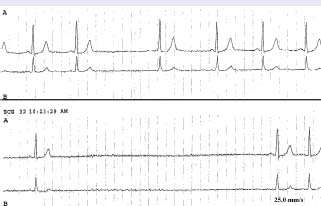
Figure 79.2 Holter monitor recording from Case 1 showing significant bradycardia and a sinus pause lasting 5.8 seconds. This pause was associated with severe presyncope.
Case history 2
A 72-year-old man is brought to the emergency department by his daughter after a syncopal episode. He was sitting on a chair when he suddenly lost consciousness for approximately 40 seconds. He recovered with no residual symptoms. When asked, he denied any prodromes but his daughter noticed transient cyanosis during the episode. Past medical history is significant for hypertension which was controlled after weight loss and low-salt diet.
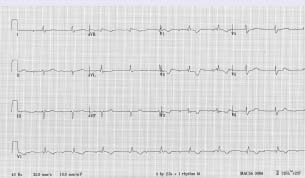
Physical examination reveals no acute distress with a blood pressure of 112/62 and a regular heart rate of 48 beats per minute. Chest exam shows good bilateral air entry and lungs are clear. Neck veins are 3 cm above the sternal angle. Normal S1 and S2. No added sounds or murmurs on auscultation. He is not a smoker and he has no history of stroke, coronary artery disease or diabetes. There is no previous history of syncope. A recent two-dimensional echocardiogram (three months ago) measured his left ventricular ejection fraction at 60%. A 12-lead ECG was obtained (Fig. 79.3).
Figure 79.3 Twelve-lead ECG from Case 2 showing complete third-degree heart block with right bundle branch block.
What is your diagnosis and what therapy is indicated for each patient?
In Case 1 the clinical presentation of syncope, presyncope and fatigue, temporarily related to sinus pauses on both the 12-lead ECG and Holter monitor, point to a diagnosis of sinus node dysfunction (SND). Before confirming the diagnosis, it is of key importance to exclude secondary causes of sinus bradycardia such as hypothyroidism or pharmacologically induced bradycardia.
SND constitutes a spectrum of cardiac arrhythmias including sinus bradycardia, sinus arrest, sinoatrial block, and paroxysmal supraventricular tachycardia alternating with periods of bradycardia or asystole. Patients with the latter condition may be symptomatic from paroxysmal tachycardia, bradycardia or both. Correlation of symptoms with the above-mentioned arrhythmias by use of 12-l ead ECG, Holter monitoring or event recorder is essential.
Sinus node dysfunction may present as chronotropic incompetence in which there is an inadequate response to exercise or stress. Chronotropic incompetence is defined as failure to achieve 85% of the predicted maximal heart rate during a treadmill stress test. Other more common causes of syncope such as vasovagal syncope should always be ruled out. However, this diagnosis is unlikely given the clinical presentation of syncope, presyncope and progressive fatigue induced by exercise in addition to symptom correlation of presyncope and a sinus pause >3 seconds (see Fig. 79.2).
Simple historic criteria have recently been described and a point score to rule out vasovagal syncope, known as the Calgary Syncope Score, that includes age of onset of syncope before age 35, classic prodrome, evidence of ECG alterations, and other clinical characteristics, has been validated.1 A point score <-2 had a high sensitivity and specificity for the diagnosis of vasovagal syncope. In both cases the Calgary Syncope Score was -7, which rules out vasovagal syncope. Case 1 has typical clinical and ECG features of SND and has a Class I, Level C indication for a permanent pacemaker.2,3 Sinus bradycardia is a physiologic finding in trained athletes, who frequently have resting heart rates between 40 and 50 bpm at rest. Moreover, rhythm changes during sleep such as sinus pauses > 2 seconds, sinus bradycardia (<40bpm), first-degree atrioventricular (AV) block and type I second-degree AV block are observed in up to 24% of healthy subjects.4 The patient presented in Case 1 has a Class I, Level C indication for a permanent pacemaker. Current Class I, Level C indications for sinus bradycardia syndromes are as follows; permanent pacemaker implantation is indicated for:
- SND with documented symptomatic bradycardia, including frequent sinus pauses that produce symptoms
- symptomatic chronotropic incompetence
- symptomatic sinus bradycardia that results from required drug therapy for medical conditions.
The patient presented in Case 2 has a clear presentation of abrupt syncope with no prodrome and ECG documentation of third-degree AV block associated with right bundle branch block (see Fig. 79.3). Patients diagnosed with high-degree AV block-third-degree or second-degree type 2 -are clearly at risk for adverse cardiovascular events if not treated with permanent pacemaker implantation.5,6 Therefore, this patient unquestionably benefits from a permanent pacemaker and also has a Class I, Level C indication.
Both cases may benefit from a single-chamber pacemaker. In Case 1 an atrial-based single-chamber pacemaker is appropriate and in Case 2 a single-chamber ventricular pacemaker may also be adequate. The need for a temporary transvenous wire is advocated by current ACLS guidelines7 for patients with second-degree AV block type 2 or third-degree AV block associated with signs or symptoms of poor perfusion secondary to bradycardia. Transvenous pacing may increase the risk of postoperative infection8 and cardiac perforation9 and should be reserved for carefully selected patients although these issues have not been addressed by randomized controlled studies.
Which is the most beneficial pacing mode for each patient?
The use of dual-chamber pacing offers theoretic advantages over ventricular pacing, such as maintenance of AV synchrony and preservation of normal ventricular activation through the His-Purkinje system (only in SND and depending upon a programmed long AV delay). Given the higher cost, greater complexity and increased complications of dual-chamber permanent pacemaker (PPM), several clinical studies assessed their potential benefit. In patients with SND, retrospective studies involving approximately 1400 patients suggest a significant survival benefit of dual-chamber PPM.10–16 However, this is observational information and randomized clinical trials are needed to establish the benefit of dual-chamber pacing.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


