Introduction
Economics is concerned with how to allocate scarce resources among alternative uses efficiently and effectively. It is a fundamental principle of economics that resources are limited relative to human wants, and that those resources have alternative uses.1 Consequently, when people say that the cost of healthcare has grown too high, they mean that the quantity of resources flowing toward medical care has grown to the point where additional funds cannot be spent on other things that society values, such as education, public safety, environmental protection, public works, pensions for the retired or disabled, or assistance to the poor. The fact that most people put a very high value on health does not mean that they are willing to provide limitless resources to medical care. Indeed, the goal of improving health and longevity may also be served by non – medical expenditures on programs such as nutritional supplements, a safe and clean water supply, police and fire protection or safety improvements to roads.
The cost of medical care has been rising steadily for the past 40 years in all developed countries2 but it has only been in the past decade that the level of expenditure has become so large as to cause alarm among policy makers, payers, and the general public (Table 4.1). The steady expansion of healthcare has now begun to meet substantial resistance in the large industrial countries, and new policies and payment mechanisms have been introduced to contain the rising cost of medical care. As a consequence, physicians must now consider cost as they design programs to prevent, diagnose, and treat disease. Cardiovascular diseases consume a large share of healthcare resources (Table 4.2), so cardiovascular specialists must be particularly knowledgeable about health economics.
Table 4.1 US national healthcare expenditures, 2006
Source: Health Affairs 2007;26:w242–w253
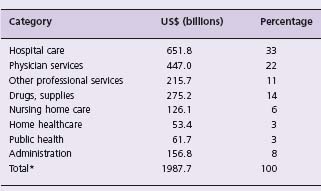
* per capita, $6641
Table 4.2 Resources devoted to cardiovascular care in the USA, 2005
Sources:a NCHS Monthly Vital Statistics Report 2007;56(No. 5)
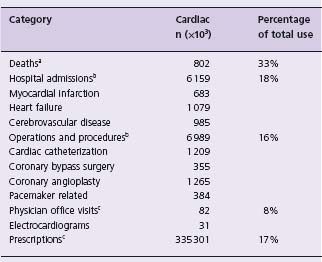
b NCHS Advance Data 2007 (No. 385)
c NCHS Advance Data 2007 (No. 387)Sources: aNCHS Monthly Vital Statistics Report 2007;56(No. 5)
This chapter will attempt to outline the major principles of health economics relevant to cardiovascular medicine. First, some general concepts of health economics will be presented. Second, methods to identify and compare the costs of cardiovascular interventions will be described. Finally, the principles of cost-effectiveness analysis will be discussed.
Various societies have adopted different systems to pay for healthcare and these systems reflect societal values and the historical experience within each country. The United Kingdom has a national health service, Canada has national health insurance, France and Germany have public/private financing for healthcare, and the United States has a perplexing and evolving patchwork of public and private health insurance systems. These are very different systems for financing healthcare and yet each is faced with the same issues of how to allocate the limited resources available to best provide healthcare. Each country is also facing the same steady rise of healthcare costs, despite the wide differences in the ways they finance healthcare.
Provision of cardiovascular services requires resources in all societies, irrespective of the method of financing or delivering healthcare. Coronary bypass surgery, for example, is very resource intensive, requiring cardiac surgeons, a cardiac anesthesiologist or anesthetist, a perfusionist, several nurses, and considerable quantities of specialized supplies and equipment. Postoperative care also requires skilled nurses and physicians, with support from specialized supplies, equipment, and facilities. Each health professional involved in cardiac surgery spends the scarce resource of time to care for the patient – time that could be put to other valuable uses, such as care for other patients. The drugs used, the disposable supplies, the operating room equipment, even the hospital building, all cost money. All of these are true costs to the system, even if the coronary bypass operation is performed “for free” – that is, without charge to the patient. The scene in the operating room, the postoperative recovery areas, and the hospital wards is much the same in the United Kingdom, Canada, France, Germany, and the United States despite the different ways in which these societies pay for medical care. The resources used in the care of patients and the increasing sophistication of that care drive healthcare costs up in each of these countries, irrespective of the way in which such care is paid for.
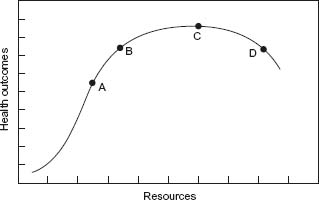
Another basic concept of economics is the so-called “law of diminishing returns”. This concept is illustrated in Figure 4.1, in which the quantity of resources used in healthcare is plotted on the horizontal axis and the resulting health benefits on the vertical axis. In the case of the patient with an acute myocardial infarction, for example, survival would be improved as more resources are applied, such as pre-hospital transportation, electrocardiographic monitoring, access to defibrillation, and a competent team to deliver coronary care. Outcomes might be further improved by reperfusion therapy, but with a greater increment in survival from using a cheaper, basic approach (streptokinase, for example) relative to no therapy than from more expensive alternatives (such as tissue plasminogen activator or primary angioplasty). The extra benefit from adding even more aggressive care will be smaller still, and at some point the patient may be harmed by overly aggressive care. Helping physicians to define the optimal point on this curve (Fig. 4.1) is one of the goals of economic analysis.
Figure 4.1 General relationship between increasing healthcare resources (horizontal axis) and health outcomes (vertical axis). At point A, outcomes are improving rapidly with increased resources and treatment is cost effective. At point B, outcomes are still improving with increased resources, but at a rate that is not cost effective. At point C, increased resources are no longer improving outcome (that is, “flat of the curve”), and at point D increased resources actually lead to worse outcomes, through iatrogenic complications and overtreatment.
