Thoracic Trauma
EMERGENT INTERVENTIONS
Thoracic injuries are common, with up to one of five trauma patients presenting with injuries involving the chest. Thoracic injury and the ensuing complications are responsible for as much as 25% of the blunt trauma mortality.1 Motor vehicle accidents (MVA) are the most common cause of blunt thoracic injuries, followed by falls, with injury resulting from the transmission of energy to the chest wall and underlying structures. The size and location of the chest make it vulnerable to penetrating mechanisms, such as gunshot and stab wounds. Early identification and intervention can lead to significant impact on mortality in the trauma population.
Many injuries to the thorax require immediate intervention during the primary survey to support cardiopulmonary function. Establishment of a secure airway and ventilatory assistance should occur immediately in patients with respiratory compromise. Evidence of reduced respiratory compliance measured on mechanical ventilation (i.e., elevated peak and plateau airway pressures) and decreased breath sounds may indicate a tension pneumothorax, which requires urgent intervention. External bleeding should be controlled with direct pressure while resuscitation with crystalloid solution and blood products is initiated. Hemodynamic instability may signal injuries that need to be addressed during the primary surgery such as tension pneumothorax requiring decompression, hypovolemia requiring hemorrhage control and resuscitation, or cardiac dysfunction secondary to pericardial tamponade. Evaluation for sources of bleeding should commence after addressing airway and breathing issues. This should include a chest X-ray as well as a bedside ultrasound looking for the presence of a pericardial effusion, especially in the setting of penetrating trauma. Based on these initial interventions, decisions regarding subsequent management such as immediate operation can be determined. In the event of cardiac arrest, especially in the setting of penetrating mechanisms, a resuscitative thoracotomy can be considered but carries with it an extremely high mortality. The chance of a salvageable patient is even less in blunt trauma and resuscitative thoracotomy should be reserved for circumstances where there is a witnessed cardiac arrest.
EVALUATION
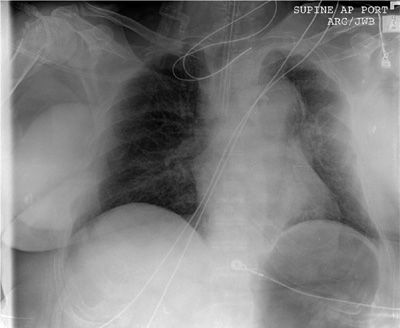
Most thoracic injuries can be identified with a physical examination and plain chest radiography. Physical examination will reveal superficial injuries, including chest wall defects and penetrating wounds. Deviation of the trachea at the sternal notch may reveal intrathoracic tension on the side opposite the trachea. Distended neck veins indicate heart failure or impaired venous return, which requires further evaluation. Chest radiography is performed on all significantly injured patients at risk for thoracic injuries. This study can be obtained rapidly in the trauma bay, with the results quickly revealed. The chest radiograph identifies the presence of a pneumothorax or hemothorax, as well as rib and sternal fractures. The appearance of a widened mediastinum may suggest a thoracic aortic injury (Fig. 106-1). An ultrasound of the pericardium, which may reveal pericardial blood, is a component of the focused abdominal sonography for trauma (FAST) examination. In recent years, thoracic CT angiography has emerged as a valuable tool in the evaluation of blunt thoracic trauma. CT provides visualization of the chest wall and hemithoraces, allowing determination of rib fractures, pneumothoraces, and hemothoraces, and pulmonary contusion. Of great value has been the ability to evaluate the thoracic aorta for injury that historically required standard angiography when suggested by a chest radiograph. Chest CT angiography is able to identify transection of the aortic wall, as well as lower-grade injuries that involve only the aortic intima. Many thoracic surgeons have modified their approach and now proceed with operative intervention based on the chest CT alone, without formal angiography.
Figure 106-1 Widened mediastinum suspicious for thoracic aorta injury.
