Fig. 12.1
NYHA functional class before and after surgery
TR was severe in 20 patients, moderate in 41 and mild in 4. The median TR grade was 3 (range 2–4; interquartile range 3–4) (Fig. 12.2).
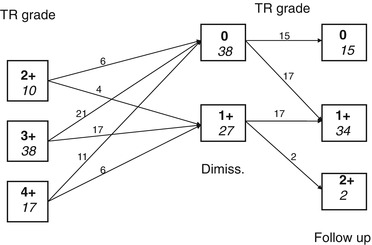
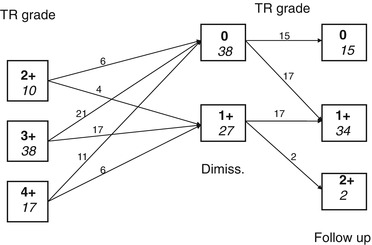
Fig. 12.2
Tricuspid regurgitation (TR) grade before and after surgery
The RV dimensions and volumes were calculated in ASD patients echocardiographically and in the PVR patients with cardiac magnetic resonance imaging (CMRI).
Surgical treatment of the primary cardiac lesion included ASD heterologous pericardial patch closure in 40 patients and pulmonary valve implantation (PVI) in 25 patients.
Functional TR was treated by annuloplasty (De Vega operation) in 48 patients, by a rigid tricuspid valve ring in 14 and by tricuspid valve replacement with biological prosthesis in 3. A ring size of 34 mm was used routinely for males (n = 9) and a ring size of 32 mm for females (n = 5).
Preoperative TR grading was assessed echocardiographically in four grades using colour Doppler flow images to characterise flow direction in the inferior vena cava or hepatic veins, as grade 0 = absent, 1 = trace, 2 = mild, 3 = moderate and 4 = severe.
The indications for surgical treatment of functional TR were a moderate to severe degree (grades 3 and 4) of insufficiency and/or the presence of considerable tricuspid annular dilation. The tricuspid annular dimensions were determined directly from the heart in the operating room, by measuring the maximal diastolic size of the tricuspid annulus between the anteroseptal and anteroposterior commissures.
No hospital deaths occurred during the study.
At discharge, TR was not found in 40 patients and was only traces (grade I) in 25. The median TR grade was 0 which represents a significant (p = 0.001) improvement from the preoperative status (Fig. 12.2).
The follow-up was complete in all 65 surviving patients and ranged from 12 to 96 months (mean 63 months).
One late death occurred due to complications that were not cardiac related and one patient (1.5 %) underwent tricuspid valve replacement at 5 years after annuloplasty.
Both the NYHA functional class (p = 0.001) and TR grade (p = 0.001) were significantly improved among survivors (Figs. 12.1 and 12.2).
No hospital deaths occurred in our series [8] and a significant improvement was observed in both NYHA functional class and TR grade among survivors. The incidence of reoperations (1/65 = 1.5 %) compared favourably with values reported in other comparative studies [7–10, 12, 16–22].
The postoperative RV dimensions and volumes, calculated at 12 months after surgery in all patients, showed a significant reduction [8].
Our results show that surgery for functional TR can be performed with low risk, and all our patients achieved a significant clinical improvement as compared to patients with acquired heart disease [9–12, 14, 17–21]. Several factors may be considered to explain that, like the younger mean age of our patients (46 years), the surgical treatment often including RV volume reduction and TV surgery and the normal preoperative LV function in all our patients.
Tricuspid valve repair is preferable to tricuspid valve replacement, but no clear indications are available to demonstrate which techniques are optimal for repair of the tricuspid valve. The annuloplasty techniques (like Key and De Vega techniques) are simple and have been widely used, but the recurrence of moderate to severe TR in these patients has been reported quite frequently [17, 18]. Another technique suggested has been the use of an annuloplasty ring [18, 20]. In this case, the ring annuloplasty will remodel the annulus, decrease the tension on the suture lines, increase leaflet coaptation and prevent recurrent annulus dilation.
Rigid ring annuloplasty has been used routinely, while flexible rings have been developed more recently to permit a physiologic motion of the tricuspid annulus.
No significant differences related to annuloplasty versus the rigid tricuspid valve ring were observed in our series [8] during the follow-up period.
In cases of tricuspid valve replacement, the use of a bioprosthesis is preferable to a mechanical valve in the tricuspid position. Previous reports [21, 22] have shown that a bioprosthesis in the tricuspid position is more satisfactory than in the mitral position, as this results in favourable long-term outcomes with a low incidence of structural valve deterioration and reoperation.
Another possible advantage using bioprosthesis in tricuspid position can be the possibility to perform future transcatheter valve replacement with the so-called “valve-in-valve” procedure [23].
In conclusion, functional TR in adult patients with congenital heart disease is related to RV dilation/dysfunction, usually as a consequence of chronic RV volume overloading.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


