Introduction
Despite overwhelming evidence of the importance and effectiveness of smoking cessation in the prevention and management of heart disease, and the availability of effective cessation interventions it is, regrettably, still the case that smoking cessation has not figured prominently among the interventions provided by cardiologists. In part this may reflect the unfortunate and tragic persistence of outdated attitudes and perspectives: to the uninformed, smoking still remains a “habit” or “lifestyle choice” that can be addressed only by determination and the application of strong will. Some cardiologists may view the responsibility for smoking cessation as resting with others – typically the family physician. More likely, the lack of familiarity with the clinical principles of smoking cessation, a misperception of their efficacy and effectiveness, and a failure to appreciate the need for the systematic identification of smokers combined with the delivery of proven interventions may have contributed to an indifference to intervene in the cardiac setting.
It has been noted that it is difficult to identify any condition that is as prevalent, lethal and yet so prone to neglect as tobacco addiction.1 One – half of all smokers will die prematurely as a consequence of their tobacco use.2 In the United Kingdom it has been calculated that 40% of heart disease is attributable to smoking; the burden is similar in the USA and elsewhere in the developed world.3–5 There can be no doubt of the causative role that tobacco addiction plays in the development and accentuation of cardiac and cardiovascular disease; the evidence is overwhelming and has been accumulating for decades.6–7 Tobacco use is a principal contributor to the development of coronary artery disease (CAD), acute myocardial infarction (AMI), heart failure and the complications which inevitably follow. Deaths from coronary artery disease in smokers below the age of 45 exceed the mortality produced by any other tobacco -related disease.8 Smoking cessation may have a greater effect on reducing mortality among smoking patients with CAD than any other intervention or treatment.9 Sadly, tobacco use has been described as “reflecting a rare confluence of circumstances: (1) a highly significant health threat; (2) a disinclination among clinicians to intervene consistently; and (3) the presence of effective interventions”.10
“The rapidity and potency of risk reduction, as well as the other health – enhancing effects associated with smoking cessation, argue for the prioritization of smoking cessation in any program of secondary prevention of coronary disease.”
Forrester JS, Merz CNB, Bush TL et al JACC1996;27:991–1006
In recent years the prevalence of smoking has declined in the developed world; regrettably rates of smoking in developing nations continue to rise and herald epidemics of tobacco – related disease for years to come. 100 million deaths resulted from tobacco use in the 20th century11; it has been estimated that one billion more will occur in the 21st.12 A significant proportion of these deaths will occur as a result of the development of heart disease.
Cardiovascular physicians pride themselves on the degree to which their practices are based on carefully cultivated evidence derived from large, thoughtfully developed clinical trials which ultimately inform the development of practice guidelines. The evidence defining best practice for the treatment of smoking comes from several sources, principal among which are the influential guidelines that emerge regularly from the US Department of Health and Human Services.10,13
Smoking cessation is a very powerful and highly cost-efficient intervention.14–16 The most recent recommendations are clear and direct and have specific implications for all cardiologists and cardiovascular professionals: clinicians and health systems must “consistently identify and document tobacco use” among their patients and “treat every tobacco user seen in a healthcare setting”; clinicians should “offer every patient who uses tobacco… the brief treatments shown to be effective”; and should encourage the “use of the numerous effective medications available for tobacco dependence”.10
The pathophysiology of smoking and cardiovascular disease
Cigarette smoke contains nicotine, tar, and oxidant gases. Nicotine, the addictive constituent of tobacco, is delivered rapidly to the addiction centers of the brainstem when inhaled in tobacco smoke. Nicotine influences blood pressure and heart rate and, particularly in nicotine-naïve subjects, vasoconstriction. Carbon monoxide impairs the delivery of oxygen, while oxidant gases and their constituents play a major role in the initiation and progression of atheroma.17
Atheromatous lesions develop within a blood vessel as the consequence of a combination of pathophysiologic processes which impair vasomotor function, damage the vessel wall, accentuate the effects of elevated lipoproteins, and stimulate platelet aggregation and thrombosis. Cigarette smoking plays a distinct role in each of these processes. The constituents of cigarette smoke interfere with the availability of nitric oxide, thereby disrupting the normal vasomotor responses of the blood vessel wall; increase vascular inflammation, contributing to an accumulation of leukocytes on endothelial surfaces; promote the deposition of inflammatory and proinflammatory materials within the vessel wall; contribute to the elevation of total cholesterol and low-density lipoprotein cholesterol (LDL), and reduce levels of high-density lipoprotein cholesterol (HDL); increase the oxidation of LDL; accentuate platelet aggregation and adhesion; reduce the dissolution of thrombi; and contribute to plaque rupture.7,18,19 Smoking also leads to elevated levels of carbon monoxide (CO), producing increased levels of carboxyhemoglobin and thereby reducing the blood’s capacity to carry and release oxygen (Box 10.1).
Notwithstanding their increased risk of atherosclerosis, heart disease, and coronary events, smokers have been noted to demonstrate improved rates of survival following a myocardial infarction – the “smoker’s paradox” – a phenomenon attributable to the younger age at which smokers experience acute coronary events, their more favorable coronary anatomy, and reduced levels of co-morbidity.20,21
Second-hand smoke (SHS) is a combination of exhaled mainstream smoke (15%) and the sidestream smoke produced by an idling cigarette (85%).18 SHS is harmful and also contributes to platelet activation and endothelial dysfunction, distorts lipoprotein profile, elevates levels of carboxyhemoglobin, accentuates inflammation and contributes to the progression of atherosclerosis.22–24 Exposure to SHS has predictably deleterious effects on cardiac function; it results in a 30% elevation in the risk for coronary heart disease.25–28 The ischemic stress of exercise is accentuated upon exposure to SHS which may precipitate anginal symptoms.29,30 Second-hand smoke exposure has been estimated to cause 35 000 excess cardiovascular events each year in the USA and is the third leading cause of preventable death24 (Class I, Level A).
BOX 10.1 The Perfect Storm: cigarette smoke contributes directly to the processes underlying the development of CAD
- Impairs nitric oxide activity
- Diminishes vasomotor responses
- Increases vascular inflammation
- Promotes deposition of inflammatory materials in vessel wall
- Oxidizes lipoproteins
- Accentuates platelet aggregation
- Reduces dissolution of thrombi
- Contributes to plaque rupture
- Increases carboxyhemoglobin levels
Smokeless tobacco, whose use has surged in North America in recent years, frequently produces levels of nicotine that are higher, and more sustained, than those seen with smoking. The use of these products is known to produce acute cardiovascular effects.31 Blood pressure levels are influenced by the high sodium content of smokeless tobacco and the presence of its two pharmacologically active ingredients: nicotine and licorice.32 Smokeless tobacco users are more likely to have elevated levels of both diastolic and systolic blood pressure,33 and may have distorted lipoprotein profiles.34 Insulin resistance and a higher prevalence of diabetes have been noted in smokeless tobacco users.35,36 Physicians are advised to counsel users of smokeless tobacco products to quit.37
The benefits of smoking cessation
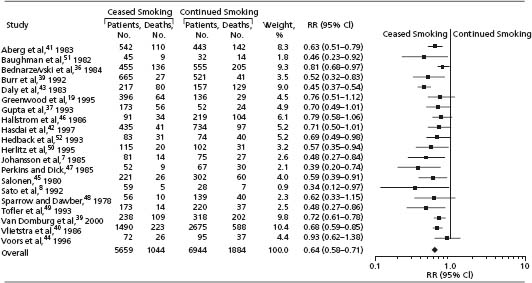
Smoking cessation confers distinct and immediate benefits to the smoker with cardiovascular disease. The elimination of exposure to mainstream tobacco smoke (and its multiplicity of toxic constituents) has a rapid impact on the reduction of those factors which contribute to the development and progression of atherosclerosis, removes the deleterious impact of smoking on established indices of cardiac performance, and eliminates the stimuli for clotting and thrombi formation central to the development of many acute cardiac conditions. The likelihood of sudden death, the propensity for myocardial infarction or re-infarction, the incidence of arrhythmia and an array of postinfarction complications, the adverse impact of smoking on myocadial contractility, and the progression of congestive heart failure (CHF) are all dramatically reduced following smoking cessation9,38–42 (Class I, Level A). A very substantial, 36% relative risk reduction of mortality is experienced following smoking cessation in those with coronary artery disease; this intervention is more potent than other classic secondary preventive strategies (e.g. cholesterol treatment) which, arguably, have received far greater attention in recent years (Table 10.1, Fig. 10.1).38 Quitting smoking produces a substantial, 30% decline in mortality in those with heart failure, a reduction of risk which equals or exceeds that produced by treatment with metoprolol, enalapril or spironolactone42 (Class I, Level A)
Table 10.1 Reducing mortality in CHD: the benefits of smoking cessation are greater and accrue more rapidly in comparison to other important preventive interventions
Source: adapted from Critchley JA, Capewell S. JAMA;2003; 290: 86 – 97
| Intervention | Reduction in mortality |
| Smoking cessation | 36% |
| Statin therapy | 29% |
| Beta-blockers | 23% |
| ACE inhibitors | 23% |
| Aspirin | 15% |
Figure 10.1 Pooled relative risks of mortality reduction when patients with CHD stop smoking: random effects meta-analysis of all 20 studies. The data show an overall 36% reduction in mortality associated with smoking cessation in patients with CHD. (Reproduced with permission from Critchley J, Capewell S. JAMA 2003; 290 (1):86 – 97.)
