Transesophageal and Intracardiac Echocardiography
Jae K. Oh
Donald J. Hagler
Allison Cabalka
Guy S. Reeder
Frank Cetta Jr
James B. Seward
Transesophageal Echocardiography
In 1987, clinical transesophageal echocardiography (TEE) was introduced at Mayo Clinic Rochester (1). This technology has inexorably changed the diagnostic strategy for numerous cardiovascular diseases and, in many circumstances, has become the diagnostic procedure of choice. The principal reason for this change in practice is that TEE provides superb clarity and resolution and easily interpretable images, which are uniquely suited to the clinical circumstance. After some initial trepidation, it is now appreciated that TEE is a procedure that is relatively easy to perform, uncomplicated, and capable of providing unique insight into cardiothoracic structures, even in critically ill patients. TEE incorporates all the functionality of transthoracic echocardiography (TTE), including three-dimensional imaging, which can reliably interrogate cardiovascular anatomy, function, hemodynamics, and blood flow. Before the introduction of TEE, echocardiography was frequently used as a screening tool that had to be complemented by other diagnostic modalities. Currently, definitive management of valvular disease, aortic dissection, endocarditis, atrial fibrillation, congenital heart disease, and intracardiac masses and tumors can be accomplished on the basis of a complete echocardiography examination, including TEE (2, 3, 4, 5). In this clinical context, TEE will continue to have a major role in the management of virtually all cardiovascular diseases. Approximately 5% to 10% of patients who have a TTE examination require the addition of TEE. Also, TEE has become an integral part of cardiovascular surgery for identifying a previously unrecognized abnormality that may affect the surgical procedure or the patient’s outcome and for assessing the result of the operation (see Chapter 21). As in the first two editions of The Echo Manual, TEE is discussed throughout the text in relation to the diagnosis and management of specific cardiovascular diseases.
Indications
The indications for referral for 8,535 TEE procedures from September 2001 to July 2004 at Mayo Clinic Rochester are listed in Table 3-1. The distribution of indications for TEE varies from institution to institution, depending on the patient population. The most common indication has been for evaluation of a potential cardiac source of embolism (35%) and atrial fibrillation (34%). Besides these pervasive and somewhat controversial indications, TEE is now considered essential in the evaluation of the mitral valve lesions, left atrial (LA) or LA appendage thrombus, intracardiac mass, atrial septal defect (in particular, aortic dissection), and critically ill patients (6, 7, 8, 9, 10, 11). Because of 1) an increasing number of patients with atrial fibrillation, 2) a new practice model for TEE-guided cardioversion, and 3) ablation procedures, atrial fibrillation has become one of the more common reasons for referral for TEE.
Table 3-1 Indications for transesophageal echocardiography at Mayo Clinic Rochester from September 2001 to July 2004: 8,535 procedures | ||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Preparation and Potential Complications
TEE is a semi-invasive procedure that can be uncomfortable in unprepared patients. Patients should be informed about why TEE is performed, and the entire procedure should be explained, including rare side effects (<1%) or complications such as laryngospasm, transient throat pain, shortness of breath, methemoglobinemia, aspiration, hypotension, hypertension, tachycardia, esophageal rupture, and even the rare risk of death (12, 13, 14). For elective TEE, the patient should fast for at least 6 hours before the procedure. A history of clinically significant dysphagia or esophageal disease should be evaluated before TEE is performed (Table 3-2). If the patient has dentures, they should be removed. Every patient should have an intravenous access (preferably a three-way stopcock) for administration of a contrast agent or medications.
Immediately before intubation with the transesophageal probe, a local anesthetic spray is used to anesthetize the posterior pharynx. An excessive amount of locally administered lidocaine has been reported to cause central nervous system toxic effects in patients who have congestive heart failure or diminished liver function (15). Toxic methemoglobinemia also has been reported, particularly after the administration of benzocaine. Methemoglobin is the oxidized (Fe3+) form of hemoglobin that cannot carry oxygen. In normal red blood cells, it is a minor (1%) component of hemoglobin and is reduced to the ferrous (Fe2+) form of hemoglobin by cytochrome-b5 reductase. Benzocaine, an oxidizing agent, has been associated with serious methemoglobinemia. Patients with inherited lack of cytochrome-b5 reductase are at increased risk for the development of methemoglobinemia. The estimated incidence is 0.12% (13). Benzocaine should be applied as no more than two short (half-second) sprays (a 1-second spray of 20% benzocaine = 200 mg). The major manifestations of methemoglobinemia are central cyanosis and oxygen desaturation. Blood color is brown. A typical example is a methemoglobin level of 10% or more and oxygen desaturation. Treatment consists of methylene blue, 1 mg/kg of a 1% solution, administered over 5 minutes (13). Methylene blue should be available in the room where TEE is performed. Reversal of methemoglobin may take from several minutes to 2 to 3 days. In severe cases (>70% methemoglobin), exchange transfusion or dialysis may be needed.
A drying agent, glycopyrrolate (Robinul, 0.2 mg), can be used to minimize oral secretions and decrease the possibility of aspiration during the examination. Because glycopyrrolate is an atropine-like drug, it may increase heart rate, especially in patients with atrial fibrillation. A short-acting sedative or amnestic agent such a midazolam (Versed), 1 to 10 mg (mean dose, 3.6 ± 2.3 mg), and fentanyl, 25 to 100 mg intravenously, are used almost routinely to make the TEE examination more comfortable and accepted by the patient. These agents should be used with caution in debilitated or elderly patients because of potential respiratory suppression. However, midazolam can be rapidly reversed in about 60 seconds with flumazenil, 0.2 to 0.4 mg intravenously. In young patients, meperidine (Demerol), 25 to 50 mg, also may be used to help alleviate the gag reflex, relieve pain sensation, and enhance sedation. Prophylaxis for subacute bacterial endocarditis is not necessary or generally used even in patients with a prosthetic valve (16). Occasionally, it has been necessary to paralyze an agitated critically ill patient.
A nasogastric or endotracheal tube usually does not interfere substantially with esophageal intubation with the TEE probe or prohibit the acquisition of satisfactory images. Esophageal perforation is a rare but disastrous complication of TEE (12). TEE should not be performed in patients with dysphagia without further evaluation of the esophagus. Intubation of a TEE probe should not be forced. Prolonged intubation of a TEE probe during an operation may increase the risk of perforation. When the TEE probe is not used intraoperatively, it may be disconnected from the machine to reduce thermal injury. Also, the TEE probe should not be left in the esophagus or the stomach in a locked position.
Instrumentation
The TEE probe is a modified gastroesophageal endoscopy probe, typically with a 3- to 7-MHz ultrasound transducer at the tip. It can be maneuvered to various positions in the esophagus and stomach, from which the heart and other cardiovascular and surrounding structures can be visualized. The diameter of the adult transducer tip
is 9 to 14 mm, and this is miniaturized to less than 3 mm for pediatric and neonatal and even fetal use. All adult probes use multiplane transducers that can be rotated 180 degrees. The transducer usually is rotated by a finger-pressure–sensitive switch at the proximal operator end. The tip of the probe also can be anteflexed or retroflexed or moved side to side by larger knobs at the proximal end. When performed electively, the examination begins with the patient in the left lateral decubitus position. The procedure room is equipped with oral suction, oxygen supply, pulse oximeter, and cardiopulmonary resuscitation capabilities. In critically ill patients for whom transfer is difficult, the examination is performed at the bedside. If the patient is mechanically ventilated, the TEE probe is often introduced with the patient supine.
is 9 to 14 mm, and this is miniaturized to less than 3 mm for pediatric and neonatal and even fetal use. All adult probes use multiplane transducers that can be rotated 180 degrees. The transducer usually is rotated by a finger-pressure–sensitive switch at the proximal operator end. The tip of the probe also can be anteflexed or retroflexed or moved side to side by larger knobs at the proximal end. When performed electively, the examination begins with the patient in the left lateral decubitus position. The procedure room is equipped with oral suction, oxygen supply, pulse oximeter, and cardiopulmonary resuscitation capabilities. In critically ill patients for whom transfer is difficult, the examination is performed at the bedside. If the patient is mechanically ventilated, the TEE probe is often introduced with the patient supine.
