Postoperative atrial fibrillation (AF) is a serious yet common complication after coronary artery bypass grafting (CABG) surgery. Risk factors for postoperative AF have been identified, including echocardiographic parameters, and these are relied on to implement preventative strategies that reduce the incidence of AF. There has yet to be a study examining the impact of echocardiographic right-sided cardiac parameters on the prediction of postoperative AF. Thus, a panel of right-sided cardiac parameters was measured in a cohort of patients undergoing isolated CABG surgery, excluding those who did not have echocardiographic assessment within 30 days before surgery and those with any history of AF. The primary outcome was postoperative AF defined as any episode of AF requiring treatment during the index hospitalization. Postoperative AF occurred in 197 of 768 patients (25.6%); these were older and more likely to have hypertension and chronic kidney disease. After adjustment for clinical and echocardiographic variables, left atrial volume index ≥34 ml/m 2 (odds ratio [OR] 1.98, 95% confidence interval [CI] 1.36 to 2.87), abnormal right ventricular myocardial performance index (OR 1.50, 95% CI 1.01 to 2.24), and advancing age (OR 1.05, 95% CI 1.03 to 1.07) were found to be independent predictors of postoperative AF. In conclusion, right ventricular myocardial performance index is a novel predictor of postoperative AF in patients undergoing isolated CABG surgery and appears to be additive to established risk factors such as age and left atrial volume.
Postoperative atrial fibrillation (AF) is a serious yet common complication after coronary artery bypass grafting (CABG) surgery. Risk factors for postoperative AF have been identified and are relied on by clinicians to implement preventative strategies that have been shown to reduce the incidence of AF. To date, echocardiographic risk factors have been restricted to left-sided cardiac parameters such as left atrial volume and left ventricular (LV) function. There has not yet been a study examining the impact of echocardiographic right-sided cardiac parameters on the development of postoperative AF. Using the Pre-Operative Surgical Stratification by Echocardiography (POSSE) database, we hypothesized that echocardiographic right-sided cardiac parameters would provide additive prognostic value to predict the occurrence of postoperative AF.
Methods
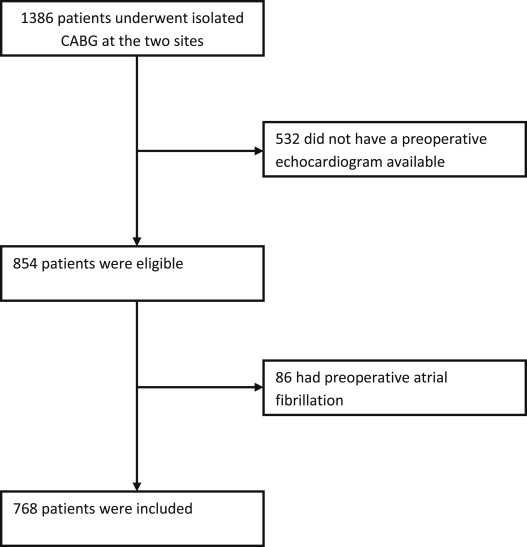
Consecutive patients undergoing isolated CABG surgery without concomitant repair or replacement of the heart valves or great vessels were identified within the POSSE database. Data were obtained from 2 university-affiliated hospitals in the United States (Massachusetts General Hospital, Boston, Massachusetts, January 1, 2007 to December 31, 2009) and Canada (Jewish General Hospital, Montreal, Quebec, September 1, 2010 to July 11, 2011). From this cohort, subjects who had a digitally available preoperative echocardiogram within 30 days before surgery were eligible for inclusion (n = 854). Subjects who had any history of AF were excluded ( Figure 1 ). The study protocol was approved by the institutional review boards of both hospitals.
Demographic data, preoperative clinical variables, operative variables, and postoperative in-hospital outcomes were extracted from the Society of Thoracic Surgeons Adult Cardiac Surgery Database at the Massachusetts General Hospital and from electronic medical records using identical data definitions at the Jewish General Hospital. These covariates included, but were not limited to, age, gender, body mass index, previous AF, supraventricular arrhythmia, ventricular arrhythmia, previous myocardial infarction, diabetes, hypertension, dyslipidemia, chronic kidney disease, chronic lung disease, peripheral arterial disease, cerebrovascular disease, preoperative creatinine level, preoperative medications, previous cardiac surgery and/or percutaneous coronary intervention, cardiac presentation, cardiogenic shock, intra-aortic balloon pump use, number of diseased coronary vessels, number of grafts, and whether the operation was elective or urgent/emergent.
Echocardiographic parameters were remeasured offline from the digital echocardiograms by independent echocardiography-trained cardiologists who were blinded to the study outcomes. Disagreements were resolved by consensus and/or a third senior observer. These parameters encompassed left- and right-sided chamber size, geometry, systolic function, diastolic function, as well as valvular regurgitation and stenosis. All were measured and classified according to the American Society of Echocardiography guidelines.
Right and left atrial areas were traced at end-systole in the apical 4-chamber view. Right ventricular (RV) endocardial borders were traced at end-diastole and end-systole in apical 4-chamber view. The RV fractional area change, a measure of RV systolic function, was calculated by the following formula: [(RV end-diastolic area−RV end-systolic area)/RV end-diastolic area] × 100. RV myocardial performance index (MPI), a measure of systolic and diastolic function, was measured by either the pulsed Doppler method or the tissue Doppler method and calculated using the following formula: [(tricuspid closure-opening time−ejection time)/ejection time], using a cutoff of 0.40 for both methods. Pulmonary artery systolic pressure was estimated using peak tricuspid regurgitation jet velocity with 10 mm Hg added for right atrial pressure. LV mass was measured using the Devereux method and indexed to body surface area. LV ejection fraction was measured using the biplane Simpson’s method. Several parameters including pulsed Doppler of the mitral and pulmonary vein inflow and tissue Doppler septal and lateral mitral annulus early diastolic velocities were integrated to determine LV diastolic function. The degree of valvular regurgitation and stenosis was assessed using a multiparametric approach according to the American Society of Echocardiography guidelines. Significant valvular regurgitation was defined as being at least moderate in severity.
Echocardiographies were performed with GE Vivid 7 or GE Vivid E9 machines and interpreted on EchoPAC workstations (GE Healthcare, Milwaukee, Wisconsin) at the Jewish General Hospital and with the Philips iE33, Sonos 7500 and Xcelera workstations (Philips Healthcare, Andover, Massachusetts) or GE Vivid 7 machines and EchoPAC workstation (GE Healthcare) at the Massachusetts General Hospital.
Patients were monitored by continuous telemetry for at least 72 to 96 hours after surgery and by 12-lead electrocardiographies performed on a routine daily basis and when indicated due to clinical signs. AF was recognized universally as a supraventricular arrhythmia with an irregularly irregular ventricular rhythm. The primary end point of this study was postoperative AF defined by the Society of Thoracic Surgeons as an episode of AF of any duration diagnosed by the attending physician that occurred during the in-hospital postoperative period and required treatment (medical therapy and/or electrical cardioversion). The decision to treat a patient for AF was at the discretion of the attending physician. Postoperative in-hospital outcomes other than postoperative AF included death from any cause, stroke, acute renal failure, prolonged intubation, the need of reoperation, and postoperative length of stay.
Continuous variables are reported as mean ± SD and compared using a 2-tailed Student t test. Categorical variables are reported as proportions and compared using the chi-square test or Fisher’s exact test as appropriate. Demographic, clinical, and echocardiographic variables were entered in a multivariate logistic regression model. The Akaike’s Information Criterion was used to select the optimal model (lowest Akaike’s Information Criterion) to predict postoperative AF. Stata 12 (StataCorp, College Station, Texas) was used to conduct analyses.
Results
The study population consisted of 768 patients (21.6% women), of which 197 patients (25.6%) developed postoperative AF. No patient was lost to follow-up for the primary outcome measure. Patients who developed postoperative AF were older (mean age 71.3 vs 64.9 years, p <0.001) and had a significantly higher rate of hypertension, chronic kidney disease, and congestive heart failure. They had slightly more number of diseased vessels and longer cardiopulmonary bypass times than patients without postoperative AF. There were no other notable differences between groups in baseline characteristics ( Table 1 ).
