Total Anomalous Venous Connection
In a total anomalous pulmonary venous connection, there is no direct continuity between the pulmonary veins and left atrium. For the neonate to survive there must be some mixing of circulation through a small atrial septal defect or a patent foramen ovale. The pulmonary veins converge to form a pulmonary venous confluence that in turn connects to the systemic venous system and right atrium. This confluence lies posterior to the pericardial sac behind the heart. The common pulmonary vein may rarely be atretic, a condition that results in death after a short time. Anomalous pulmonary venous connection may also be partial (see Chapter 19).
In approximately 25% of patients with total anomalous pulmonary venous connection, the drainage is directly into the right atrium or coronary sinus. The drainage in these cases is therefore exclusively intracardiac. In another 25% of patients, the drainage is through infracardiac connections, that is, the hepatic and portal veins. In 45% of patients, a common pulmonary venous channel drains into an anomalous vertical vein joining the innominate vein or superior vena cava, thereby reaching the right atrium in a supracardiac manner. In approximately 5% of cases, the drainage is mixed, occurring through all three or any combination of two of these connections. Very rarely, there is no connection to either atrium except through some collateral vessels, a condition referred to as common pulmonary vein atresia.
Two-dimensional echocardiography can usually delineate the anatomy and demonstrate any associated anomalies. Rarely is cardiac catheterization or magnetic resonance imaging necessary for patients who have not undergone previous cardiac surgery.
Technique
Most patients are neonates with unstable cardiorespiratory status. Those who present with pulmonary venous obstruction are true surgical emergencies. In neonates, the procedure is usually carried out during a period of deep hypothermic circulatory arrest. Continuous cardiopulmonary bypass using bicaval cannulation with aortic cross-clamping and moderate systemic hypothermia is used in older patients.
A median sternotomy is performed. The pericardium is opened, and the distal ascending aorta is cannulated. If hypothermic arrest is to be used, a single cannula is introduced into the right atrium through the right atrial appendage. Cardiopulmonary bypass is initiated, and the patient is cooled for 10 to 15 minutes. The aorta is cross-clamped, and cardioplegic solution is administered into the aortic root. Pump flow is discontinued, and after draining blood from the infant, the venous cannula is clamped and removed.
The ductus must be dissected and occluded with a tie or metal clip before the initiation of cardiopulmonary bypass.
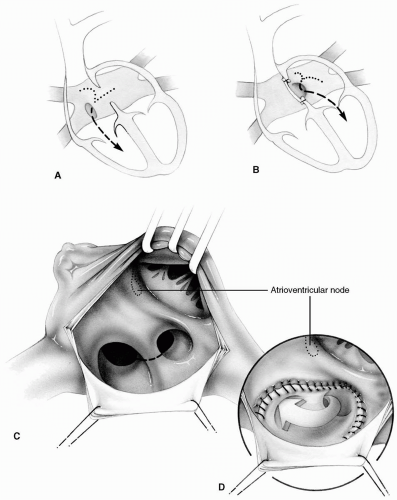
Intracardiac Type
A generous right atriotomy is made, somewhat below and parallel to the atrioventricular groove. The edges are retracted with fine sutures to provide maximal exposure. The inside of the right atrium is assessed carefully to delineate the precise anatomy. A patent foramen ovale or an atrial septal defect is always present. There may be a common pulmonary vein orifice opening into the right atrium, or the pulmonary veins may drain directly into the coronary sinus. In the latter case, the orifice of the coronary sinus is somewhat enlarged. The pulmonary venous return is rerouted into the left atrium by enlarging the atrial septal defect and using a pericardial patch to baffle the anomalous veins through the atrial septal defect.
The defect in the septum must be large enough to allow an unobstructed flow of pulmonary venous return. Most commonly, it is enlarged by extending its inferior margin toward the inferior caval or common pulmonary vein orifice.
Whenever the common pulmonary vein returns to the coronary sinus, its orifice is extended superiorly to reach the atrial septal defect. This incision must be well away from the anterior margin of the coronary
sinus to prevent damage to the atrioventricular node and the conduction system (Fig. 20-1). In addition, the incision in the roof of the coronary sinus should be extended to the posterior wall of the heart. The resulting defect in the atrial septum is closed with an autologous pericardial patch using 6-0 Prolene suture.
sinus to prevent damage to the atrioventricular node and the conduction system (Fig. 20-1). In addition, the incision in the roof of the coronary sinus should be extended to the posterior wall of the heart. The resulting defect in the atrial septum is closed with an autologous pericardial patch using 6-0 Prolene suture.
The continuous suturing of the patch must incorporate the wall of the coronary sinus well below its anterior rim to avoid the conduction system. Alternatively, only very shallow bites of endocardium are taken along the anterior rim of the coronary sinus.
When the patch is satisfactorily sewn in place, the atriotomy is closed with a continuous 6-0 Prolene suture. The heart is filled with saline, the venous cannula is replaced, cardiopulmonary bypass is recommenced, and the patient is warmed. The aortic cross-clamp is removed, and the cardioplegic site is allowed to bleed freely.
Infracardiac Type
This type is usually associated with obstruction and represents a true surgical emergency. During the cooling phase of cardiopulmonary bypass, the heart is elevated upward and to the right to expose the anomalous descending vertical vein. A 5-0 Prolene suture is placed
at the apex of the left ventricle to simplify retraction of the heart. The posterior pericardium is opened, and a vertical incision is made in the anomalous vein to decompress the pulmonary veins (Fig. 20-2). The heart is replaced in the pericardial well until complete cooling is achieved. The aorta is cross-clamped, and cardioplegia is given. After emptying the circulating volume into the pump, the venous cannula is removed. The heart is again lifted out of the pericardial well, and the previous incision on the anomalous vertical vein is extended longitudinally along the length of the pulmonary confluence.
at the apex of the left ventricle to simplify retraction of the heart. The posterior pericardium is opened, and a vertical incision is made in the anomalous vein to decompress the pulmonary veins (Fig. 20-2). The heart is replaced in the pericardial well until complete cooling is achieved. The aorta is cross-clamped, and cardioplegia is given. After emptying the circulating volume into the pump, the venous cannula is removed. The heart is again lifted out of the pericardial well, and the previous incision on the anomalous vertical vein is extended longitudinally along the length of the pulmonary confluence.
A matching incision is made on the posterior left atrial wall and is extended onto the left atrial appendage. A tie placed on the left atrial appendage helps to expose and position the left atrium for anastomosis. It is of paramount importance for the atriotomy to fall directly on the common pulmonary vein opening when the heart is allowed to resume its normal position.
The superior (rightward) aspect of the anastomosis is performed first with a continuous 7-0 Prolene suture. The inferior (leftward) aspect is similarly completed (Fig.20-2C).
A small right atriotomy is now performed to close the atrial septal defect, usually a patent foramen ovale. If primary suture closure appears to compromise left atrial size, an autologous pericardial patch should be used (see Chapter 19). Cardiopulmonary bypass is started again, and the patient is warmed.
The vertical incision on the common pulmonary vein channel may be extended slightly onto the left upper pulmonary vein to allow for a larger anastomosis. However, some surgeons advocate a “no touch” technique, staying well away from individual pulmonary venous ostia to reduce the incidence of postoperative pulmonary vein stenosis. Therefore it may be preferable to enlarge the anastomosis using the divided vertical vein (see subsequent text).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree