Liver dysfunction has a prognostic impact on the outcomes of patients with advanced heart failure (HF). The model for end-stage liver disease (MELD) score is a robust system for rating liver dysfunction, and a high score has been shown to be associated with a poor prognosis in ambulatory patients with HF. In addition, cardiac metaiodobenzylguanidine (MIBG) imaging provides prognostic information in patients with chronic HF (CHF). However, the long-term predictive value of combining the MELD score and cardiac MIBG imaging in patients with CHF has not been elucidated. To prospectively investigate whether cardiac MIBG imaging provides additional prognostic value to the MELD score in patients with mild-to-moderate CHF, we studied 109 CHF outpatients (New York Heart Association: 2.0 ± 0.6) with left ventricular ejection fraction <40%. At enrollment, an MELD score was obtained, and the heart-to-mediastinal ratio on delayed imaging and MIBG washout rate (WR) were measured using cardiac MIBG scintigraphy. During a follow-up period of 7.5 ± 4.2 years, 36 of 109 patients experienced cardiac death (CD). On multivariate Cox analysis, MELD score and WR were significantly independently associated with CD, although heart-to-mediastinal ratio showed an association with CD only on univariate Cox analysis. Patients with abnormal WR (>27%) had a significantly greater risk of CD than those with normal WR in both those with high MELD scores (≥10; hazard ratio 4.0 [1.2 to 13.6]) and with low MELD scores (<10; hazard ratio 6.4 [1.7 to 23.2]). In conclusion, cardiac MIBG imaging would provide additional prognostic information to the MELD score in patients with mild-to-moderate CHF.
Liver dysfunction often coexists with heart failure (HF) as cardiac or congestive hepatopathy and is associated with adverse clinical outcomes in patients with advanced HF. The cardiohepatic syndrome, a condition characterized by the development of congestive hepatopathy in patients with advanced HF, has been recognized in the clinical settings. The model for end-stage liver disease (MELD) is a robust scoring system of liver dysfunction, and a high score has been shown to be associated with poor prognosis, not only in patients with advanced HF under consideration for heart transplantation and/or ventricular assist device but also in general patients admitted with decompensated HF. In patients with chronic HF (CHF), sympathetic overactivity contributes to the progression of the disease and is associated with an unfavorable prognosis. Cardiac iodine-123 (I-123) metaiodobenzylguanidine (MIBG) imaging, which is useful for the estimation of cardiac sympathetic nerve activity, has been reported to predict poor clinical outcomes in patients with CHF. The purpose of the present study was to investigate whether cardiac MIBG imaging can provide additional prognostic power to the MELD score in patients with mild-to-moderate CHF.
Methods
We studied 109 consecutive stable CHF outpatients with radionuclide left ventricular ejection fraction (LVEF) <40%, who had been diagnosed based on clinical signs and symptoms according to the Framingham criteria and enrolled in our previous prospective cohort study. None of the patients had an implantable cardioverter defibrillator (ICD), biventricular pacemaker, or biventricular defibrillator at enrollment. The exclusion criteria comprised significant renal (serum creatinine level >3 mg/dl) or hepatic dysfunction (aspartate aminotransferase or alanine aminotransferase >threefold of normal limit level), insulin-dependent diabetes mellitus, and autonomic neuropathy. The mean age of the patients was 63 ± 12 years. There were 82 men and 27 women. CHF was due to ischemic heart disease in 57 patients and idiopathic dilated cardiomyopathy in 52 patients. Mean New York Heart Association functional class was 2.0 ± 0.6, with 17% of patients in class I, 60% in class II, and 23% in class III. Mean LVEF was 30 ± 8%. At the time of entry into the study, all patients were prospectively assessed by cardiac MIBG imaging, echocardiography, and Holter electrocardiography, and a venous blood sample was withdrawn from each of them. Osaka General Medical Center’s Review Committee approved the protocol, and all patients provided written informed consent to participate.
All patients were assessed while at rest in the supine position by myocardial imaging with I-123 MIBG (FUJIFILM RI Pharma Laboratory, Tokyo, Japan) using the same gamma camera that was used for radionuclide angiography. The patients were injected intravenously with a 111-MBq dose of I-123 MIBG after an overnight fast. Initial and delayed anterior chest views were acquired at 20 and 200 minutes after the isotope injection. Two independent observers, who were unaware of the clinical status of the patients, assessed cardiac MIBG uptake as previously described. The heart-to-mediastinum ratios on early and delayed images were then calculated by dividing the mean counts/pixel in the left ventricle by those in the mediastinum. After taking into consideration the radioactive decay of I-123, the cardiac MIBG washout rate (WR) was calculated from the initial and delayed images. From the findings of our previous study, an abnormal WR was defined as >27%.
The patients were assessed by 2-dimensional echocardiography and 24-hour electrocardiogram as previously reported. Left ventricular end-diastolic dimension and left atrial dimension were measured using standard techniques, and ventricular arrhythmias were classified according to Lown’s grade.
Blood for measurement of serum levels of sodium, albumin, total bilirubin, aspartate aminotransferase, alanine aminotransferase, blood urea nitrogen, creatinine, uric acid, prothrombin time-international normalized ratio (PT-INR), hemoglobin, and plasma noradrenaline concentration was collected through an intravenous cannula inserted into patients who had rested for at least 30 minutes in the supine position. The MELD score was calculated by using the following formula: 11.2 × ln(PT-INR)+ 9.57 × ln(creatinine)+ 3.78 × ln(total bilirubin) + 6.43. We applied the MELD modifications adopted by the United Network for Organ Sharing.
All study patients were followed prospectively at our institution by clinicians who were blinded to the results of cardiac MIBG imaging. The primary end point of the present study was cardiac death (CD), which included sudden CD (SCD), defined as witnessed cardiac arrest or death within 1 hour after the onset of acute symptoms; unexpected or unwitnessed death in a patient who was known to have appeared well within the previous 24 hours; and pump failure death (PFD), defined as death because of progressively reduced cardiac output and failed organ perfusion.
Data are shown as the mean value ± SD. Differences among continuous and discrete variables were compared using the Student t test and Fisher’s exact test in patients with and without cardiac events, respectively. Cardiac event-free rates were calculated using the Kaplan–Meier method, and differences between each group were detected using the log-rank test. The Cox proportional hazards regression model was used to determine the significance of variables predictive of outcomes by univariate analysis (p <0.05) as independent predictors of cardiac events on multivariate analysis. The diagnostic utility of the MELD score was examined through the use of the receiver-operating characteristic curves (ROC), and the results are expressed in terms of the area under the curve and 95% CI for this area. All data were statistically analyzed using StatView, version 5 (SAS Institute, Cary, North Carolina), except for ROC analysis, which was analyzed using EZR, version 1.03 (Saitama Medical Center, Jichi Medical University, Saitama, Japan). p Values <0.05 were considered statistically significant.
Results
During a mean follow-up period of 7.5 ± 4.2 years, 45 patients died. A cardiac cause of death was noted for 36 patients. SCD was the most common cause of CD (n = 22), followed by PFD (n = 13) and death from acute myocardial infarction (n = 1).
The baseline characteristics of patients with and without CD are listed in Table 1 . There were no differences baseline characteristics between patients with and without CD, except for systolic blood pressure, LVEF, Lown’s grade, PT-INR, serum levels of total bilirubin, creatinine, and uric acid.
| Variables | Cardiac death | p Value | |
|---|---|---|---|
| Yes (n = 36) | No (n = 73) | ||
| Age (years) | 63 ± 12 | 64 ± 13 | 0.9757 |
| Men | 83% | 71% | 0.1718 |
| NYHA class | 2.2 ± 0.7 | 2.0 ± 0.6 | 0.1151 |
| Heart rate (beats/min) | 74 ± 11 | 74 ± 11 | 0.0958 |
| Systolic blood pressure (mmHg) | 123 ± 16 | 130 ± 18 | 0.0444 |
| Diastolic blood pressure (mmHg) | 72 ± 9 | 74 ± 10 | 0.3286 |
| Ischemic heart disease | 50% | 53% | 0.7392 |
| Atrial fibrillation | 27% | 13% | 0.0792 |
| Medications | |||
| ACE inhibitor/ARB | 81% | 92% | 0.0906 |
| Beta-blocker ∗ | 69% | 75% | 0.5167 |
| Loop diuretics | 74% | 63% | 0.1979 |
| Aldosterone antagonist | 36% | 37% | 0.9298 |
| Warfarin | 61% | 36% | 0.0114 |
| Radionuclide angiography | |||
| LV ejection fraction (%) | 26 ± 8 | 31 ± 7 | 0.0022 |
| Echocardiography | |||
| LVDd (mm) | 65 ± 7 | 62 ± 8 | 0.0701 |
| LAD (mm) | 45 ± 7 | 43 ± 8 | 0.2246 |
| Holter ECG | |||
| Lown’s grade | 4.0 ± 1.0 | 3.2 ± 1.5 | 0.0048 |
| Laboratory examination | |||
| Hemoglobin (mg/dL) | 13.5 ± 1.5 | 13.5 ± 1.6 | 0.8646 |
| Serum sodium (mEq/L) | 138 ± 3.4 | 139 ± 2.7 | 0.0974 |
| PT-INR | 1.3 ± 0.4 | 1.1 ± 0.3 | 0.0126 |
| Albumin (g/dL) | 4.1 ± 0.6 | 4.0 ± 0.4 | 0.0781 |
| Total bilirubin (mg/dL) | 0.9 ± 0.4 | 0.7 ± 0.3 | 0.0154 |
| AST (IU/L) | 30 ± 22 | 25 ± 17 | 0.1841 |
| ALT (IU/L) | 25 ± 23 | 23 ± 19 | 0.5428 |
| BUN (mg/dL) | 21 ± 12 | 18 ± 8 | 0.1198 |
| Creatinine (mg/dL) | 1.1 ± 0.4 | 0.9 ± 0.3 | 0.0425 |
| Uric Acid (mg/dL) | 7.5 ± 2.0 | 6.5 ± 1.8 | 0.0111 |
| Noradrenaline (pg/mL) | 506 ± 240 | 417 ± 234 | 0.0708 |
∗ Medication with β blocker (carvedilol) scored at the last follow-up.
