Transverse gray scale
Spectral wave forms
CFV, SFJ (prox GSV)
Right and left CFV
Prox, mid, and distal FV
Pop V
Pop V
Post tib V
Peroneal V
Additional images as needed
Additional as per protocol
Additional as per protocol
6.2.2 Reflux (or Insufficiency) Documentation Protocol
For an insufficiency protocol, the goal is to determine the presence and pattern of venous reflux. Although DVT testing is not the primary goal, evaluating the deep system for thrombosis is still a critical aspect. This is an abbreviated exam compared to a full DVT protocol, but the insufficiency protocol includes some DVT-type determinations. Evaluation for DVTs is performed at the following locations: common femoral, SFJ, proximal great saphenous, mid-femoral, popliteal, and SSV. If a DVT is found, the typical protocol calls for a conversion to a standard DVT protocol in order to more fully document the DVT.
After this abbreviated DVT protocol, the reflux study continues to include spectral wave forms (typically using release of distal augmentation in the standing position, cuff inflators) of the following deep and superficial vessels: common femoral (right AND left), SFJ, femoral vein, great saphenous vein in multiple locations (from three to five sites), popliteal vein, and SSV (at least two sites). Other images are required in the following circumstances: the presence of disease or as per written protocol which typically calls for additional images to fully document the presence of disease; to understand the location and length and pattern of reflux if found; and in the interrogation of the varicose veins, perforators, and other veins suspected of reflux (according to written protocol). Listed in Table 6.2 are the basic insufficiency requirements. Additional aspects could include an evaluation using color and power Doppler flow imaging, which will vary according to individual lab protocols. Most significantly and covered in another section of this chapter is the creation of a venous reflux map, which is becoming the standard procedure in most dedicated vein treatment centers.
Table 6.2
Vascular testing protocol: reflux (insufficiency)
Transverse gray scale | Spectral wave forms |
|---|---|
CFV | CFV |
SFJ | SFJ |
Mid FV | FV |
GSV | GSV |
Pop V | Pop V |
SSV | SSV |
Additional images as needed | Suspected areas of reflux |
Additional as per protocol | Additional as per protocol |
6.3 Deep System Considerations
Although CVD is related to saphenous insufficiency and varicose veins, deep system analysis cannot be overlooked due to the significance of hemodynamics and overload. A recent consensus document from the International Union of Phlebology (UIP) suggests the underappreciated nature of deep system disease, including some interesting new trends and findings:
Partial correction of venous defects may have enormous influence on the clinical state.
Axial reflux is poorly tolerated by the skin and subcutaneous tissues of the lower extremity and deserves surgical correction. Axial deep vein reflux need not be corrected as the initial step when deep and superficial refluxes coexist.
Correction of post-thrombotic reflux can be achieved by direct repair when the proximal valve has not been destroyed.
Early restoration of iliac vein patency at the time of acute iliofemoral thrombophlebitis has shown improved long-term results and is becoming the norm.
It is now recognized that iliac vein obstruction is ubiquitous and is often present in silent form in the general population. In symptomatic (CEAP clinical 3–6) primary and post-thrombotic CVI patients, such lesions are present in >90 % when examined with intravascular ultrasound (IVUS) [19].
Further, when performing reflux testing on the deep system, particular attention needs to be paid to the deep system valves in the infra- and supra-saphenic positions in relation to a saphenous junction (i.e., SFJ or saphenopopliteal junction [SPJ] [Fig. 6.1]). Kostas et al. define reflux in the deep system as the “presence of reflux in any deep venous segment distal to the level of the common femoral vein and at least 1 cm away from the saphenofemoral or saphenopopliteal junctions where there was coexistent reflux at these sites” [20]. Others have described the segmental deep system reflux at the SFJ or SPJ as being actually a “siphon effect,” due to the suction created by the incompetent saphenous and varicose reservoir [21, 22]. This suggests that with the removal of the refluxing segment’s reservoir, the segmental deep insufficiency will correct, which has been seen in this author’s personal experience. Further, in the recent UIP consensus document on Duplex Reporting after Varicose Vein Treatment, there are clear recommendations that the deep system “should be examined in both the lying and standing position to check for residual obstruction and reflux, respectively” [23].
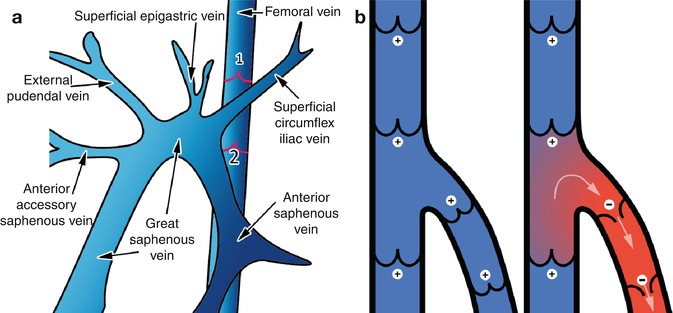
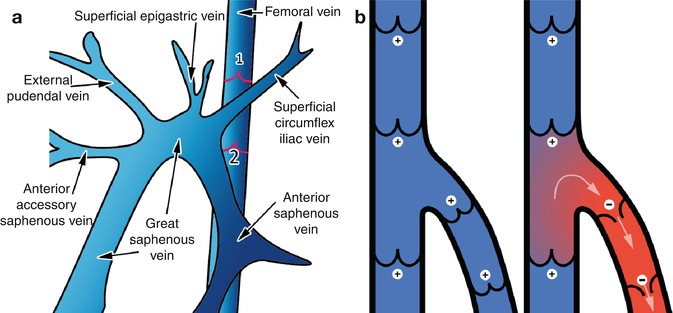
Fig. 6.1
(a) Illustration of the branches of the saphenous vein. The saphenous vein arch contains the space between the preterminal valve and the terminal valve. (b) The varicose reservoir below an incompetent segment reflux near a junction can create false deep vein reflux
With these concepts in mind, one can appreciate the importance of the DVT exam, and further, how the insufficiency evaluation of the deep venous system is equally important. In this regard, augmentation techniques are important and will be covered more fully later, but van Bemmelen clearly describes that “diastolic function of valves is clinically more important,” and goes on to state, “Valves refluxing while the patient is in the erect position may seem competent when the patient is in the supine position” and “Manual compression of the supine limb proximal to the transducer site did not result in closure of the valve but rather in reflux during the entire compression…” [4]. Those ideas can be distilled into the following practical information by this author: compression distal to the valve being tested is preferred; proximal compression should be avoided, with the exception of Valsalva for evaluation of the common femoral vein and SFJ; and a cuff device is more standardized and reproducible when compared to a hand augmentation.
6.4 Saphenous and Superficial Venous System General Considerations
The amount of information currently available on superficial venous anatomy and testing techniques has been vastly expanded over the past two decades. The following section will cover such aspects as terminology, overview of key anatomy, reflux, and factors that affect reflux reproducibility including augmentation techniques.
6.4.1 General Anatomy Basics
Although anatomy was covered more fully in an earlier chapter, understanding of some key anatomic facts assists the sonographer not only in gathering information during a diagnostic reflux exam but also in understanding and interpreting the results, so that clinical correlation and appropriate next steps can be considered.
Superficial veins are divided into saphenous and epifascial veins. Saphenous veins run in an “Egyptian eye” visible on transverse ultrasound (Fig. 6.2). As opposed to arteries, which bifurcate, veins are generally described from a normal flow direction, and therefore distal veins form a confluence (or union) with other veins, becoming larger as we move proximal or towards the heart. Regarding terminology, the generally accepted terms of great saphenous vein (GSV), and small saphenous vein (SSV), though ubiquitous in the phlebology community, are not yet well adopted in general medicine or by newcomers entering the field who still might inappropriately refer to the “L” lesser saphenous vein, or “superficial” femoral vein. The concept of a junctional “area,” sometimes referred to as the “saphenous arch” for the saphenofemoral junction (SFJ), includes a length of the saphenous vein that includes the preterminal valve.
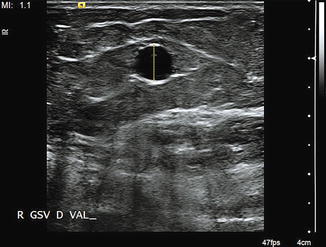
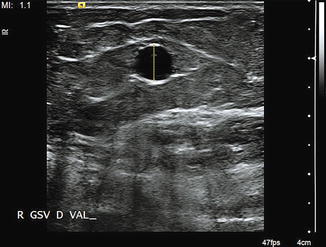
Fig. 6.2
Saphenous veins, by consensus definition [37], run in saphenous “eyes.” In this image, the black “pupil” (saphenous vein) is enclosed in the hyperechoic “globe” (fasciae) above and below the vein
Some general terms in the current language making their way into our diagnostic reports are: agenesis for either non-development of a vein or for varying degrees of incomplete development of a vein, aplasia being more severe than hypoplasia, and atrophy for a wasting away of a normal vein. Also, key points are that a venous aneurysm is a local dilation of a vein >50 % than the normal adjacent vein [24]. A true “duplication” of the great saphenous vein is one that occurs in the saphenous canal at an incidence of approximately 2 % and is much lower than previously reported [25]. As described in the UIP posttreatment document, venous measurements should be “performed in the transverse veins and the outer diameter should be measured (including the vein wall)….the saphenous trunk should be measured at a site where there is no focal (or aneurysmal) dilation of the trunk….for the GSV trunk, measurements…should be made 3 cm below the saphenofemoral junction (SFJ)” [23].
We also now appreciate the presence of the three compartments of the leg (N1 deep, N2 saphenous, and N3 epifascial), as well as the saphenous ligament, which is not present in conjunction with the epifascial tributaries. Additionally, though chronic venous disease is predominantly related to saphenous reflux, the diagnostic investigator will need to appreciate that approximately 9 % of CVD patients will have non-saphenous reflux patterns [26]. Unfortunately, pelvic symptoms related to CVD are often missed. Awareness of this category of non-saphenous reflux patterns can serve to refocus the clinician on pelvic issues. Finally with regard to anatomy, a reminder that the posterior tibial perforators (previously Cockett’s) connect the posterior tibial veins to the posterior accessory saphenous vein of the leg (previously posterior arch vein) and not to the distal great saphenous vein itself. Though not fully inclusive, these key points on anatomy and terminology should be kept in mind while performing diagnostic ultrasound for reflux; they will be invaluable for recognition and reporting.
6.4.2 Considerations on Reflux
The definition of reflux was made by Labropoulos et al., stating that abnormal retrograde flow and valve closure times for the superficial venous system in excess of 0.5 s defines pathologic reflux [7, 27]. For the femoropopliteal segment, 1.0 s is the cutoff. Further, reflux is related to fluid hemodynamics and typically involves a change in compartment (i.e., deep system [N1] leaking out into the superficial compartment [N2] or into the epifascial compartment [N3]). Even after several decades of reflux testing, there is no standardization in method or technique, but there are some relative consistencies. Some consider the “absolute quantitative” determination of reflux as a fool’s errand because there are so many factors that affect the amount, rate, and volume of reflux at any given time. Repeatability and reproducibility are compelling discussion points in reflux testing and have recently been investigated. Repeatability is the variability of the measurements obtained by one person while measuring the same item repeatedly, versus reproducibility, which is the variability in measurement caused by differences in operator behavior (i.e., between different sonographers). As presented recently at the American Venous Forum meeting, several key conclusions were drawn: “Repeatability of duplex ultrasound in detection of venous reflux is high; reproducibility of this test is sufficient and can be improved by educational intervention; testing patients at different times of day, in different positions, and using different reflux-provoking maneuvers significantly decreases reliability” [28]. In order to achieve the most accurate, reliable, and reproducible diagnostic testing results, the sonographic investigator needs to be aware of these factors and their impact, especially the reasons for false negatives. Some of these key factors will be explored further in this chapter. To emphasize the point, although these variables have influence, most clinicians with a phlebologic interest follow a set of “standardized” techniques that maximize accuracy and minimize variability. It should be noted that there is high confidence in these methods. Further, it is suggested that anyone performing reflux testing should adopt these techniques and clearly describe methods used in reporting, or any variations that occur on an individual case-by-case basis.
6.4.3 Time of Day
Although intuitively we understand that standing is a better position to test reflux than supine, does the time of day a reflux study is performed really have an impact? The Investigating Venous disease Evaluation and Standardization of Testing (INVEST) study suggests that including the time of day that testing was performed should be part of the reporting process, and this author agrees. If we think about the effects of gravity on reflux, it makes sense that the longer a patient is standing, the greater the impact of reflux. Also, it makes sense that while sleeping in bed, equilibration and normalization occurs. These considerations align with the general pattern of symptoms being worse with prolonged standing and relieved with rest and elevation. In one study, patients who work third shift (overnight) were considered outliers and eliminated from statistical analysis in its published data [29]. Further, this study reveals specifics of increased swelling, increased reflux in general, and especially reflux in perforators, as noted in afternoon examinations when compared to morning examinations. The changes in perforator reflux from abnormal to normal were stumbled upon during morning reexaminations to verify reflux prior to perforator interventions scheduled first thing in the morning. Varying results were noted when compared to the study performed the preceding afternoon. Others have described this variability [11, 30]. Ironically, no consensus on time of day for performing scans has been agreed upon. It is impractical to perform all studies in either the morning or afternoon. As stated above, the best line of thought is to realize this variability exists, especially when results do not match symptoms or clinical findings (false negatives), and to include time of day in the dictated report as suggested in the INVEST study.
6.4.4 Patient Position
As previously mentioned, reflux requires a pressure gradient, and this is not only typically related to compartment, but is also gravity dependent. Therefore, position of the patient is a key variable in the reflux determination process. Purists in the phlebology community adamantly defend the concept of standing evaluation for venous reflux [31–33]. The recent UIP document on posttreatment evaluation echoes this sentiment, “When assessing superficial veins, patients should be examined in the standing position where possible.” The INVEST study, though carried out using both standing and non-standing positions, indicates the “position of the patient” should be a part of the report. Typically, reflux evaluation in the standing position is performed on the non-weight-bearing leg to avoid effects of muscular systole on venous flow.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