| Variable | Postoperative AF | p Value | |
|---|---|---|---|
| No (n = 571) | Yes (n = 197) | ||
| Age (yrs) | 64.9 ± 11.0 | 71.3 ± 9.9 | <0.001 |
| Women | 125 (21.9) | 41 (20.8) | 0.75 |
| Body mass index (kg/m 2 ) | 28.5 ± 4.8 | 28.5 ± 5.1 | 1.0 |
| Obesity | 185 (32.4) | 65 (33.0) | 0.88 |
| Hypertension | 443 (77.6) | 172 (87.3) | <0.01 |
| Dyslipidemia | 281 (49.2) | 88 (44.7) | 0.27 |
| Diabetes mellitus | 215 (37.7) | 71 (36.0) | 0.69 |
| Chronic kidney disease | 169 (29.6) | 93 (47.2) | <0.001 |
| Preoperative creatinine level (mg/dl) | 1.22 ± 0.73 | 1.26 ± 0.44 | 0.47 |
| Preoperative creatinine clearance | 80.0 ± 32.9 | 69.5 ± 34.7 | <0.001 |
| Chronic lung disease | 55 (9.6) | 19 (9.6) | 1.0 |
| Peripheral arterial disease | 83 (14.6) | 35 (17.8) | 0.28 |
| Previous cerebrovascular disease | 86 (15.1) | 39 (19.9) | 0.12 |
| Previous stroke | 48 (8.4) | 13 (6.6) | 0.42 |
| Myocardial infarction | 236 (41.4) | 82 (41.6) | 0.94 |
| Urgent/emergent operative status | 485 (84.9) | 168 (85.3) | 0.91 |
| Heart failure within 2 weeks | 129 (22.8) | 59 (30.6) | 0.04 |
| Number of diseased vessels | 3.5 ± 0.6 | 3.6 ± 0.6 | 0.04 |
| Cardiopulmonary bypass time | 121.1 ± 38.7 | 135.7 ± 52.4 | <0.001 |
| Preoperative medication use | |||
| ACE inhibitors | 156 (35.5) | 46 (28.8) | 0.23 |
| β Blockers | 400 (91.1) | 150 (93.4) | 0.49 |
| Statin | 334 (76.1) | 128 (80.0) | 0.58 |
| Inotropes | 8 (1.4) | 6 (3.0) | 0.32 |
| In-hospital outcomes | |||
| Mortality or major morbidity | 62 (10.9) | 47 (23.9) | <0.001 |
| Mortality | 3 (0.5) | 5 (2.5) | 0.03 |
| Stroke | 4 (0.7) | 5 (2.5) | 0.053 |
| Renal failure | 7 (1.2) | 17 (8.6) | <0.001 |
| Prolonged intubation >24 h | 39 (6.8) | 34 (17.3) | <0.001 |
| Need for reoperation | 28 (4.9) | 17 (8.6) | 0.055 |
| Postoperative length of stay (days) | 7.5 ± 4.5 | 12.5 ± 10.4 | <0.001 |
The composite outcome of in-hospital mortality and major morbidity was significantly higher in the postoperative AF group (23.9% vs 10.9%, p <0.001). With respect to individual outcomes, mortality, renal failure, and prolonged intubation rates were significantly higher in the postoperative AF group; stroke and reoperation rates tended to be higher in the postoperative AF group, although these outcomes did not reach statistical significance. In addition, patients with postoperative AF remained in hospital 5.0 days longer on average.
Echocardiographic variables for patients with and without postoperative AF are listed in Table 2 . With respect to right-sided parameters, patients who developed postoperative AF had larger right atrial size, worse RV MPI, worse tricuspid regurgitation severity, higher pulmonary artery systolic pressure, and no difference in RV fractional area change. With respect to left-sided parameters, patients who developed postoperative AF had larger left atrial size, larger LV end-diastolic volume and mass, and lower LV ejection fraction. Furthermore, they were more likely to have LV diastolic dysfunction and moderate mitral regurgitation. There were no cases of severe mitral or tricuspid regurgitation (given the isolated CABG cohort that did not undergo any valve procedures).
| Variable | Postoperative AF | p Value | |
|---|---|---|---|
| No (n = 571) | Yes (n = 197) | ||
| Left atrium volume index (ml/m 2 ) | 28.0 ± 11.4 | 32.0 ± 11.5 | <0.001 |
| LV end-diastolic volume index (ml/m 2 ) | 49.2 ± 18.2 | 55.7 ± 21.1 | <0.001 |
| LV ejection fraction (%) | 56.1 ± 12.9 | 53.7 ± 13.4 | 0.03 |
| LV diastolic function | |||
| Normal | 234 (41.2) | 65 (33.0) | <0.05 |
| Impaired | 195 (34.3) | 66 (33.5) | 0.87 |
| Pseudonormal | 77 (13.6) | 33 (16.8) | 0.26 |
| Restrictive | 37 (6.5) | 27 (13.7) | <0.01 |
| N/A | 25 (4.4) | 6 (3.1) | 0.41 |
| LV mass index (g/m 2 ) | 90.2 ± 24.2 | 94.8 ± 23.7 | 0.02 |
| Moderate/severe mitral regurgitation | 31 (5.4) | 19 (9.6) | 0.04 |
| Right atrial area index (cm 2 /m 2 ) | 7.1 ± 1.9 | 7.6 ± 1.9 | <0.01 |
| RV end-diastolic area index (cm 2 /m 2 ) | 7.9 ± 2.1 | 8.2 ± 2.3 | 0.09 |
| RV fractional area change (%) | 50.6 ± 8.7 | 49.5 ± 10.2 | 0.14 |
| RV MPI | 0.32 ± 0.14 | 0.37 ± 0.16 | <0.001 |
| Pulmonary artery systolic pressure (mm Hg) | 35.4 ± 10.2 | 39.4 ± 12.3 | <0.001 |
| Moderate/severe tricuspid regurgitation | 12 (2.1) | 10 (5.1) | 0.03 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