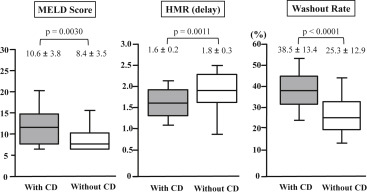
The results of the MELD score and cardiac MIBG parameters are shown in Figure 1 . The MELD score was significantly greater in patients with than without CD. Furthermore, patients with CD had a significantly lower heart-to-mediastinal ratio on the delayed image and a significantly higher WR than those without CD. ROC analysis revealed that an MELD score of 10 was a fair discriminator for CD (area under the curve 0.70 [95% CI 0.602 to 0.806]). Patients with MELD scores ≥10 had a significantly higher incidence of CD than those with MELD scores <10 (58% vs 19%, respectively, p = 0.0002).
Univariate and multivariate analysis for the identification of patients with CHF at risk for CD are presented in Table 2 . A multivariate Cox analysis revealed that abnormal WR, high (≥10) MELD score, and decreased LVEF were significantly independently associated with CD. Kaplan–Meier analysis ( Figure 2 ) in the subgroup with high MELD scores revealed that CD was significantly more frequently observed in patients with an abnormal WR than those without (70% [19 of 27] vs 31% [4 of 13], p = 0.028). Furthermore, in the subgroup of patients with low MELD scores (<10), the incidence of CD was also significantly higher in patients with an abnormal WR than in those without (34% [10 of 29] vs 8% [3 of 40], p = 0.005). The hazard ratio of an abnormal WR for CD was 4.0 (95% CI [1.2 to 13.6]) and 6.4 (95% CI [1.7 to 23.2]) in patients with high MELD scores and low MELD scores, respectively.
| Variables | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|
| p Value | HR (95% CI) | p Value | HR (95% CI) | |
| Cox proportional hazard model for CD | ||||
| Washout rate | <0.0001 | 1.051 (1.029-1.074) | 0.0002 | 1.046 (1.022-1.071) |
| High MELD score | 0.0002 | 3.743 (1.891-7.409) | 0.0120 | 2.761 (1.374-5.547) |
| Uric acid | 0.0003 | 1.368 (1.153-1.624) | ··· | ··· |
| Heart-to-mediastinum ratio from delayed images | 0.0006 | 0.165 (0.059-0.461) | ··· | ··· |
| Left ventricular ejection fraction | 0.0035 | 0.938 (0.898-0.979) | 0.0068 | 0.941 (0.898-0.986) |
| Lown’s grade | 0.0128 | 1.570 (1.101-2.241) | ··· | ··· |
| Left ventricular end-diastolic dimension | 0.0324 | 1.045 (1.004-1.088) | ··· | ··· |
| Plasma noradrenaline concentration | 0.0414 | 1.001 (1.000-1.002) | ··· | ··· |
| NYHA class | 0.0455 | 1.733 (1.011-2.972) | ··· | ··· |
| Warfarin use | 0.0457 | 1.981(1.013-3.874) | ··· | ··· |
| Systolic blood pressure | 0.0475 | 0.982 (0.964-1.000) | ··· | ··· |
| Cox proportional hazard model for SCD | ||||
| Washout rate | 0.0009 | 1.045 (1.018-1.073) | 0.0020 | 1.040 (1.012-1.068) |
| Heart-to-mediastinum ratio from delayed images | 0.0026 | 0.138 (0.038-0.499) | ··· | ··· |
| High MELD score | 0.0057 | 3.274 (1.411-7.594) | 0.0458 | 2.632 (1.113-6.221) |
| Plasma noradrenaline concentration | 0.0120 | 1.002 (1.000-1.003) | ··· | ··· |
| Uric acid | 0.0160 | 1.298 (1.050-1.650) | ··· | ··· |
| Lown’s grade | 0.0316 | 1.691 (1.047-2.730) | ··· | ··· |
| Left ventricular ejection fraction | 0.0440 | 0.946 (0.896-0.999) | ··· | ··· |
| Cox proportional hazard model for PFD | ||||
| Washout rate | 0.0010 | 1.062 (1.025-1.101) | 0.0330 | 1.047 (1.004-1.092) |
| Left ventricular end-diastolic dimension | 0.0052 | 1.089 (1.026-1.157) | 0.0080 | 1.105 (1.026-1.190) |
| Uric acid | 0.0059 | 1.542 (1.133-2.098) | ··· | ··· |
| Systolic blood pressure | 0.0060 | 0.956 (0.925-0.987) | ··· | ··· |
| High MELD score | 0.0092 | 4.800 (1.474-15.633) | 0.0281 | 4.204 (1.167-15.413) |
| Heart-to-mediastinum ratio from delayed images | 0.0236 | 0.156 (0.031-0.780) | ··· | ··· |
| Left ventricular ejection fraction | 0.0305 | 0.925 (0.861-0.993) | ··· | ··· |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


