CVP value
Possible explanations
Low (<10 mmHg)
Hypovolemia
High (>15 mmHg)
Tricuspid regurgitation
Primary systolic right ventricular dysfunction
Right ventricle outflow obstruction
Diastolic right ventricular dysfunction
Pulmonary hypertension
Pulmonary embolism
Cardiac tamponade
17.1.4 Pulmonary Artery Pressure (PAP)
The use of pulmonary artery catheters is generally avoided in TV surgery. In small paediatric patients pulmonary artery catheters are not available; in adults, the presence of the catheter inside the right heart chambers may disturb the surgical procedure.
However, PAP is an important measurement in this setting. It can be indirectly derived using echocardiographic examination (transthoracic or transoesophageal) based on the velocity of the systolic regurgitant flow of the TV in case of TV repair.
17.1.5 Left Atrial Pressure (LAP)
LAP is less important in TV surgery. It can be measured using direct surgical insertion of a left atrium catheter, when additional conditions suggest the risk for left ventricular dysfunction.
17.1.6 Cardiac Output
Measurement of cardiac output with thermodilution techniques and pulmonary artery catheters is usually difficult for the above-reported reasons. In adult patients, cardiac output can be assessed using pulse waveform systems; in paediatric patients, echocardiography may offer some additional information. In general, in paediatric patients, the adequacy of cardiac output may be evaluated looking at the indirect signs of poor peripheral perfusion. These include cold, pallid, and mottled skin; high central–peripheral temperature gradient; prolonged peripheral vein filling time; dilated jugular veins; enlarged and stiff liver; faint or absent peripheral pulses; and poor urine output.
17.1.7 Echocardiography
Echocardiographic assessment of the RV is a key aspect of postoperative treatment. It can be achieved with both transthoracic and transoesophageal echoes, even in small children, using adequate probes. The classical view for assessing RV function is the “inflow–outflow” view, where the aortic valve is in the middle and the RV is embracing it. This view allows to assess the RV free wall motility. Additional measures include the tricuspid annular plane systolic excursion, which may be useful in case of TV repair, but not in TV replacement.
17.1.8 Central Venous Oxygen Saturation (ScVO2)
Under normal conditions, the ScVO2 value is 70–75 %; that means that if the arterial oxygen saturation is 100 %, the oxygen extraction rate (O2ER) is 25–30 %. A decrease of the ScVO2 (<70 %) with a concomitant increase in the O2ER is representative of an inadequate cardiac output, which may derive from an inadequate preload or from a poor cardiac contractility.
ScVO2 is measured with serial samples from the CVC catheter; however, a continuous measurement is feasible in newborns, larger paediatric patients, and adults, using the available CVCs with oximetric sensor at the distal tip. This continuous measurement provides a reliable value and represents a very useful information, able to immediately detect rapid changes of the ScVO2 [3] (Fig. 17.1).
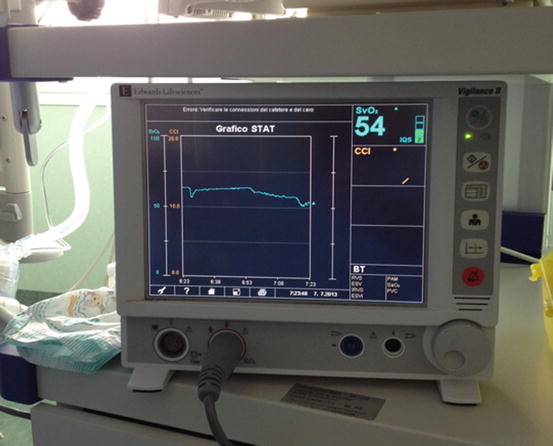
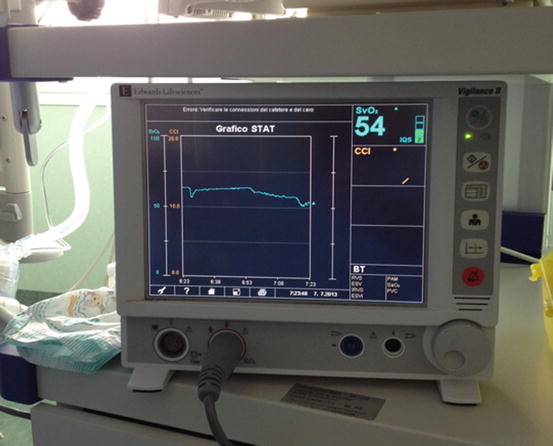
Fig. 17.1
Continuous ScVO2 measurement during the postoperative course
17.1.9 Arterial Blood Lactates
When the cardiac output is inadequate, anaerobic metabolism takes place, with lactate formation. Arterial blood lactates exceeding 3 mmol/L are suggestive for an inadequate cardiac output, even if other conditions (reperfusion, liver failure, hyperglycaemia) should be ruled out. Hyperlactataemia is associated with bad outcomes after cardiac operation [4–7].
17.1.10 End Tidal CO2 (ETCO2)
ETCO2 is measured by capnography. ETCO2 is a measure of both the adequacy of ventilation and pulmonary perfusion. In the first case, both the ETCO2 and the arterial pCO2 are increased. Low levels of ETCO2 with normal or increased values of arterial pCO2 are suggestive for a poor lung perfusion that is usually derived from the inability of the RV to recruit venous blood into the systemic circulation (Table 17.2).
Table 17.2
ETCO2 in clinical context
ETCO2 value | PaCO2 value | Possible reasons |
|---|---|---|
Increased (>40 mmHg) | Increased (>45 mmHg) | Hypoventilation |
Excessive dead space | ||
Respiratory distress syndrome | ||
Lactic acidosis | ||
Excessive NaHCO3 administration | ||
Decreased or normal | Increased or normal | Low pulmonary blood flow |
Pulmonary embolism | ||
Low cardiac output | ||
Tracheal tube obstruction | ||
Decreased | Decreased | Hyperventilation |
17.1.11 Pulse Oximetry
Pulse oximetry provides a non-invasive, on-line measure of peripheral oxygenation, and its use is mandatory in the setting of postoperative care of CHD patients.
17.1.12 Near-Infrared Spectroscopy (NIRS)
NIRS provides a non-invasive measure of the cerebral venous oxygenation, with electrodes placed on the forehead. In paediatric patients, somatic NIRS, with electrodes placed on the dorsal region, may be an additional measure. The regional oxygen saturation (rSO2) obtained with this measurement is a surrogate of the ScVO2 and behaves in a similar way [8, 9].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