The cost of producing a particular healthcare service can be defined in a variety of ways. The cost of performing a coronary angiogram can be used as a specific example that will illustrate the various aspects of cost and how the cost might be measured.
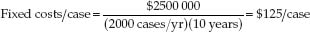
Performing a coronary angiogram requires a variety of resources, including radiographic equipment, trained personnel (including an angiographer and technical assistants), and specialized supplies such as catheters, radiographic contrast, and sterile drapes. The equipment needed is very expensive to purchase and the healthcare facility where it is installed may require special modifications to insure proper radiation shielding and adequate electrical power. The capital cost for a coronary angiography laboratory will be considerable, perhaps $2 – 3 million, depending on the type of equipment purchased. The laboratory will have a physical lifespan of perhaps 7 – 10 years, although technologic innovations may lead to replacement of the equipment before the end of its physical lifespan. The cost of building an angiography suite represents a large fixed cost for coronary angiography, a cost that is roughly the same whether the laboratory performs 200 or 2000 angiograms per year. The cost per case is lower in the high-volume laboratory, however, because the fixed equipment costs can be spread over more cases. Thus, if the equipment costs $2.5 million and has a useful life of 10 years, the prorated share of fixed costs for each patient in the low-volume laboratory performing 200 cases per year is:
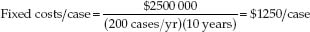
whereas in the high-volume laboratory (2000 cases per year) the prorated share of fixed costs per case would be:
Procedures that have high fixed costs will be performed with greater economic efficiency in centers that have sufficient volume to spread those fixed costs over a larger number of individual patients. (There may be additional advantages to larger procedure volumes as well, since the technical proficiency is higher and clinical outcomes of many procedures are usually better when performed in higher volume clinical centers.3–5) Procedures with lower fixed costs will have a smaller effect of volume on costs.
In contrast to the fixed equipment costs, the cost of supplies consumed in performing coronary angiography varies directly with the volume of cases performed, and the supply cost per case will be fairly constant irrespective of the volume of cases performed (apart from the small effect of discounts available to large-volume purchasers). The cost of laboratory staff falls in between these two extremes, in that the hours worked in the catheterization laboratory by technical staff can be varied somewhat according to the volume of cases performed, but some staff effort is required regardless of patient volumes, such as supervisors.
Hospital overhead is also a real cost but one that is less directly linked to any one medical service or procedure. Hospitals must pay for admitting offices, the medical records department, central administration, the laundry service, the cafeteria, housekeeping and utilities, to name just a few areas. These costs cannot be tied easily to the coronary angiography procedure in the same way as the cost of the catheters or radiographic contrast. Most facilities assign a share of these costs to patient care services according to a formula such as the step-down method. Discussion of specific methods to allocate hospital overhead is beyond the scope of this chapter but can be found in several articles and books.6,7
The overall effect of procedure volume on the cost per case is illustrated in Figure 4.2. In general, the cost per case declines as more cases are performed, up to the limit of the facility’s capacity (for example, 2000 cases). If volume increases further, more facilities must be built, increasing the cost per case, as more fixed costs are spread over a few more patients. Figure 4.2 also illustrates the distinction between concepts of “marginal cost” and long run “average cost”. The marginal cost is the added cost of doing one more case. In an already equipped and staffed coronary angiography laboratory, the marginal cost of performing one more procedure is just the cost of the disposable supplies consumed in the case: the catheters, radiographic contrast, and other sterile supplies. In the example of Figure 4.2, the marginal cost is $250 per case. The marginal cost is lower than the average cost per case ($375 per case), which also includes a prorated share of the salaries of the laboratory staff, depreciation of the laboratory equipment costs, and the facility’s overhead costs.
Figure 4.2 Cost per case for coronary angiography as a function of clinical volume. Assumes fixed costs per laboratory of $250000 per year, and marginal (that is, variable) costs of $250 per case. When volume reaches 2000 cases per year in a laboratory, the model assumes an additional laboratory will be built. The dotted line indicates the “long run average” cost per case of $375.
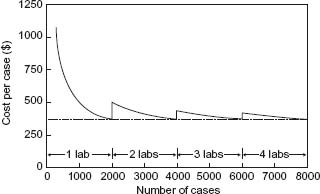
It is important to distinguish “cost per case” from “total health system costs”. The example above suggests that it is more economically efficient to perform 2000 procedures per year in one center (total cost $750 000/year) than it is to perform 500 procedures per year in each of four centers (total cost $1 500 000/year). Of course, if the four centers each performed 2000 procedures per year instead of 500 procedures, the total cost to the health care system would be higher overall ($3 000 000/year) even though the cost per case would have been reduced (from $750/case to $375/case).
The cost of providing a specific service, such as coronary bypass surgery, can be established in several alternative ways. In principle, one valid way to measure cost would be to identify a competitive market for medical service, and note the charge (price) for coronary bypass surgery in that market. While competitive market pricing might work well for commodities such as consumer electronic devices or farm products, it is not well suited to medical care, where there are few competitive markets. An alternative method is to take note of the charges for a service and apply correction factors to estimate cost more accurately. A third method to estimate costs is to examine in detail the resources used to provide a service, and apply price weights to the resources used.8
Most health economic studies currently use this third method to measure the costs of care. The price weights are taken from standardized reimbursement schedules (for hospital or outpatient services) or average prices (for drugs and supplies) paid in the community. A consistent set of price weights should be used, taking all the prices from the US Medicare system, for instance, or all from the US private insurance market.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