Table 3-2 Preparation for transesophageal echocardiography | |
|---|---|
|
We use a bite guard to protect the TEE scope, unless the patient is edentulous. When the scope is introduced, the imaging surface of the transducer faces the tongue, which directs the ultrasound beam from the posteriorly located esophagus anteriorly toward the heart. A digital technique generally is used for esophageal intubation. When the probe is introduced, the posterior portion of the tongue is depressed with the left index finger to minimize tongue movement, and the tip of the transducer is placed over the left index finger to a position at the center of the tongue. After the transducer is in the correct position, the left index finger is placed over the distal shaft or tip of the probe and depressed directly downward onto the tongue. This places the tip of the probe in direct alignment with the posteriorly located esophagus and away from the anteriorly located trachea. The tip of the transducer is advanced smoothly and slowly posteriorly toward the esophagus. At this time, the patient is asked to swallow. The tip of the TEE transducer should be advanced into the esophagus without force or notable resistance. The distance from the incisors to the part of the esophagus behind the mid LA is approximately 30 cm.
Training of Physicians and the Role of Sonographers
TEE complements the TTE examination. Therefore, it is advised that a physician who performs TEE has competency
in TTE, which includes personally performing more than 300 documented surface echocardiograms before performing TEE. The physician also needs to learn the technique of esophageal intubation under the supervision of an endoscopist or other echocardiologist experienced in TEE procedure. We consider a minimum of 50 esophageal intubations necessary to provide adequate training in intubation.
in TTE, which includes personally performing more than 300 documented surface echocardiograms before performing TEE. The physician also needs to learn the technique of esophageal intubation under the supervision of an endoscopist or other echocardiologist experienced in TEE procedure. We consider a minimum of 50 esophageal intubations necessary to provide adequate training in intubation.
Table 3-3 Summary of the role of the sonographer/assistant in transesophageal echocardiography (TEE) | |
|---|---|
|
The sonographer or trained assistant has an essential role in preparing patients for TEE and in assisting the physician during the examination. The role of the sonographer or assistant in TEE is summarized in Table 3-3. In our laboratory, a registered nurse or nurse sonographer coordinates and assists with TEE examinations. Because TEE is semi-invasive, the skills of a registered nurse are preferred for closely monitoring the patient, that is, for obtaining vital signs, administering medications, inserting intravenous catheters, and using suction, oxygen, or other emergency equipment. A properly trained assistant can perform these functions except for intravenous administration of medications. Because TEE has a small but definite risk for the patient, it generally is considered necessary for the procedure to be performed by a physician. Also, physicians and allied health personnel involved in performing TEE are required to have annual training in conscious or moderate sedation.
Multiplane Transesophageal Echocardiography Imaging Views
The multiplane TEE transducer consists of a single array of crystals that can be rotated electronically or mechanically around the long axis of the ultrasound beam in an arc of 180 degrees (Fig. 3-1). With rotation of the transducer array, multiplane TEE produces a continuum of transverse and longitudinal image planes (17).
Multiplane images are identified by an icon to indicate the degree of transducer rotation (Fig. 3-2). This designation helps the operator to understand the orientation of the ultrasound beam and to conduct the TEE examination more efficiently. The transverse esophageal plane, which is in the short axis of the body, is designated as 0 degrees. The longitudinal esophageal plane, which is in the long axis of the body, is designated as 90 degrees. The TEE transducer can be rotated in a continuum throughout 180 degrees, resulting in versatility of the examination and ease of understanding. Normally, from the midesophagus, the short axis of the heart is imaged at 45 degrees of rotation and its long axis at 135 degrees.
Almost all views obtained with surface echocardiography can be duplicated by TEE. Because the same cardiovascular structures are imaged by both TTE and TEE, the anatomic correlations and image orientations should be consistent for both examinations. To replicate the identical transthoracic (TTE) image format, we usually keep the electronic transducer artifact of TEE predominantly at the bottom of the display screen throughout the TEE examination (17). However, if preferred, the opposite orientation, with the transducer at the top of screen, may also be used.
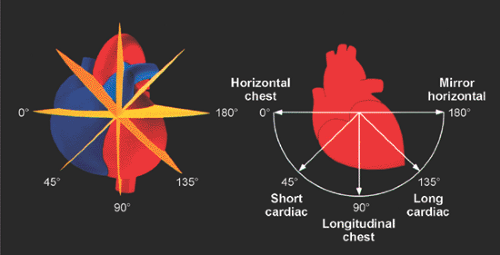 Figure 3-1 Array rotations of selected degrees (0, 45, 90, 135, and 180 degrees) permit a logical sequence of standard transducer orientations and resultant images. Such a display helps the examiner acquire the desired views:0-degree transverse orientation, which is horizontal to the chest at the midesophageal level; 45-degree short-axis orientation to the base of the heart from the midesophagus; 90-degree longitudinal orientation, which is in the sagittal plane of the body; 135-degree long-axis orientation to the heart from the midesophagus; and 180-degree rotation, which produces a mirror-image transverse plane. (From Seward et al [17]. Used with permission of Mayo Foundation for Medical Education and Research.) |
Primary Views
Four primary multiplane TEE views can be obtained (Fig. 3-3 and 3-4) by rotating the transducer array from 0 degrees to 135 degrees:1) 0 degrees (transverse plane):oblique view of basal structures; the four-chamber view or transgastric short-axis view can be obtained from this position by retroflexion and anteflexion of the transducer tip, respectively; 2) 45 degrees:short-axis view; this image is similar to the TTE parasternal short-axis view at the level of the aortic valve; 3) 90 degrees:longitudinal transducer orientation; this produces images oblique to the long axis of the heart; 4) 135 degrees:the true long axis of the LA and left ventricular outflow tract (LVOT); this is analogous to the parasternal long-axis view.
Longitudinal Views
With the transducer array at 90 degrees, the plane is sagittal to the body and oblique to the long axis of the heart. Sequential leftward (counterclockwise rotation) and rightward (clockwise rotation) rotations of the probe shaft will develop a series of longitudinal TEE views (Fig. 3-5 and 3-6). These views include the following:1) counterclockwise rotation of the scope, producing a two-chamber left ventricular (LV) inflow view; 2) slight rightward rotation of the scope from the first view, producing a long axis of the right ventricular outflow tract (RVOT); 3) further rightward rotation, producing a long-axis view of the proximal ascending aorta; and 4) still further rightward rotation of the scope, producing a long-axis view of the venae cavae and atrial septum.
 Figure 3-3 Primary multiplane transesophageal views (0, 45, 90, and 135 degrees) are obtained by rotating the array indicator from left to right on the icon. The transducer is in midesophagus. At 0 degrees (transverse plane), an oblique view of the basal structures, including the noncoronary (N) and right coronary (R) cusps of the aortic valve (AV), is obtained. At 45 degrees, a short-axis view of the basal structures, including the left coronary cusp (L) and N and R cusps of the AV, is obtained. At 90 degrees (longitudinal plane), a long-axis view of the basal cardiac structures, including the ascending aorta (Asc Ao), is obtained. At 135 degrees, the array is aligned with the long axis of the left ventricle (LV). LA, left atrium; LVO, left ventricular outflow; MPA, main pulmonary artery; RA, right atrium; RAA, right atrial appendage; RV, right ventricle; RVO, right ventricular outflow; TV, tricuspid valve; VS, ventricular septum. (From Seward et al [17]. Used with permission of Mayo Foundation for Medical Education and Research.) |
 Figure 3-4 Tomographic anatomy of the heart at midesophagus. The anatomic specimens have been cut to correspond to the echocardiographic images shown in Figure 3-3. Specimens are presented from the perspective of 0-degree rotation of the imaging array (left) to 135-degree rotation (right). In an oblique short-axis cut at the base of the heart (0-degree rotation), the esophagus (E) is posterior and adjacent to the left atrium (LA). The image array is in the short axis of the body, and, consequently, the cusps of the aortic valve (AV) are cut obliquely. Frequently, the LA appendage (LAA) and left upper (superior) (LUPV) and left lower (inferior) (LLPV) pulmonary veins are visualized in this short-axis view. The right atrium (RA) is to the viewer’s left; the right ventricular outflow (RVO) is anterior. In a short-axis view of the aortic valve (45-degree rotation), the AV cusps, left coronary (L), noncoronary (N), and right coronary (R), are optimally displayed. The descending thoracic aorta (Ao) is cut obliquely. The RVO is anterior, and the esophagus is posterior. In a longitudinal scan (90-degree rotation), the basal structures of the cardiac specimen, including the proximal ascending aorta (Asc Ao), are in the long axis of the body. The esophagus is posterior. A membranous atrial septum (arrowheads) and patent foramen ovale (arrow) are evident in this view. The right pulmonary artery (RPA) courses posterior to the ascending aorta. In a long-axis view of the LA (135-degree rotation) (identical to the parasternal long-axis view), the esophagus is posterior and adjacent to the LA. The AV, left ventricular outflow (LVO), and body of the left ventricle are viewed in the long axis. The RVO is anterior. In this tomographic cut, the view of the heart is from the left ventricle toward the ventricular septum (VS) and right ventricle. AS, atrial septum; B, bronchus; IVC, inferior vena cava; MV, mitral valve; PM, posteromedial papillary muscle; PV, pulmonary valve; RV, right ventricle; TS, transverse sinus (a pericardial space separating LA, RPA, Asc Ao, and RA); TV, tricuspid valve. (From Seward et al [17]. Used with permission of Mayo Foundation for Medical Education and Research.) |
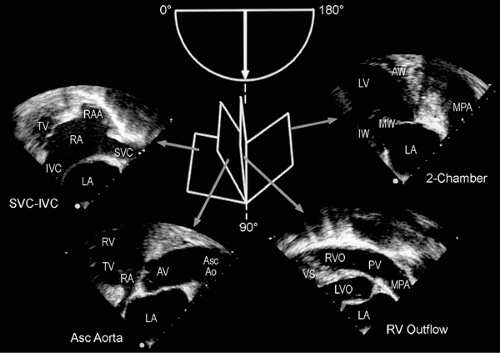 Figure 3-5 Series of longitudinal echocardiographic views obtained with the tip of the transducer in midesophagus. Rotation of the shaft of the scope to the patient’s left (counterclockwise rotation of the shaft) produces an optimal image of the mitral valve (MV) and left ventricular (LV) inflow. A sequence of longitudinal views is obtained by progressive rotation of the shaft of the scope to the patient’s right. (Note that the array is kept at 90 degrees throughout this maneuver.) The sequence presentation begins at the right in this illustration:1) a two-chamber LV inflow view is obtained with the scope rotated to the left; 2) right ventricular outflow (RVO) is depicted by a slight rightward rotation of the scope; 3) next, further rightward rotation (neutral position) results in a long-axis view of the proximal ascending aorta (Asc Ao); and 4) a long-axis view of the superior (SVC) and inferior (IVC) vena cava and atrial septum is obtained by further rightward rotation of the scope. AV, aortic valve; AW, anterior wall; IW, inferior wall; LA, left atrium; LVO, left ventricular outflow; MPA, main pulmonary artery; PV, pulmonary valve; RA, right atrium; RAA, right atrial appendage; TV, tricuspid valve; VS, ventricular septum. (From Seward et al [17]. Used with permission of Mayo Foundation for Medical Education and Research.) |
 Figure 3-6 Midesophageal longitudinal tomographic anatomic sections cut to correspond to the echocardiographic images in Figure 3-5. Anatomic views are described from the viewer’s right to left. In a two-chamber view, the esophagus is posterior to the left atrium (LA), which is the primary chamber visualized along with the left ventricle (LV). Mitral valve (MV) inflow is demonstrated best in this view. The LA appendage (LAA) is seen in the anterior LA. The view of the specimen is from the LV toward the chambers on the right side of the heart. In a long-axis view of right ventricular outflow (RVO), the section is oblique to the body of the heart but in the long axis of the RVO, pulmonary valve (PV), and proximal main pulmonary artery (MPA). The posteriorly located LA is adjacent to the esophagus. In a long-axis view of the proximal ascending aorta (Asc Ao), the LV and aortic valve (AV) are cut obliquely. This view is best for visualizing the membranous ventricular septum (VS and arrow). The right pulmonary artery (RPA) is posterior to the ascending aorta. In a long-axis view of the superior (SVC) and inferior (IVC) vena cava, the specimen is viewed from the left toward the free wall of the right atrium (RA). The right atrial appendage (RAA) is anterior in the RA cavity. The right pulmonary artery (RPA), transected in the short axis, courses posterior to SVC. The posteriorly located LA is adjacent to the esophagus. AS, atrial septum; AW, anterior wall; B, bronchus; Desc Ao, descending thoracic aorta; IW, inferior wall; LCA, left main coronary artery; LPA, left pulmonary artery; LVO, left ventricular outflow; Pul V, left inferior pulmonary vein; TS, transverse sinus; TV
Get Clinical Tree app for offline access
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


|
