Fig. 19.1
Inflamed bulbous varices above and below the knee with an acute bout of STP
Superficial thrombophlebitis offers an array of presentations. Yet despite the knowledge that has emerged over the past 20 years, the curricula in medical schools and residencies fail to acknowledge STP as anything more than a self-limiting disease. The gap in venous education in the USA leads many unknowing providers to prescribe a recipe for thrombus extension, based upon established yet inaccurate dogma associated with STP. Although clinical trials are emerging, there is far more to be learned about this topic. Mass adoption of present management principles is not likely to occur overnight. The case presentations shared in this chapter will arm providers with the latest in peer-reviewed literature, enabling the reader to optimize outcomes through minimizing the risk of complications related to this common venous condition of the lower extremity.
Case 1. JJ
JJ is a 35-year-old Caucasian male with chief complaint of leg pain, aching, and heaviness for 2 weeks. He reports sudden onset of symptoms with “firm knots” over the medial and anterior thigh. JJ has suffered from symptomatic varicosities over the past 5 years. At the time of presentation, no therapy had been instituted.
There is no past medical history except for the presence of varicosities. He takes no medicines and shares no drug allergies. Family history is negative for varicose veins, venous ulcers, or “blood clots.” JJ is a business owner of a sports bar and limousine service and works long hours standing or sitting. He does not drink or smoke. Review of systems reveals no further concerns.
Vital signs as follows: Respiratory rate 12, heart rate 82, blood pressure 131/76, oxygen saturation 99 %, and a body mass index (BMI) of 40.4. Physical exam was unremarkable with the exception of left lower extremity cluster of veins with overlying erythema and proximal streaking (Fig. 19.2). No palpable cord is appreciated through the girth of the affected extremity.


Fig. 19.2
Case #1 – JJ’s physical findings. A dramatic inflammatory response is seen corresponding to painful thrombosed superficial varices
Given JJ’s history and physical findings:
Does this patient have the working diagnosis of STP?
What are the clinical features of STP?
What is the differential diagnosis of STP?
Does this patient have risk factors for DVT?
What tests are indicated at the initial evaluation of clinically suspected STP?
19.2 Clinical Features
Superficial thrombophlebitis offers a spectrum of presentations, yet the most common is that of sudden onset of leg discomfort with firm, inflamed varicosities. A palpable cord may be present with saphenous or deep venous involvement [1]. Fluctuance is frequently noted over the varicosities involved, and edema may be present. Inflammation over the region may at times be extreme despite the lack of a true infectious etiology [2]. In patients with severe and sustained inflammatory response in a superficial varix, hemorrhage may occur and thrombus may be expelled as the skin weakens [3]. As Sobreira et al. reported, the proximal most point of thrombus extends, on average, 15 cm beyond where clinically evident, rendering the physical exam a limited tool [4].
The inflammatory process that is commonly linear, forces us to consider other potential pathology and a broader differential diagnosis (Table 19.1). Historical features of exotic travel, intravenous drug abuse, recent hospitalization with intravenous catheter, insect bites, etc., offer added insight to the potential underlying pathology. The lower extremities are the most commonly involved site, yet STP may occur in superficial veins throughout the body, including upper extremity, breast, and genital veins [5–8]. Although the diagnosis of STP is typically not in question, the true extent and nature of thrombus burden must be verified.
Table 19.1
Differential diagnosis considerations for STP
Posttraumatic – hematomas adjacent to veins |
Venipuncture |
Intravenous drug abuse |
Allergic reaction to insect bites |
Filarial infestation |
Lymphangitis |
Cellulitis |
Erythema nodosum |
Erysipelas |
19.3 Epidemiology/Pathophysiology
The Tecumseh Community Health Study was the first large-scale effort to define the incidence of venous thromboembolic phenomena including superficial thrombophlebitis. Combining sequential history and physical exams, Coon et al. estimated the STP incidence between 3 and 11 % of the population [5]. At the time of the Tecumseh study, it was estimated that 123,000 cases occur each year [6]. The true prevalence is likely much higher. As duplex ultrasonography has emerged, we have learned much more about patterns of STP and complications associated with this disease state.
Nothing has been more important in understanding the patterns and clinical sequelae of superficial thrombophlebitis than the development of duplex ultrasound technology. In Lutter’s series of nearly 13,000 lower extremity duplex evaluations for deep vein thrombosis, 1,412 were found to have acute venous thrombosis. Of these, one of every eight was found to involve superficial venous system. The location of thrombus most commonly involved the great saphenous vein (GSV) (69 %), followed by the small saphenous vein (30 %), and isolated to varicose veins (13 %) [7]. Multi-segment involvement is commonly seen as is bilateral involvement (9 %) (Fig. 19.3).


Fig. 19.3
Bilateral STP Image. This image depicts bilateral STP involving varices below the knee on the right leg and the left anterior thigh
The pathophysiology of STP is thought to be similar to deep vein thrombosis, except STP is clearly associated with varicose veins as the predominant pattern [9]. Histopathology has been suggested to differ with regard to the extent of inflammation involving the vein wall, where STP involves a tremendous amount of inflammation compared to that found with acute deep vein thrombosis [8]. As shown in Fig. 19.4, extensive inflammatory changes are noted throughout the vein wall in a patient with phlebitis isolated to the superficial vessels. Over time the region of thrombus may become more organized and incorporated into the vein wall, may become completely recanalized, or may remain scarred with venous septae in an otherwise refluxing vessel [10] (Fig. 19.5).
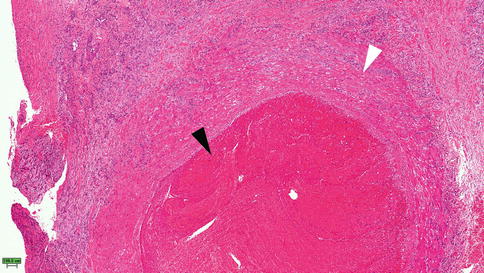
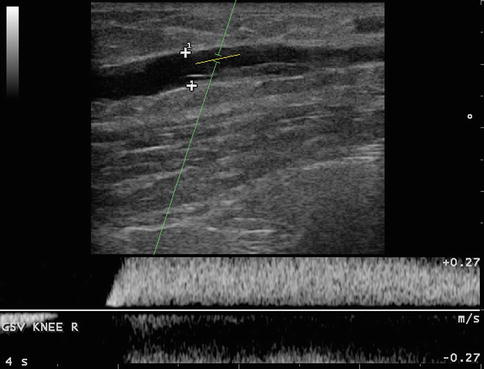
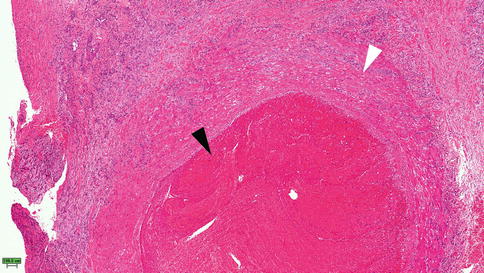
Fig. 19.4
Histopathology seen in acute STP, Case #1. Black arrow indicates thrombus within the vein lumen. White arrow indicates the transmural inflammation and neutrophil infiltration
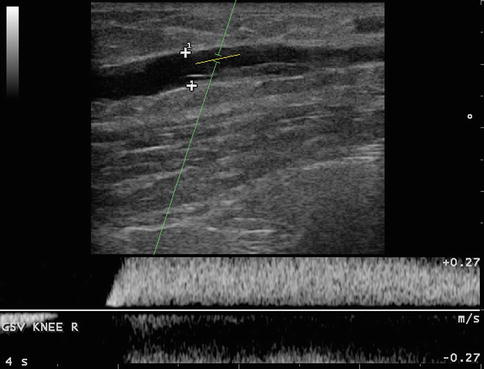
Fig. 19.5
Residual scar from STP in lumen of the great saphenous vein
19.4 Risk Factors for STP
When considering risks for the development of STP, one must reflect on Virchow’s triad including venous stasis (immobilization or reflux), vessel injury or trauma, and thrombophilia states due to hereditary or acquired conditions. The risks for developing superficial thrombophlebitis have been gleaned from numerous studies, many of which, not surprisingly, are well aligned with those of deep vein thrombosis (Table 19.2). The most common predisposing risk includes varicose veins in the lower extremity, occurring in 61–93 %, advancing age ≥60, female/male ratio of 2:1, obesity in 20 %, multiparity, recent surgery/immobilization, hormonal influences, history of prior venous thromboembolism (VTE), and hypercoagulable states including malignancy [9, 11]. Seasonal variations have also been reported where a peak incidence is seen in warmer summer months [11].
