 | 0.0469 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


