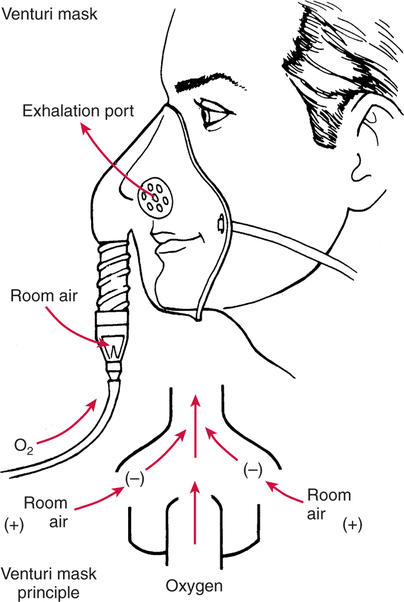
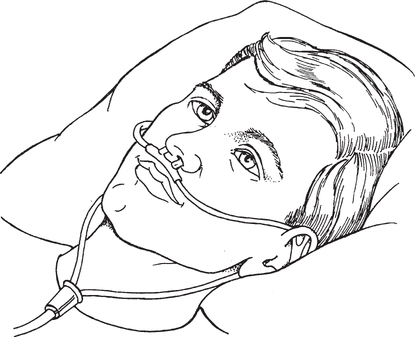
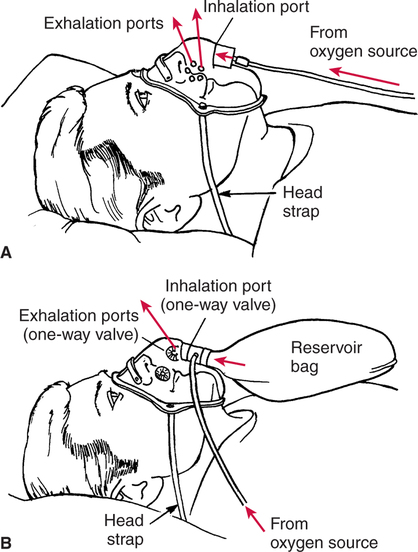
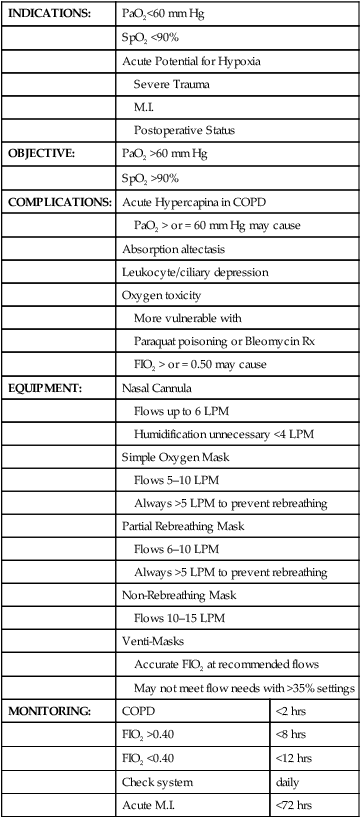
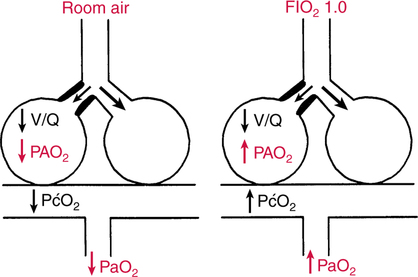
In clinical practice, moderate hypoxemia is usually corrected, which minimizes the compensatory stress placed on the cardiovascular system and ensures that hypoxia does not occur. Although mild hypoxemia (PaO2 60 to 79 mm Hg) is generally not associated with hypoxia, oxygen therapy may be used to minimize the strain on the cardiopulmonary system and to make the patient more comfortable. Notwithstanding, liberal use of oxygen therapy has recently been challenged.696 It has been purported that oxygen administration may delay application of appropriate respiratory care.696 The types of palliative therapy commonly used for acute PaO2 support are shown in Box 10-1. The most appropriate measures for a particular patient depend on the specific nature of the oxygen-loading problem. For example, when hypoxemia results from severe hypoventilation, mechanical ventilation will likely be necessary. On the other hand, when the hypoxemic mechanism is predominantly relative shunting, oxygen therapy may be all that is needed. Finally, with substantial absolute capillary shunting, therapy with positive end-expiratory pressure or continuous positive airway pressure (PEEP/CPAP) and/or alveolar recruitment maneuvers will probably be necessary. The effectiveness of oxygen therapy in relieving hypoxemia depends primarily on the nature of the mechanism responsible for the hypoxemia in the first place. For example, oxygen therapy is very effective in reversing the hypoxemia caused by relative shunting. As illustrated in Figure 10-1, relative shunts are alveolar-capillary units that have low but finite ventilation- perfusion ratios. The gas exchange problem in these units is that the quantity of oxygen available is insufficient (i.e., decreased partial pressure of alveolar oxygen [PAO2]) to oxygenate completely the volume of blood perfusing them. The effectiveness of oxygen therapy is related to its effects on alveolar-capillary units with low V/Q ratios. Administration of oxygen increases the alveolar oxygen supply and partial pressure in these units (see Fig. 10-1). It should be understood that the administration of oxygen does not change the ventilation-perfusion ratio or improve lung function. Nevertheless, despite low ventilation with respect to perfusion, alveolar oxygen delivery and PaO2 are increased. Oxygen therapy is also effective in the presence of diffusion defects. The increased PAO2 associated with oxygen therapy increases the driving pressure of oxygen across the alveolar-capillary membrane and thereby speeds up equilibration. Pulmonary diffusion is discussed in detail in Chapter 6. High-flow systems, sometimes referred to as fixed performance systems, are defined as oxygen administration devices that provide gas flow rates that are high enough to completely satisfy the patient’s inspiratory demand.298 Ventilators and low fraction of inspired oxygen (FIO2) air-entrainment masks (Fig. 10-2) are examples of high-flow systems. High-flow systems offer the advantage of delivering accurate, controlled levels of FIO2. Furthermore, they often provide control of temperature and humidity of the inspired gas. A disadvantage of high-flow systems is that they are often noisy, bulky, and uncomfortable. Low-flow systems, sometimes referred to as variable performance systems, supply oxygen at flow rates that are less than the patient’s inspiratory flow demand. The specific level of FIO2 delivered may be high or low. Examples include the nasal cannula (Fig. 10-3), the simple mask (Fig. 10-4,A), and partial and non-rebreathing masks. A non-rebreathing mask is shown in Figure 10-4,B. Advantages of low-flow systems include simplicity and patient tolerance. A disadvantage is that control of FIO2 levels with low-flow systems is less precise, because levels may vary with changes in ventilatory pattern. The approximate levels of FIO2 that are delivered with a specific apparatus set on a given flow rate are shown in Table 10-1. One must remember, however, that these approximations apply only to individuals with a normal breathing pattern (e.g., tidal volume ≅ 500 mL, respiratory rate ≅ 12 breaths per minute). When a patient breathes more rapidly or deeper than normal, the actual FIO2 level delivered is less than that shown in Table 10-1. Conversely, with slow, shallow ventilation, FIO2 levels may be much higher than those shown in Table 10-1. Table 10-1 Approximate FIO2 Levels with Low-Flow Devices Adapted from Ziment, I.: Respiratory Pharmacology and Therapeutics. Philadelphia, W.B. Saunders, 1978. Non-rebreathing masks that incorporate one-way valves to prevent inspiration of room air have been traditionally thought to provide a higher FIO2 (i.e., 0.6 to 0.8) than partial rebreathing masks (i.e., 0.4 to 0.7).302 There is some evidence to suggest only very minimal FIO2 differences between these two types of masks under normal clinical circumstances.303 698 699 It is interesting to note that, as a variable system, FIO2 delivered via a nasal cannula could theoretically increase from 0.44 at a tidal volume of 500 mL, to 0.68 if tidal volume fell to 250 mL.10 Therefore, it must not be assumed that low flow rates of oxygen from devices such as nasal cannulas always deliver low FIO2 levels. One must always keep in mind the effects of breathing pattern on FIO2 when using low-flow oxygen administration systems. To further complicate matters, there is evidence to suggest that oxygen concentration may be higher during nasal breathing versus mouth breathing when using nasal cannulas,315 although this finding is controversial.302 Despite the fact that high-flow systems are more accurate and that their use is advocated by some clinicians,300 low-flow systems have more widespread use because of their simplicity and comfort. Recommendations by the American Association for Respiratory Care302 as well as the American College of Chest Physicians and the National Heart and Blood Institute state that oxygen therapy should be used when PaO2 is less than 60 mm Hg or SaO2 is less than 90%.298 A summary of key recommendations for oxygen therapy in the acute care hospital are shown in Box 10-2. Box 10-3 outlines key factors to consider when applying oxygen therapy in preterms and neonates.302 304 For example, oxygen therapy may be deemed beneficial if it is accompanied by an improving blood pressure or heart rate even if the PaO2 failed to increase significantly. As stated by Campbell, “Oxygen therapy is too serious to be left to electrodes alone.”297 Evaluation of the need for oxygen must include an assessment of the entire cardiopulmonary system as well as complete hypoxic assessment as discussed in Chapter 11. It is noteworthy that analysis of arterial blood gases is not always indicated simply because oxygen is being briefly administered. The cost of arterial blood analysis may outweigh its benefit, particularly in short-term therapy.298 The price of one blood gas analysis may exceed the cost of 24 to 48 hours of oxygen therapy. In many cases, pulse oximetry can serve as a cost-effective alternative to arterial blood gas analysis for monitoring oxygen therapy. In the absence of chronic obstructive pulmonary disease (COPD), chronic CO2 retention, or acute severe asthma,700 oxygen therapy may be administered without concern for inducing hypoventilation. It has been said that “the brain softens before the lung hardens,” in reference to the reluctance of clinicians to administer oxygen for fear of oxygen toxicity. Oxygen therapy must not be withheld in the case of a patient who may be hypoxic. When PaO2 falls below 55 mm Hg acutely, short-term memory is altered and euphoria or impaired judgment may be observed.298 Therefore, in most clinical situations the PaO2 should be targeted to 60 to 80 mm Hg. The approach to oxygen therapy in the patient with COPD, acute severe asthma,700 or chronic hypercapnia is completely different. In these individuals, caution is the byword. Excessive oxygen therapy administered to these oxygen- sensitive patients could potentially have fatal consequences. Nevertheless, even in these patients, when hypoxia is suspected, oxygen therapy should never be withheld simply because the patient may be sensitive to oxygen. Correction of hypoxia is always the first priority. Specifically, the first line of supportive treatment in acute exacerbation of COPD is low FIO2 therapy. Typically, the patient with COPD in acute respiratory failure has blood gases approximating those shown in Example 10-1.300 Despite PaCO2 levels in excess of 60 to 65 mm Hg, many patients with COPD can be treated without mechanical ventilation.306 In general, mechanical ventilation should not be initiated unless pH falls below 7.20297 306 and after all else fails.297 307 The decision to institute mechanical ventilation in COPD is always difficult and requires consideration of a host of variables. A reasonable target PaO2 in acute exacerbation of COPD is 60 mm Hg.308 This level guards against hypoxia and is unlikely to cause substantial hypercapnia and acidosis. A useful guideline for FIO2 selection in acute exacerbation of COPD is the fact that PaO2 increases approximately 3 mm Hg for each 0.01 increase in FIO2.300 309 Thus, if a patient with COPD is seen in the emergency department during an acute exacerbation with a PaO2 of 39 mm Hg on FIO2 of 0.21, the FIO2 level indicated to achieve a PaO2 of 60 mm Hg is 0.28. In other words, an FIO2 increase of 0.07 should increase PaO2 approximately 21 mm Hg (7 × 3 mm Hg). The formula shown in Equation 10-1 may be used to determine the appropriate percentage of oxygen to be applied in acute exacerbation of COPD, assuming a target PaO2 of 60 mm Hg. Of course, this is just a guideline, and individual cases may vary considerably. It must also be remembered that this guideline applies only to the patient with COPD in acute exacerbation.It should also be noted that when in doubt it is probably wise to administer more oxygen rather than less.
Treatment of Hypoxemia and Shunting
TREATMENT
Acute Hypoxemia
OXYGEN THERAPY
Mechanism of Effectiveness
Relative Shunting
Diffusion Defects
Oxygen Administration Devices
High-Flow Systems
Low-Flow Systems
Device
Flow (L/min)
FIO2
Nasal Cannula
1
0.24
2
0.28
3
0.32
4
0.36
5
0.40
6
0.44
Simple mask
6
0.40
7
0.50
8
0.60
Partial rebreathing mask
6–10
0.60
Oxygen Therapy in the Spontaneously Breathing Patient
Goals in Oxygen Therapy
Clinical Approach to Oxygen Therapy
Non–Oxygen-Sensitive Patients
Oxygen-Sensitive Patients
Example 10-1
pH
7.23-7.39
PaCO2
60-80 mm Hg
PaO2
∼ 40 mm Hg
FIO2 Selection
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Treatment of Hypoxemia and Shunting
60 mm Hg − room air PaO2/3 = required % FIO2 increase Equation 10-1
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue

 /
/ and thus corrects this form of hypoxemia.
and thus corrects this form of hypoxemia.