Table 19.2
Common risk factors for STP and DVT
Shared risk factors for STP or DVT |
Varicose veins |
Previous DVT/STP |
Immobilization |
Malignancy |
Trauma |
OCP/puerperium |
Hypercoagulable states |
19.5 Risk for VTE Complications/Recurrence
Superficial thrombophlebitis and the association with complications of DVT, with or without pulmonary embolus, have been noted for 7 years. Once thought to be a rare finding, duplex ultrasonography reports have revealed concomitant deep and superficial vein thrombosis at a rate of 8.6–24 % [9, 12–14] This confirms a reality that the clinical picture of superficial thrombophlebitis may, and often, harbors more serious sequelae than previously suspected.
There are two patient populations at the time of initial presentation, one of isolated STP and another with complications of concomitant DVT or pulmonary embolus. Identifying which patients possess the greatest propensity in developing VTE complications is of paramount importance.
19.6 Deep Vein Thrombosis
Anatomic location of the thrombus (e.g., near the saphenofemoral or saphenopopliteal junctions) has not been proven to yield a higher proclivity for VTE events. Lutter’s study compared populations with isolated STP to those with combined disease at initial presentation and found age >60, prior history of DVT, recent immobilization, and systemic infection as statistically significant risk factors for developing concomitant DVT and STP (Fig. 19.6). Quenet identified 427 consecutive hospitalized patients with isolated STP. Over the following 3 months, 4.1 % (17/413) were confirmed to have developed deep vein thrombosis. Univariate and multivariate regression analysis revealed male sex, history of VTE, severe chronic venous insufficiency, and sudden onset of STP as statistically significant risk factors for developing VTE complications [4].
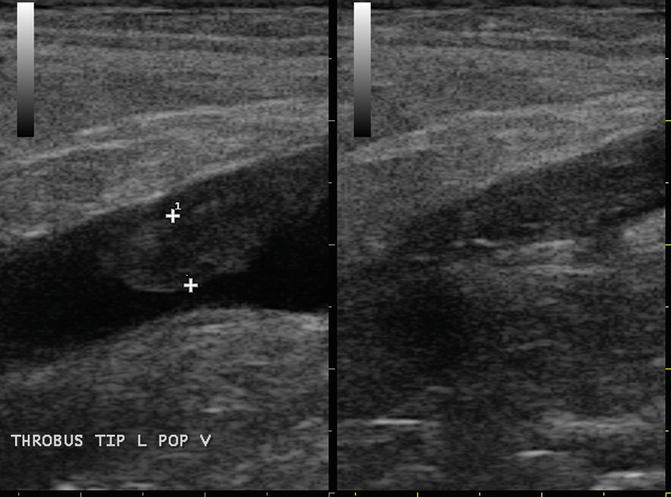
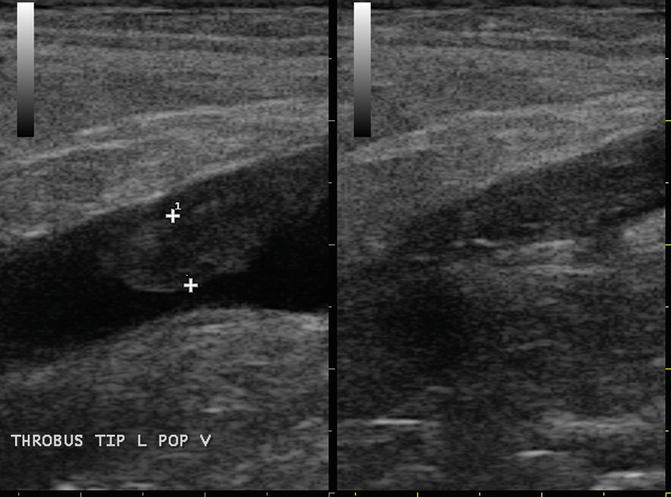
Fig. 19.6
STP at the saphenopopliteal junction with free-floating tongue
19.7 Pulmonary Embolus
The life-threatening complication of pulmonary embolus (PE) has been largely thought to occur only in the presence of deep vein thrombosis. STP as a suspected cause of pulmonary embolus was first described by Richter in 1905 [9]. Is it possible that isolated superficial thrombophlebitis may in fact cause pulmonary embolus? Verlato et al. prospectively studied 21 consecutive patients with isolated STP involving the proximal great saphenous vein. Each subject received systemic duplex scanning excluding presence of DVT through the calf veins and underwent chest radiography and pulmonary perfusion scanning. Surprisingly, despite general lack of symptomatology for pulmonary embolus, one-third was found to have high probability scintigraphy studies [12]. Sobreira et al. studied 60 consecutive patients with clinical findings of STP. Each subject received complete duplex scanning of the lower extremities and pulmonary perfusion scanning. Although 13 (21.7 %) patients were found to have concomitant DVT at presentation, 17 (28 %) were found to have high probability scans. Five of the 17 (29 %) found to have pulmonary embolus had concomitant DVT [10].
Although large randomized trials are lacking, the simultaneous occurrence of superficial and deep vein thrombosis suggests that this is more than a benign disease process [13, 14]. Epidemiology studies declaring the relatively high incidence of concomitant DVT and/or PE among STP patients warrant further consideration toward the prevention of further thromboembolic events. If merely 1 % of these cases result in PE or VTE complications, thousands of lives are placed at risk [15].
Case 2. JD (Fig. 19.7)

Fig. 19.7
Case #2 – JD’s calf image. This patient demonstrates painful bulbous varices of the calf with a faint pink hue after long car ride in a confined space
JD is a 70-year-old Caucasian male presenting with “knots” in the left calf after a 16 h car ride from coastal North Carolina to Chicago. He sat in the back seat of a car with confined space for leg room. He reported to an urgent care facility who made a diagnosis of STP, and he was referred for fitted gradient compression.
Past medical history is significant for degenerative joint disease, hypertension, hypercholesterolemia, and type II diabetes mellitus. He has no prior history of thrombosis yet has had varicose veins in the calf that have not previously been problematic. Family history is negative for varicose veins, venous ulcers, or “blood clots.” JD does not drink or smoke. He enjoys golf and church activities. Review of systems was noncontributory.
JD has normal vital signs, oxygen saturation of 98 %, and a BMI of 29.0. He communicates easily and appears in no distress. Physical findings reveal a firm, tender, inflammatory region in the medial proximal calf, corresponding to an intersaphenous branch. A pink hue is present over the firm varicosities. Trace edema is noted at the ankle in addition to high-pressure telangiectasia.
The urgent care advised the use of an anti-inflammatory reported that an antibiotic may be required if there was no improvement. No laboratory tests or imaging tests performed at the time of his initial evaluation.
What risk factors does JD possess that place him at risk for developing STP?
What risk factors does JD possess that place him at risk for VTE?
Describe a practical approach to evaluate JD and guide his treatment.
Do you agree with the urgent care recommendations of anti-inflammatory agents, an antibiotic, and compression therapy? Please explain.
19.8 Diagnostic Approach
Superficial thrombophlebitis most often occurs in patients with varicose veins but may also occur in normal saphenous veins in patients with an underlying thrombophilia. Given the common findings of DVT and/or pulmonary embolus in patients with superficial thrombophlebitis, once the clinical assumption is made, affirmation requires further diagnostic testing.
19.8.1 Duplex Ultrasonography
The prevalence of concomitant venous complications in patients with superficial thrombophlebitis mandate duplex ultrasound for each patient suspected of this condition [13, 14]. Duplex evaluation is valued for proving the diagnosis of STP while accurately assessing the thrombus burden throughout the lower extremity. The results of the duplex study serve to not only declare the presence or absence of thrombus but aid in identifying presence of complications found commonly in patients with STP. Simply put, duplex ultrasonography is the most critical of studies to perform and may indicate a need for more advanced imaging.
19.8.2 Acute Phase Testing
Principles of assessing a lower extremity for thrombosis are well documented. Systematic comprehensive whole-leg assessment of venous anatomy be mapped and for thrombus burden and the extent of venous reflux [13]. Bilateral scanning is indicated when bilateral symptoms are present and when institutional protocols mandate the study. Complete testing of an asymptomatic contralateral limb is debatable beyond assessing the most proximal segments of the limb [14].
As seen in an acute setting, probe compression in the region of thrombosis reveals noncompressible vessels which are hypoechoic (Fig. 19.8). The standard commonly used in clinical studies to define thrombus in the great or small saphenous vein includes a segment at least 5 cm in length (Fig. 19.9). A free-floating thrombus tip may be seen as an extensive STP protrudes into the lumen of the common femoral or popliteal vein (Fig. 19.10a, b). Valsalva testing and spectral waveform patterns are helpful in assessing presence of proximal obstruction (Fig. 19.11). Duplex findings or signs of proximal involvement should trigger algorithms to address pelvic vein pathology and the central circulation.
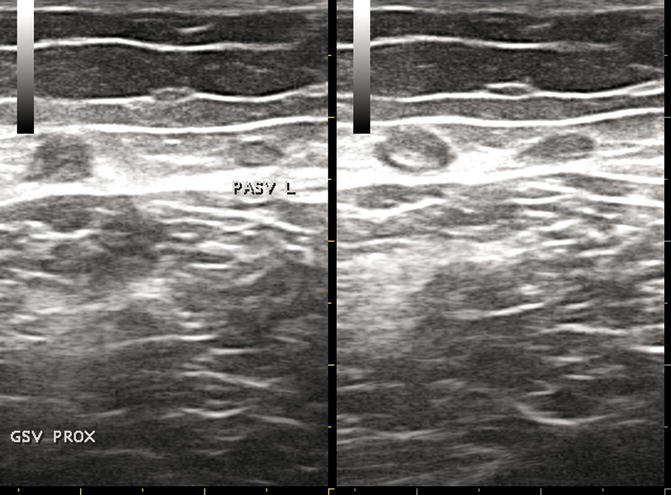

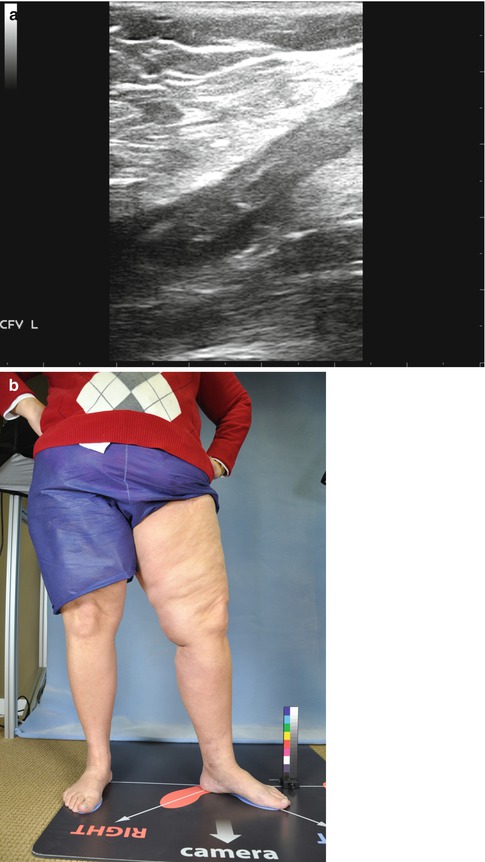
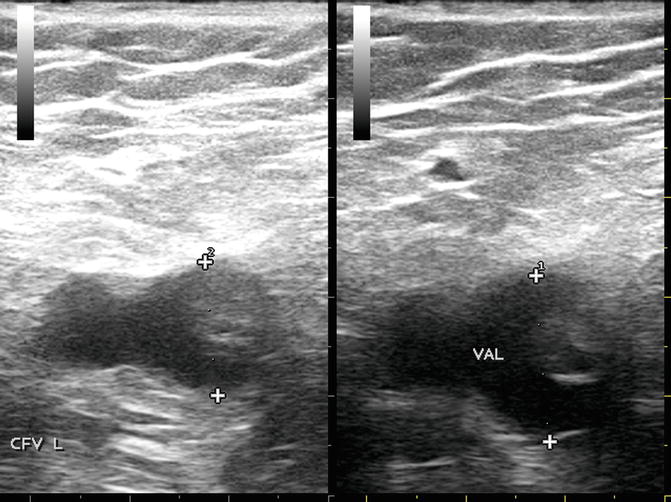
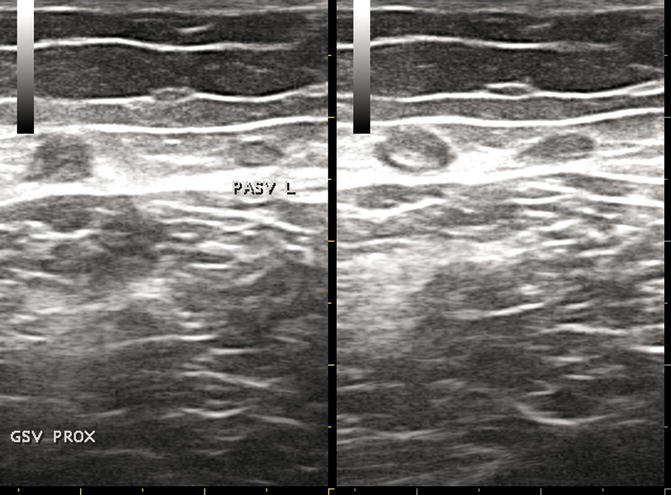
Fig. 19.8
STP of the GSV. Probe compression reveals limited compression of the great saphenous vein of the proximal thigh

Fig. 19.9
STP and thrombus tip in mid-thigh in a nondilated saphenous vein
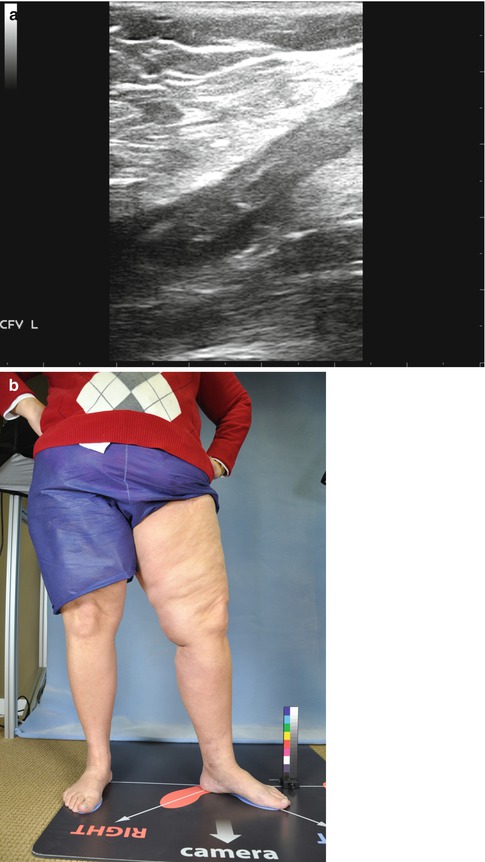
Fig. 19.10
STP at the saphenofemoral junction (duplex and standing photo of limb). (a) This image depicts the thrombus extending from the GSV through the SFJ and into the CFV for the patient below. (b) This image demonstrates limited findings with focal tenderness at the knee
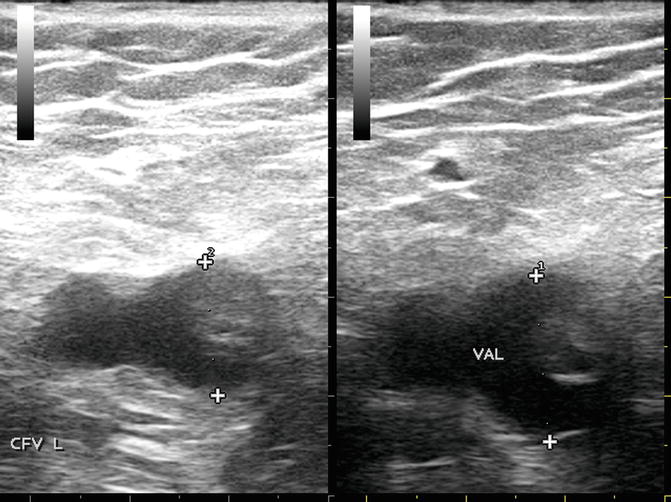
Fig. 19.11
CFV with STP extension with and without Valsalva
19.8.3 Follow-Up Duplex Scanning
Although there may be institutional standards, there are generally no accepted principles for serial duplex scans in this patient population [16]. Despite the argument regarding cost effectiveness, periodic surveillance of thrombus burden is strongly recommended for patients at higher risk for thrombus extension (e.g., involving proximity of the saphenous junctions or proximal one-third of the great saphenous vein) [4]. If the patient is not a candidate for anticoagulation, sequential scanning is imperative. As the majority of thrombus extends during the first week, a general rule of thumb is to reimage patients within 2–10 days [17, 18]. Additional studies are recommended for increasing pain or swelling of the affected limb and near the anticipated end of anticoagulation. This permits not only an assessment of residual thrombus burden but insight to residual reflux and permits a provider to determine the best surgical course of action if indicated.
19.8.4 Laboratory Testing
Patients with their first bout of superficial thrombophlebitis may indeed be manifesting their first event of an as of yet unknown thrombophilia [17]. The incidence of hypercoagulable conditions has been as high as 35 % in a series reported by Hanson et al. [19]. Schonauer prospectively observed 615 patients with first VTE who had completed 3 months anticoagulation therapy. Over an average of two and one-half years, 45 (7.3 %) STP events were reported. When analyzed, elevated factor VIII levels proved to be an independent risk factor for developing STP [20]. Recently, MTHFR C677T polymorphism was found to be significantly higher in patients with superficial thrombophlebitis when compared to patients with DVT [21]. Despite the reality that an underlying thrombophilic state may exist in a substantial percentage of patients with STP, acute phase laboratory testing is best geared toward those commonly performed prior to initiating anticoagulation. In these patients, a complete blood count with differential and platelets, PT/aPTT, and D-dimer generally suffice in the acute phase. Given the features of assessing a patient for inherited thrombophilia, it is not only timing of testing that is important, but rather an assessment whether the findings may change the course of management [21]. A thorough review of thrombophilia and testing may be found in the chapter dedicated to this topic.
Case 3. JA (Fig. 19.12)
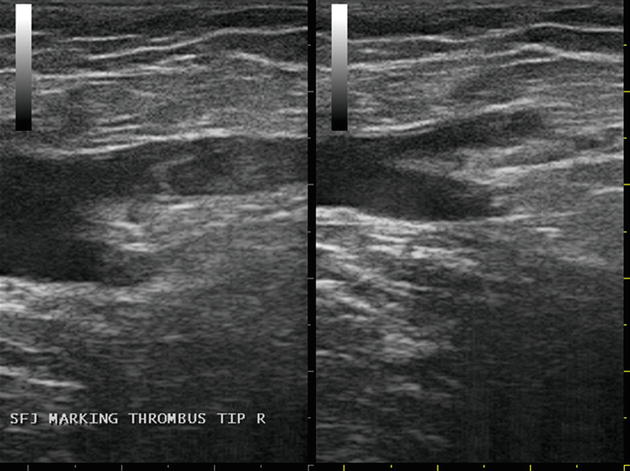
Fig. 19.12
Case #3 – JA SFJ with and without compression
JA is a 38-year-old Caucasian male presenting with chief complaint of “firm painful knot” over the right anterior thigh for 1 week. The discomfort is constant and associated with red streaking along the inner thigh and superficial vessels of the anterior thigh and leg. There are no aggravating or relieving factors and no therapy had been instituted. Past medical history is significant for apparent uncomplicated STP 3 years prior, and a remote right ankle injury without loss of function. Family history is negative for “blood clots” or known thrombophilia, yet positive for varicose veins and severe venous insufficiency. JA is married, he is a nonsmoker. He is a successful farm equipment salesman, spending long hours on the road. Review of systems revealed a 1 week history of nonproductive cough and dyspnea.
Vital signs reveal a respiratory rate of 20, heart rate of 72, a blood pressure of 128/70, and oxygen saturation of 98 %. JA is morbidly obese in no apparent distress. Physical exam was unremarkable with the exception of an extensive superficial thrombophlebitis with firm, painful varices with overlying inflammation above and below the knee. A palpable cord was easily noted along the medial thigh from just below the knee to the proximal thigh. Pretibial edema is noted, and pulses are equal bilaterally.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


