Early revascularization is the mainstay of treatment for cardiogenic shock (CS) complicating acute myocardial infarction. However, data on the contemporary trends in management and outcomes of CS complicating non–ST-elevation myocardial infarction (NSTEMI) are limited. We used the 2006 to 2012 Nationwide Inpatient Sample databases to identify patients aged ≥18 years with NSTEMI with or without CS. Temporal trends and differences in coronary angiography, revascularization, and outcomes were analyzed. Of 2,191,772 patients with NSTEMI, 53,800 (2.5%) had a diagnosis of CS. From 2006 to 2012, coronary angiography rates increased from 53.6% to 60.4% in patients with NSTEMI with CS (p trend <0.001). Among patients who underwent coronary angiography, revascularization rates were significantly higher in patients with CS versus without CS (72.5% vs 62.6%, p <0.001). Patients with NSTEMI with CS had significantly higher risk-adjusted in-hospital mortality (odds ratio 10.09, 95% confidence interval 9.88 to 10.32) as compared to those without CS. In patients with CS, an invasive strategy was associated with lower risk-adjusted in-hospital mortality (odds ratio 0.43, 95% confidence interval 0.42 to 0.45). Risk-adjusted in-hospital mortality, length of stay, and total hospital costs decreased over the study period in patients with and without CS (p trend <0.001). In conclusion, we observed an increasing trend in coronary angiography and decreasing trend in in-hospital mortality, length of stay, and total hospital costs in patients with NSTEMI with and without CS. Despite these positive trends, overall coronary angiography and revascularization rates remain less than optimal and in-hospital mortality unacceptably high in patients with NSTEMI and CS.
Cardiogenic shock (CS) complicates 2.5% to 4.7% of cases with non–ST-elevation myocardial infarction (NSTEMI). Early revascularization is the mainstay of treatment for CS complicating acute myocardial infarction and is associated with improved short-term and long-term survival compared with medical therapy alone. However, most studies on the management and outcomes of CS have focused on STEMI. Patients with NSTEMI and CS are less likely to receive urgent revascularization, have longer delays in percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG), and have similar or even higher mortality as compared to patients with STEMI and CS. Early revascularization rates have increased and in-hospital mortality decreased over the recent years in patients with STEMI and CS. However, limited data are available on the contemporary trends in coronary angiography, revascularization, and mortality in patients with NSTEMI complicated by CS. The primary objective of this study was to examine temporal trends and differences in utilization of coronary angiography, revascularization, and in-hospital outcomes in patients with NSTEMI with and without CS using the 2006 to 2012 Nationwide/National Inpatient Sample (NIS) databases.
Methods
Data were obtained from the 2006 to 2012 NIS databases. The NIS is the largest publicly available, all-payer, inpatient care database in the US containing nationally representative data on about 8 million hospital discharges from about 1,000 hospitals sampled annually. Up to 2011, the NIS included a 20% stratified sample of hospitals from which all discharges were retained. Beginning in 2012, the NIS was redesigned to improve national estimates. The 2012 NIS is a 20% sample of discharges from all community hospitals participating in Healthcare Cost and Utilization Project. To facilitate analysis of trends using multiple years of NIS data, the Agency for Healthcare Research and Quality developed new discharge trend weights for earlier NIS data.
We used the International Classification of Diseases, Ninth Edition, Clinical Modification (ICD-9-CM) code 410.71 to identify all patients aged ≥18 years with a principal diagnosis of NSTEMI (n = 2,763,250). We chose the principal diagnosis because it is considered as the primary reason for hospital admission. We excluded discharges with missing data on in-hospital mortality and/or length of stay (LOS; n = 970), those in which patients were admitted and discharged alive the same day (n = 57,014), as they may not reflect true diagnoses of NSTEMI, and discharges in which patients were admitted from other hospitals (n = 513,494) to avoid duplication of records. This gave us a final study cohort of 2,191,772 patients with NSTEMI. Patients with CS (present on admission or developing during hospitalization) were then identified using ICD-9-CM code 785.51 (n = 53,800). Validation studies have shown a specificity of 99.3%, a sensitivity of 59.8%, a positive predictive value of 78.8%, and a negative predictive value of 98.1% for the ICD-9-CM code 785.51 to identify CS. We used ICD-9-CM procedure codes to identify patients who underwent coronary angiography, PCI, and CABG ( Supplementary Table 1 ). Invasive strategy was defined as coronary angiography with or without PCI or CABG. Patients who underwent both PCI and CABG during the hospitalization (n = 7,560) were included in the PCI group as this was likely the initial intended therapy in these patients.
Our primary outcome of interest was all-cause in-hospital mortality, defined as death during the hospitalization encounter in the NIS database. The LOS and total hospital cost were used as secondary outcomes. Total hospital charges provided in the NIS were converted to costs using the Healthcare Cost and Utilization Project cost-to-charge ratio files. The costs were inflation-adjusted using the Consumer Price Index provided by the US Bureau of Labor Statistics and are reported in 2015 US dollars. Data on costs were missing for 118,548 records. Therefore, results of cost analyses are based on a sample size of 2,073,225 patients.
Baseline patient characteristics such as demographics (age, gender, and race), primary expected payer, weekday versus weekend admission, median household income for patient’s ZIP code, 29 Elixhauser co-morbidities as defined by the Agency of Healthcare Research and Quality, and other clinically relevant co-morbidities (smoking, dyslipidemia, known coronary artery disease [CAD], family history of CAD, previous myocardial infarction, previous PCI, previous CABG, carotid artery disease, dementia, and atrial fibrillation) were included. A list of ICD-9-CM and Clinical Classifications Software codes used to identify co-morbidities is provided in Supplementary Table 1 . We also included hospital characteristics such as location (rural vs urban), region (Northeast, Midwest, South, and West), bed size (small, medium, and large), and teaching status.
Weighted estimates were used for all statistical analyses. For descriptive analyses, we used Pearson’s chi-square test for categorical variables, and the Student t test for continuous variables. In addition, we used standardized differences to compare patient and hospital characteristics between study groups. Compared with traditional significance testing, standardized differences are not as sensitive to sample size and are useful in identifying clinically meaningful differences. An absolute standardized difference of >10% was considered clinically meaningful. For trend analyses, we used the Cochrane–Armitage test for categorical variables and linear regression for continuous variables. To examine differences in in-hospital mortality, multivariate logistic regression models were constructed using generalized estimating equations with exchangeable working correlation matrix to account for clustering of outcomes within hospitals. The regression models adjusted for demographics, hospital characteristics, and all Elixhauser and other clinically relevant co-morbidities. Risk-adjusted mortality rates were calculated according to previously described methods. For analyzing temporal trends, the independent variable “YEAR” was entered in the regression models as a continuous variable to obtain unadjusted and adjusted odds ratio (OR) per year. Similarly, multivariate linear regression models were used to determine differences and trends in LOS and total hospital costs. Because LOS and total hospital cost had a positively skewed distribution, we used logarithmic transformation of LOS and cost as the dependent variable in the regression models.
We performed sensitivity analyses to further explore the association of an invasive treatment strategy with in-hospital mortality in patients with NSTEMI and CS. Patients who die early during hospitalization may not have sufficient time to undergo coronary angiography and/or revascularization. Furthermore, elderly patients and those with chronic kidney disease (CKD) are often less likely to undergo coronary angiography, and have higher mortality. We, therefore, repeated the multivariate logistic regression analyses comparing in-hospital mortality in patients with CS managed using an invasive versus conservative strategy after excluding patients who died on the day of admission (n = 1,736), and after further excluding patients aged ≥75 years and/or those with CKD (n = 31,203).
Statistical analysis was performed using IBM SPSS Statistics 20.0 (IBM Corp., Armonk, New York). All p values were 2-sided with a significance threshold of p <0.05. Categorical variables are expressed as percentage and continuous variables as mean ± SD. OR and 95% confidence interval (CI) are used to report the results of logistic regression analyses.
Results
From 2006 to 2012, of 2,191,772 patients with NSTEMI, 53,800 (2.5%) had a diagnosis of CS. Compared to patients with NSTEMI without CS, those with CS were older and more likely to be admitted to large, urban, teaching hospitals in the West ( Table 1 ). Patients with NSTEMI and CS were less likely to be smokers, less likely to have dyslipidemia, CAD, family history of CAD, previous PCI, previous CABG, hypertension, and more likely to have congestive heart failure, peripheral vascular disease, diabetes mellitus with complications, deficiency anemia, fluid and electrolyte disorder, weight loss, CKD, and valvular heart disease compared to those without CS ( Table 1 ). Of note, previous myocardial infarction was slightly more prevalent in patients without CS.
| Variable | Cardiogenic Shock | P value | Absolute Standardized Difference | |
|---|---|---|---|---|
| No (n=2,137,972) | Yes (n=53,800) | |||
| Age (years), mean ± standard deviation | 69.7 ± 14.4 | 72.0 ± 12.6 | <0.001 | 17.1 |
| Women | 43.7% | 40.4% | <0.001 | 6.6 |
| White | 63.4% | 63.8% | <0.001 | 0.8 |
| Black | 9.7% | 8.0% | 5.9 | |
| Hispanic | 6.6% | 8.2% | 6.1 | |
| Asian or Pacific Islander | 1.9% | 3.0% | 7.1 | |
| Native American | 0.5% | 0.6% | 1.7 | |
| Other | 2.4% | 3.1% | 4.2 | |
| Unknown | 15.5% | 13.3% | 6.3 | |
| Primary expected payer | <0.001 | |||
| Medicare | 63.1% | 69.3% | 13.3 | |
| Medicaid | 5.6% | 6.1% | 2.2 | |
| Private insurance | 23.6% | 18.0% | 13.8 | |
| Uninsured | 5.3% | 4.3% | 4.6 | |
| Other | 2.4% | 2.3% | 0.9 | |
| Weekend admission | 26.6% | 26.4% | 0.577 | 0.2 |
| Median household income (percentile) | <0.001 | |||
| 0-25 th | 28.3% | 27.6% | 1.5 | |
| 26 th -50 th | 26.6% | 25.8% | 1.9 | |
| 51 st -75 th | 24.3% | 25.5% | 2.7 | |
| 76 th -100 th | 20.7% | 21.1% | 0.9 | |
| Hospital characteristics | ||||
| Number of beds | <0.001 | |||
| Small | 10.4% | 8.1% | 8.1 | |
| Medium | 24.8% | 22.1% | 6.3 | |
| Large | 64.7% | 69.8% | 10.9 | |
| Urban location | 89.1% | 93.0% | <0.001 | 13.9 |
| Teaching hospital | 44.2% | 49.6% | <0.001 | 10.8 |
| Region | <0.001 | |||
| Northeast | 19.5% | 17.8% | 4.5 | |
| Midwest | 22.7% | 21.6% | 2.5 | |
| South | 40.8% | 38.9% | 4.0 | |
| West | 17.0% | 21.7% | 12.0 | |
| Comorbidities | ||||
| Smoker | 30.7% | 21.6% | <0.001 | 20.9 |
| Dyslipidemia | 55.7% | 38.7% | <0.001 | 34.4 |
| Coronary artery disease | 73.2% | 67.2% | <0.001 | 13.2 |
| Family history of coronary artery disease | 6.8% | 2.8% | <0.001 | 19.1 |
| Prior myocardial infarction | 11.8% | 9.9% | <0.001 | 6.2 |
| Prior percutaneous coronary intervention | 12.5% | 7.8% | <0.001 | 15.7 |
| Prior coronary artery bypass grafting | 9.9% | 7.0% | <0.001 | 10.4 |
| Carotid artery disease | 2.2% | 1.9% | <0.001 | 1.7 |
| Dementia | 7.8% | 6.5% | <0.001 | 0.1 |
| Atrial fibrillation | 18.3% | 27.4% | <0.001 | 0.3 |
| Acquired immune deficiency syndrome | 0.2% | 0.2% | <0.001 | 1.8 |
| Alcohol abuse | 2.6% | 3.7% | <0.001 | 6.2 |
| Deficiency anemia | 18.3% | 24.9% | <0.001 | 16.1 |
| Rheumatoid arthritis/collagen vascular diseases | 2.3% | 1.9% | <0.001 | 3.3 |
| Chronic blood loss anemia | 1.3% | 1.9% | <0.001 | 4.8 |
| Congestive heart failure | 35.1% | 67.6% | <0.001 | 68.7 |
| Chronic pulmonary disease | 23.1% | 26.2% | <0.001 | 7.2 |
| Coagulopathy | 4.2% | 15.1% | <0.001 | 37.5 |
| Depression | 7.3% | 5.5% | <0.001 | 7.3 |
| Diabetes mellitus (uncomplicated) | 30.2% | 30.1% | 0.507 | 0.3 |
| Diabetes mellitus (complicated) | 7.3% | 9.9% | <0.001 | 9.3 |
| Drug abuse | 2.0% | 1.5% | <0.001 | 3.8 |
| Hypertension | 70.7% | 59.0% | <0.001 | 24.8 |
| Hypothyroidism | 11.4% | 10.1% | <0.001 | 4.0 |
| Liver disease | 1.3% | 2.1% | <0.001 | 6.0 |
| Lymphoma | 0.6% | 0.7% | <0.001 | 2.0 |
| Fluid and electrolyte disorder | 21.2% | 48.4% | <0.001 | 59.7 |
| Metastatic cancer | 1.0% | 1.2% | <0.001 | 2.0 |
| Other neurological disorders | 6.8% | 7.8% | <0.001 | 3.9 |
| Obesity ∗ | 11.9% | 10.0% | <0.001 | 6.1 |
| Paralysis | 2.0% | 2.8% | <0.001 | 5.5 |
| Peripheral vascular disease | 12.5% | 16.1% | <0.001 | 10.4 |
| Psychoses | 2.3% | 2.3% | 0.542 | 0.3 |
| Pulmonary circulation disorders | 0.1% | 0.5% | <0.001 | 6.6 |
| Chronic kidney disease | 22.1% | 32.6% | <0.001 | 23.7 |
| Solid tumor without metastasis | 1.6% | 1.8% | 0.003 | 1.3 |
| Peptic ulcer (non-bleeding) | <0.1% | <0.1% | 0.535 | 0.3 |
| Valvular disease | 0.2% | 1.0% | <0.001 | 10.8 |
| Weight loss | 2.4% | 8.2% | <0.001 | 26.2 |
∗ Obesity was defined using the International Classification of Diseases, Ninth Edition, Clinical Modification codes as specified in the Elixhauser co-morbidities.
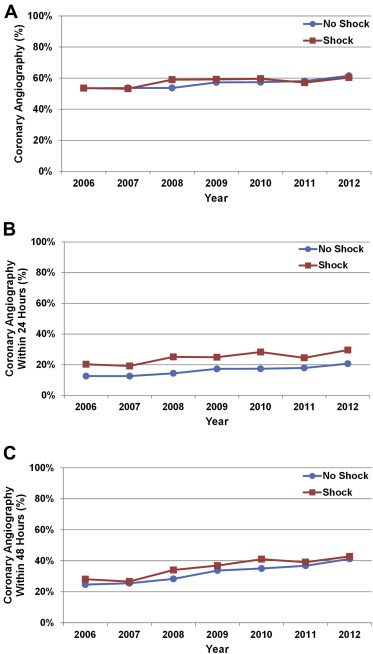
Utilization of coronary angiography in patients with NSTEMI and CS increased from 2006 to 2012 (p trend <0.001; Figure 1 ). Similar trend was seen in patients with NSTEMI without CS. Coronary angiography rates were higher in patients with CS compared to those without CS (57.8% vs 56.5%, p <0.001); however, this difference was not clinically meaningful (absolute standardized difference = 2.5). Rates of early coronary angiography were significantly higher in patients with CS compared to those without CS (within 48 hours: 36.4% vs 32.3%, p <0.001, absolute standardized difference = 8.6; within 24 hours: 25.0% vs 16.2%, p <0.001, absolute standardized difference = 21.9). Of note, in patients with NSTEMI and CS who were aged ≥75 years, the coronary angiography rate was 43.3% as compared with 69.2% in those aged <75 years (p <0.001).
Patients with NSTEMI and CS who underwent coronary angiography were younger, less likely to be women, and more likely to have private insurance compared to those who did not undergo coronary angiography ( Supplementary Table 2 ). Patients with CS who underwent coronary angiography had a higher prevalence of smoking, dyslipidemia, obesity, known CAD, and family history of CAD, and a lower prevalence of CKD, history of CABG, dementia, metastatic cancer, and other neurologic disorders.
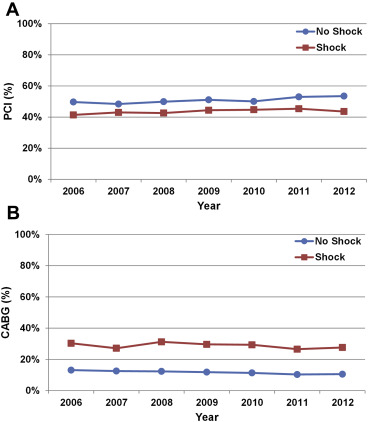
From 2006 to 2012, there was an increase in PCI rates and decrease in CABG rates in patients with NSTEMI and CS who underwent coronary angiography during hospitalization (p trend <0.001; Figure 2 ). Revascularization rates were significantly higher in those with CS versus without CS (72.5% vs 62.6%, p <0.001). Patients with CS aged ≥75 years were less likely to undergo revascularization compared to those aged <75 years (69.4% vs 73.9%, p <0.001). Compared to patients without CS, those with CS were less likely to undergo PCI and more likely to undergo CABG ( Figure 3 ).
In patients with CS, baseline characteristics were comparable between those who did or did not undergo revascularization, except for some minor differences ( Supplementary Table 3 ). Most notably, patients with CS who underwent revascularization were less likely to be women and more likely to have private insurance.
In-hospital mortality rate was significantly higher in patients with CS compared to those without CS (34.6% vs 3.6%; unadjusted OR 14.20, 95% CI 13.93 to 14.47; adjusted OR 10.09, 95% CI 9.88 to 10.32, p <0.001). In patients with NSTEMI and CS, utilization of an invasive strategy was associated with significantly lower in-hospital mortality as compared to a conservative strategy (24.8% vs 48.0%; unadjusted OR 0.36, 95% CI 0.34 to 0.37, adjusted OR 0.43, 95% CI 0.42 to 0.45, p <0.001). Similar results were seen in various subgroups of patients with CS ( Supplementary Table 4 ). Interestingly, compared to patients with CS managed using a conservative strategy, those who received coronary angiography alone (without revascularization) had a lower in-hospital mortality rate (34.5% vs 48.0%; unadjusted OR 0.57, 95% CI 0.54 to 0.60; adjusted OR 0.67, 95% CI 0.63 to 0.71, p <0.001). Nonetheless, the association between an invasive strategy and lower in-hospital mortality was strongest in patients with CS who underwent coronary angiography and revascularization (21.1% vs 48.0%; unadjusted OR 0.29, 95% CI 0.28 to 0.30; adjusted OR 0.35, 95% CI 0.33 to 0.36, p <0.001 as compared with conservative group).
Sensitivity analyses showed a persistent significant association between an invasive treatment strategy and lower risk-adjusted in-hospital mortality in patients with NSTEMI and CS after excluding patients who died on the day of admission (adjusted OR 0.45, 95% CI 0.43 to 0.47, p <0.001), as well as after further excluding patients aged ≥75 years and/or those with CKD (adjusted OR 0.37, 95% CI 0.34 to 0.40, p <0.001).
From 2006 to 2012, there was a significant decrease in in-hospital mortality in patients with and without CS ( Table 2 ). Patients with NSTEMI and CS managed using an invasive strategy showed the greatest temporal decrease in risk-adjusted in-hospital mortality during the study period ( Table 2 ; Figure 4 ).
| Cardiogenic Shock | Overall | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | Unadjusted OR Per Year (95% CI) | Adjusted OR Per Year (95% CI) |
|---|---|---|---|---|---|---|---|---|---|---|
| No | 3.6% | 4.1% | 3.9% | 4.0% | 3.5% | 3.4% | 3.2% | 3.2% | 0.954 (0.950-0.957) | 0.993 (0.989-0.997) |
| Conservative | 6.6% | 7.2% | 6.6% | 6.9% | 6.4% | 6.3% | 6.0% | 6.5% | 0.977 (0.973-0.981) | 1.002 (0.998-1.007) |
| Invasive | 1.3% | 1.4% | 1.5% | 1.5% | 1.3% | 1.2% | 1.1% | 1.2% | 0.955 (0.948-0.962) | 0.982 (0.974-0.991) |
| Yes | 34.6% | 40.8% | 40.3% | 33.2% | 33.6% | 32.3% | 32.7% | 32.7% | 0.944 (0.935-0.952) | 0.966 (0.956-0.975) |
| Conservative | 48.0% | 53.1% | 48.6% | 46.6% | 46.3% | 46.2% | 46.8% | 49.1% | 0.981 (0.968-0.994) | 0.997 (0.983-1.012) |
| Invasive | 24.8% | 30.1% | 33.0% | 23.9% | 24.8% | 22.8% | 22.1% | 21.9% | 0.921 (0.909-0.933) | 0.924 (0.911-0.938) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