Penetrating injuries to the chest that cross the mediastinum or are in the vicinity of the heart and mediastinal structures require a methodical evaluation. Penetrating wounds in “the box,” an area defined by the sternal notch superiorly, the costal margin inferiorly, and the nipples laterally, are in this group requiring further evaluation. This includes an assessment of the cardiovascular and aerodigestive structures of the mediastinum. Immediate ultrasound is performed to evaluate the pericardium for effusion. In the setting of an associated hemothorax, ultrasound may yield false-negative results due to decompression of a cardiac injury into the pleural cavity. In stable patients further evaluation has historically included an angiogram of the chest, which has now been replaced by CT angiography in most of the situations. The heart and great vessels are evaluated for injury, although this can be impeded by the presence of retained missile fragments that cause scatter on CT. In this setting, standard angiography may be necessary. Depending on the trajectory of the penetrating object, the trachea and proximal airways may require evaluation with bronchoscopy. If injury is suspected, the esophagus should be assessed with a combination of esophagoscopy and contrast esophagography. Frequently, thoracic CT will accurately identify the trajectory of the wound and thus guide the need for further evaluation.
MANAGEMENT
Up to 85% of all thoracic injuries can be managed with nothing more than a tube thoracostomy. In most cases, the placement of a chest tube is urgent but should still be performed in a controlled manner that includes strict sterile preparation and excellent surgical technique. This is very important given the morbidity associated with an empyema that can result from improper chest tube placement. The chest should be prepared appropriately with a formal skin preparation as well as wide draping to maintain the sterility of the field and the tube to be placed. The skin incision should be in the fourth to fifth intercostal space usually identified as the level of the nipple to stay superior enough to avoid the highest reach of the diaphragm. A tunnel is created in a superior direction and the chest is entered bluntly in an interspace above the skin incision. The lung is palpated to confirm chest entry and evaluate for intrathoracic adhesions. A tube large enough to drain blood (typically 32–36 Fr) is then advanced superiorly through the incision and posterior to the lung. Chest tubes that are being placed only for a pneumothorax can be positioned in the anterior hemithorax. The thoracostomy is then connected to an underwater drainage device providing 20 cm H2O suction.
Tube thoracostomies that drain large amounts of blood on initial placement or demonstrate ongoing output may indicate active intrathoracic bleeding that requires thoracotomy. Other indications for immediate thoracotomy include a massive air leak with associated pneumothorax or drainage of esophageal or gastric contents from the chest tube. The choice of thoracic approach depends on the presumed injured structures. Access to the lungs, pulmonary vasculature, and hemidiaphragm is through a posterolateral thoracotomy that is best performed through the fifth interspace, with or without removal of the fifth rib. The decision of which side to approach the injury depends on the target organ and which portion of the organ needs to be exposed. A median sternotomy can be a highly versatile approach, allowing exposure of the right heart, ascending aorta, aortic arch with right-sided arch vessels, and pulmonary vasculature.
 CHEST WALL AND PLEURAL SPACE INJURIES
CHEST WALL AND PLEURAL SPACE INJURIES
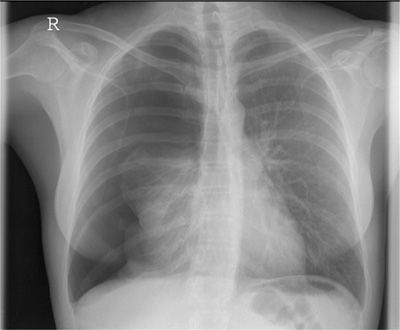
During the trauma evaluation, chest wall injuries are commonly recognized. Chest wall tenderness and changes in chest wall motion are suggestive. Some patients require immediate intervention for chest injuries, but most will subsequently undergo further evaluation. Injuries involving the chest wall or pleural space can frequently be identified on chest radiographs (Fig. 106-2). Chest CT is a common part of the evaluation for thoracic injuries at many centers. CT identifies rib and sternal fractures, as well as pleural air and blood with high sensitivity.
Figure 106-2 Multiple left-sided rib fractures on a plain chest radiography.
Rib Fractures
Fractures of the ribs are the most common thoracic injury following blunt trauma, with almost 80% of patients with chest injuries sustaining one or more fractures. Rib fractures typically occur secondary to compression of the thoracic cage in an anteroposterior or lateral direction that often will dictate the location of the cortical disruption along the rib. Steering wheels and seatbelts are commonly identified as the impinging structure resulting in a fracture.
