When a sudden, complete occlusion of a coronary artery prevents blood flow from reaching an area of myocardium, the resulting transmural myocardial ischemia4–6 is manifested by deviation of the ST segment toward the involved region. This is shown in the ECG of a patient before, during, and after receiving brief therapeutic balloon occlusion with percutaneous transluminal coronary angioplasty (Fig. 11.2A–C). The ST-segment changes typically disappear abruptly when coronary blood flow is restored by deflating the angioplasty balloon after a brief period. This indicates that the myocardial cells have been reversibly ischemic and have not actually become infarcted.
It may be difficult to differentiate the abnormal changes in the ST segment produced by transmural myocardial ischemia from variations of normal, particularly when the deviation of the ST segment is minimal. Presence of one of the following criteria is typically required for the diagnosis of transmural myocardial ischemia7:
1. Elevation of the origin of the ST segment at its junction (J point) with the QRS complex in two or more leads of:
• 0.1 mV (1 mm) in any lead except for leads V2 and V3
• in leads V2 and V3 ST-J elevation should be:
a. 0.25 mV (2.5 mm) in men less than 40 years of age
b. 0.20 mV (2.0 mm) in men 40 years of age or older
c. 0.15 mV (1.5 mm) in women of any age.
2. Depression of the origin of the ST segment at the J point of 0.10 mV (1 mm) in two or more of leads V1-V3.
A greater threshold is required for ST-segment elevation in leads V2 to V3 because a normal, slight elevation of the ST segment is often present (see Fig. 3.12). In addition, younger men are most likely to have “normal” ST elevation in leads V2 to V3, which is the reason for different thresholds by age and gender.
When the amplitude and duration of the terminal S wave is further increased in leads V1 to V3 as a result of left-ventricular dilation (see Fig. 5.8) or left-bundle-branch block (LBBB) (Fig. 11.3), an even greater “normal” elevation of the ST segment is typically present. A study has shown that elevation of the ST segment to ≥0.5 mV is required in leads V1 to V3 to diagnose acute anterior transmural myocardial ischemia in the presence of LBBB.8 This and other electrocardiographic criteria are presented in Table 11.1. However, the 0.1-mV threshold remains applicable for diagnosis of acute transmural ischemia when the deviation of the ST segment is in the same direction (concordant with) as that of the terminal QRS waveform.
Various positions along the ST segment are sometimes selected for measuring the amount of deviation from the horizontal PR-TP baseline. Measurement of ST-segment deviation is either for establishing the diagnosis of transmural myocardial ischemia or for estimating its extent. “J” and “J + 0.08 second” have been used in some clinical situations (Fig. 11.4). The deviated ST segment may be horizontal (see Fig. 11.4A), downsloping (see Fig. 11.4B), or upsloping (see Fig. 11.4C). The sloping produces different amounts of deviation of the ST segment as it moves from the J point toward the T wave. Note that the J point is more elevated than the J + 0.08-second point in Figure 11.4B, equally elevated in Figure 11.4A, and less elevated in Figure 11.4C. The ECG criteria for ST-elevation myocardial infarction (STEMI) may be accompanied by other manifestations of insufficient myocardial perfusion, such as typical or atypical precordial pain, decreased blood pressure, or cardiac arrhythmias.
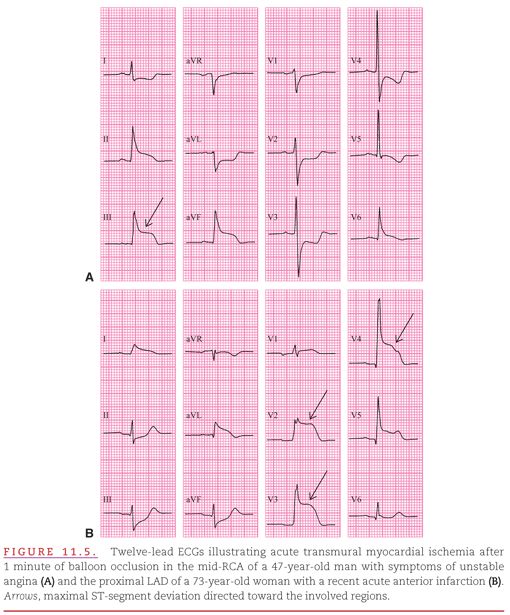
Because the ST-segment axis in transmural myocardial ischemia deviates toward the involved area of myocardium, the changes described appear positive or elevated in leads with their positive poles pointing toward ischemic inferior (Fig. 11.5A) or anterior (see Fig. 11.5B) aspects of the left ventricle (LV). Often, both ST-segment elevation and depression appear in different leads of a standard 12-lead ECG. Usually, the direction of greater deviation should be considered primary and the direction of lesser deviation should be considered secondary or reciprocal. When transmural myocardial ischemia involves both inferior and lateral aspects of the LV, the ST-segment depression of lateral involvement in leads V1 to V3 may equal or exceed the elevation produced by inferior involvement in leads II, III, and aVF.
As when considering a map of the earth, these “Mercator” views provide a planar perspective of the spatial relationships of the anatomy and pathology to the basal, middle, and apical segments of the four quadrants or “walls” of the LV in Figure 11.6.9 The LV is typically divided into septal, anterior, lateral, and inferior quadrants. Distributions of the major coronary arteries (left coronary artery [LCA], left anterior descending [LAD] coronary artery, left circumflex artery [LCX], right coronary artery [RCA], and the posterior descending artery [PDA]; see Fig. 11.6, top) are related to the distributions of insufficient blood supply resulting from occlusions of the respective arteries (see Fig. 11.6, bottom).
Transmural myocardial ischemia most commonly occurs in the distal aspect of the area of the left-ventricular myocardium supplied by one of the three major coronary arteries. Note that involvement of basal and middle segments of the lateral quadrant may be due to occlusion of the proximal LCX or a large (marginal) branch. The relationship between seven culprit areas in the three coronary arteries and the leads commonly with ST elevation or depression are shown in Table 11.2.
In about 90% of individuals, the PDA originates from the RCA, and the LCX supplies only part of a single left-ventricular quadrant. This has been termed right coronary dominance. In the other 10% of individuals with left coronary dominance, the PDA originates from the LCX, and the RCA supplies only the right ventricle.
The basal and middle sectors of the lateral quadrant of the LV typically supplied by the LCX and its branches are located distant from the positive poles of all 12 of the standard ECG leads. Therefore, occlusion of the LCX is typically indicated by ST-segment depression rather than elevation (Fig. 11.7). Note that no ST-segment elevation is present in any standard lead. Consideration of the mirror-lake image obtained by viewing the recording upside down and backward, or placement of additional leads on the posterior–lateral thorax would be required to visualize ST-segment elevation due to transmural myocardial ischemia in this area.10
Transmural myocardial ischemia may also involve the thinner walled right-ventricular myocardium when its blood supply via the RCA becomes insufficient. Right-ventricular transmural myocardial ischemia is represented on the standard ECG as ST-segment elevation in lead V1 greater than V2 (Fig. 11.8
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