Controling exposure to cigarette smoke
Elimination or reduction of exposure to second-hand smoke has a significant impact on the incidence of acute coronary events for the individual and for the community. Anginal thresholds are reduced upon exposure to second -hand smoke; the benefits to the cardiac patient of the elimination of smoking in the home and work environments are many19,24,43 (Class I, Level A). Evidence continues to accumulate, from North America and Europe, of the beneficial effects of the introduction of smoke-free policies. There has been a distinct and clearly documented reduction in the incidence of acute myocardial infarctions in several cities following the introduction of bans on public smoking44–48 (Class I, Level B). Cardiologists can play a significant role in supporting the introduction of such progressive public health policies.
Nicotine addiction: the fundamental basis of smoking behavior
Minimal exposure to nicotine is all that is required to initiate the profound changes in neuroanatomy and neuro-physiology that result in a brain, and a life, ordered and organized to ensure regular intake of nicotine. Only minimal exposure to nicotine via inhalation is necessary to produce addiction. Nicotine is arguably the most destructive of all the addictive drugs encountered in our society. It is the only drug which when used as intended will result in the premature death of one-half of all its users. The effects of nicotine on brain function, and ultimately behavior, are mediated via a number of nicotine receptors, principal among which is the α4ß2 nicotinic acetylcholine receptor (nAChR) located in the brainstem. This receptor is felt to be responsible for the initiation and preservation of the nicotine -addicted state.49 Stimulation of nAChRs, principally the α4ß2 subtypes, results in a cascade of neurologic stimulation involving the mesolimbic system, culminating in the release of dopamine and other neurotransmitters in the nucleus accumbens region of the forebrain. Elevated levels of dopamine sustain addiction by producing pleasure, stimulation and mood modulation.50
In simple terms, the development of nicotine addiction can be seen as the requirement to maintain ongoing stimulation of nicotine receptors in order to ensure elevated levels of dopamine (Fig. 10.2). A cigarette is a drug delivery device which permits the rapid introduction of nicotine, titration of receptor stimulation, and dopamine release. As addiction develops, so does a degree of tolerance or desensitization at the receptor level which causes an increase in the absolute number of nicotine receptors. Smokers autotitrate their nicotine intake so as to maintain a personalized, idiosyncratic level of nicotine and comfort-maintaining levels of dopamine (Fig. 10.3).51
Figure 10.2 Nicotine stimulates receptors in the ventral tegmental area of the brainstem, causing the further stimulation, via the mesolimbic pathway, of regions in the nucleus accumbens of the forebrain, resulting in the release of dopamine. The brain rapidly adapts to the presence of increased levels of dopamine. Addiction quickly develops following minimal, repeated exposure to nicotine and the ensuing dopamine release.
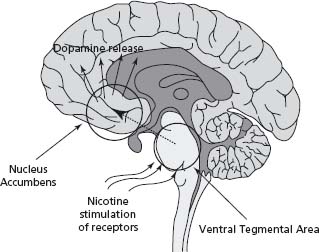
Figure 10.3 Smokers autotitrate nicotine intake to maintain plasma levels so as to accentuate “pleasure” and minimize “discomfort”. As nicotine levels rise, “pleasure” is experienced; as levels fall below a certain threshold, “discomfort” in the form of withdrawal or craving symptoms is experienced. In the neutral zone comfort is achieved without accentuating arousal and discomfort is avoided as abstinence symptoms do not develop. (Adapted with permission from Benowitz NL. Med Clin North Am 1992; 76:415 – 37.)
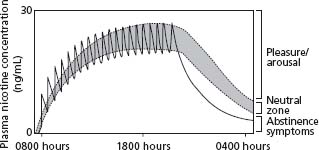
In the absence of nicotine intake, a withdrawal state quickly develops characterized by anxiety, irritation, frustration, depressed mood, lowered levels of concentration and restlessness.52 As a consequence of the relative deficiency of dopamine that accompanies smoking cessation, a prominent symptom of withdrawal is “hedonic dysregulation” – a feeling that there is minimal or no pleasure in life and that no enjoyment accompanies previously rewarding activities.53 Smoking cessation is often accompanied by the emergence of depressive symptoms and mood states. It is the discomfort and intensity of withdrawal, in association with the strongly conditioned behaviors, moods, and environmental factors associated with smoking, that can make this addiction so difficult to shed.54 It is unlikely that non-smokers will ever in their lifetimes have to make the significant, complex life transformation that a smoker must undergo to become a non-smoker.
It is important that clinicians appreciate the difficulties associated with cessation. Unassisted, only a very small proportion of smokers, 3%, are able to remain abstinent from tobacco for a six-month period; most relapse within eight days.55,56 Tobacco addiction should be viewed as a chronic relapsing addictive disorder requiring specific treatment for its elimination.
Most smokers understand the negative health consequences of their addiction, wish to stop smoking, and make at least one or two private attempts to stop smoking each year – the overwhelming majority of which are unsuccessful.57 Even in the face of compelling reasons for cessation, smoking cessation is difficult – following a myocardial infarction less than one-half of patients are able to stop smoking58; 17 – 40% of cardiac transplant recipients return to smoking at some point after their procedure.59–62 “Brain-stem trumps cerebral cortex”: it is important to realize that admonitions and exhortations to smoking patients are likely to be of only limited assistance in addressing this tenacious addiction, one which mandates the ongoing application of more insightful, evidence-based treatment strategies.
It is now understood that there are genetic predispositions affecting receptor density, the rate of nicotine metabolism, the likelihood and tenacity of addiction, and the difficulty that may be experienced in attempting to shed it.51,63–65 Individuals with certain psychiatric disorders, particularly schizophrenia and its related conditions, bipolar and other affective disorders, and substance abuse problems have a significantly increased likelihood of becoming smokers and a greater difficulty with cessation.54,66–68 Such patients have a markedly reduced life expectancy, most of which is accounted for by tobacco -related diseases, principal among which is cardiovascular disease (Class I, Level A).
Smoking cessation: the fundamental preventive intervention
Smoking cessation should be the priority in the secondary prevention of cardiac disease69 (Class 1, Level A). Sadly, there is evidence that physicians, particularly specialists, do not typically effectively address this preventive priority.70 The substantial benefits of cessation for a cardiac patient occur rapidly; they equal or exceed those of other preventive therapies. It is important to ensure that a systematic approach is adopted in every professional environment (office, clinic, and inpatient settings) which permits the identification of a patient’s smoking status; stimulates the delivery of clear, unambiguous, non-judgmental advice regarding the importance of quitting; prompts an offer of ongoing assistance with cessation; ensures familiarity with the prescription (and titration) of commonly used pharmacotherapies for cessation; and facilitates appropriate referral to other physicians, agencies or programs for follow-up where necessary or appropriate10 (Class I, Level A).
The time-honored 5 As (Ask – about smoking status; Advise – about the importance of quitting; Assess – the readiness to quit; Assist – by providing effective medications and counseling; Arrange – for appropriate follow-up) have informed and influenced professional behavior for years. But not all elements need to be delivered personally, separately or intensely. Some have suggested that we think of “Asking and Acting”. Consistency is the hallmark of a successful intervention system and unless a systematic approach is adopted in every professional setting, the potential to dramatically enhance cardiac health for our patients and communities will be diminished.1
Counseling
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