Rib fractures can vary greatly in severity, depending on the number present and patient characteristics. Associated pain can be severe and the resultant splinting can lead to the development of atelectasis and pneumonia. Aggressive analgesia should be provided to allow adequate pulmonary toilet and promote comfort. Adequate analgesia can be achieved with IV narcotics in mild cases but, in more severe cases, patients benefit greatly from the provision of epidural analgesia. Epidural analgesia after chest wall injuries has been associated with fewer ventilator days, shorter intensive care unit (ICU) length of stay, and fewer hospital days. Furthermore, one study demonstrated fewer pulmonary infections and decreased duration of mechanical ventilation with the use of epidural analgesia in patients with three or more rib fractures.2 Nonsteroidal anti-inflammatory drugs (NSAIDs) are also beneficial in conjunction with narcotics. Aggressive pulmonary toilet, including deep breathing, frequent coughing, and incentive spirometry, should be highly encouraged. Chest physiotherapy and positive expiratory pressure exercises may also be beneficial. Severe chest wall injuries with respiratory failure may require mechanical ventilation.
There has been renewed interest in the operative fixation of rib fractures, although the optimal indications for these procedures and their associated benefit remain incompletely defined. Tanaka et al.3 performed the only randomized, controlled study of operative fixation versus internal pneumatic stabilization. Groups were well matched in terms of injury severity, criteria for ventilatory support, and ventilator management. The incidence of pneumonia was lower in the surgical group (22% vs. 90%) as was the length of ventilation and length of ICU stay. The investigators reported improved lung volumes, decreased pain and dyspnea and higher return-to-work at 1 year with surgical fixation. The investigators concluded that surgical stabilization may be preferable for severe flail chest patients when prolonged ventilatory support would otherwise be expected. Other studies have yielded less supportive data. Ventilated patients who fail to demonstrate progress in moving toward extubation or patients with alternative indications for surgical intervention (e.g., retained hemothorax) should be strongly considered for chest wall stabilization.
Flail Chest
In its most severe form, large amounts of energy transferred to the chest wall can result in the creation of a flail segment, defined as two or more adjacent ribs that are each fractured in two or more locations. This results in a separation of a segment of the chest wall. Although pulmonary mechanics can be disrupted by the presence of a flail segment, the greatest physiologic insult is caused by the underlying pulmonary contusion that almost invariably occurs. As mentioned earlier, fixation of the chest wall is an attractive option but it does nothing to address the underlying contusion. Most current ongoing trials examining fixation exclude patients with large contusions, making further study of operative intervention in this population a challenge.
Pneumothorax
Simple pneumothorax is created when a tear in the pleura allows entry of air into the pleural space with resultant loss of negative intrathoracic pressure. If an injury to the lung parenchyma produces an air leak, the air accumulates in the pleural space with each breath, markedly increasing intrathoracic pressure and thereby shifting the mediastinum toward the opposite hemithorax (Fig. 106-3). This so-called tension pneumothorax is immediately life-threatening because of the limitation of vena caval blood flow causing decreased venous return, which results in hypotension, tachycardia, and cardiac arrest. Once the diagnosis of tension pneumothorax is suspected, treatment should be initiated immediately without waiting for chest radiograph confirmation. This is most rapidly done by placing a large-bore needle into the second intercostal space. This is then followed by a formal tube thoracostomy under sterile precautions.
Figure 106-3 Tension pneumothorax on the right.
Pneumothorax that is visible on a chest radiograph requires performance of a tube thoracostomy. Chest tube drainage should continue until any pulmonary air leak has resolved and pleural fluid drainage is not excessive (<150 cc/d). As CT scan is being performed more commonly in the evaluation of trauma patients, many injuries are now identified that had previously not been detected. Occult pneumothorax, defined as a pneumothorax that is seen on chest CT but not on plain films, is being diagnosed more frequently.4 Retrospective data in these cases suggests that placing a chest tube will lead to longer ICU and hospital stays.5 Most occult pneumothoraces can be safely observed but enlargement of the pneumothorax on follow-up imaging necessitates a chest tube. Another key question has been the factor of positive pressure ventilation. Several investigators have tried to answer the effect that positive pressure has on occult pneumothorax, with conflicting results. In a prospective study, Enderson et al.6 found that patients with pneumothoraces treated with observation who underwent positive pressure ventilation experienced an unacceptable rate of complications, with 3 of the 15 patients developing a tension pneumothorax. In contrast, in a prospective randomized study Brasel et al.7 found no increase in complications regardless of whether chest tube or observation was chosen. Both studies suffered from low numbers but suggested that the majority of patients with occult pneumothoraces will not have progression regardless of the presence of positive pressure ventilation. Patients who demonstrate a large amount of subcutaneous air without significant pneumothorax should be followed closely, with a low threshold for placing a chest tube, because a pulmonary air leak may still be present.
Pneumothorax and Open Chest Wound
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree