Fig. 7.1
Echocardiographic picture of a neonate with pulmonary atresia and intact ventricular septum with a severely hypoplastic tricuspid valve and right ventricle
In a minority of patients with PA and IVS, the TV is large with an Ebstein-like deformation and the RV is dilated. These patients are excluded from our considerations.
The decision making of the safest treatment depends mainly on the assessment of:
TV size and function
RV size and morphology
Coronary artery system
7.2.1 Tricuspid Valve
The TV is always abnormal concerning morphology and size.
Usually the leaflets are thickened and dysplastic with abnormal short chordae and small papillary muscles. The annular sizes range from almost normal to severely small.
The morphology, function and size of the tricuspid valve are best delineated by echocardiography. The size of the TV should be measured in diastole from the apical four-chamber view to allow comparison with published normal data [5].
The normal range of the TV diameter in the paediatric population changes with age and growth and is best correlated to the body surface area (m2). It has been proven very useful to express the normal range of diameters as the Z-value.
The Z-value is computed as follows:
The “normal diameter” is the diameter in a normal individual of the same body surface area as the patient.
Figure 7.1 shows the Z-values of the tricuspid valve annulus (cm) measured by echocardiography in a normal population according to the body surface area published by Pettersen et al. in 2008 [8].
The data of Pettersen and co-workers have the advantage over some previous publications in that the diameters are measured by echocardiography in a large cohort of normal children and adolescent (782 control persons aged 1 day–18 years) and are not derived from formalin-fixed post-mortem specimen [7].
A Z-score = 0 corresponds with the estimated mean, whereas Z = +/−1, +/−2, +/−3 corresponds with +/−1, +/−2, +/−3 standard deviation (SD).
In a normal distribution 68 % of the population would be classified within the mean +/−1 SD, 95.4 % within the mean +/−2 SD and 99.7 % within the mean +/−3 SD [8] (Fig. 7.2).
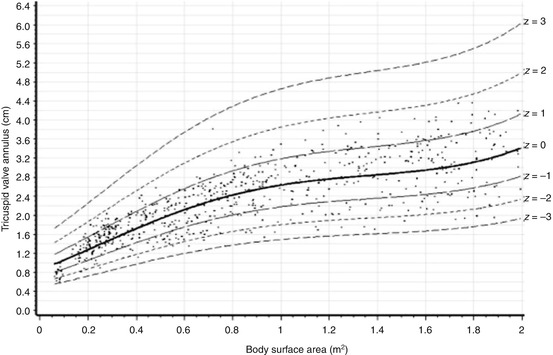
Fig. 7.2
Scatter plots of the tricuspid valve annulus versus body surface area. The superimposed solid line represents the estimated regression equation labelled as z = 0. The superimposed dashed lines represent the +/−1, 2 and 3 Z-values (With the permission of Pettersen et al. [8])
7.2.2 Right Ventricle
In the normal heart the RV has a tripartite structure consisting of an inlet, an outlet and an apical component [10, 11].
In patients with PA and IVS, the RV morphology ranges from a severely small and hypertrophied ventricle to an almost normal cavity. Due to the various degree of hypertrophy and hypoplasia, the RV can either remain its tripartite structure on the good end of the spectrum or appear – due to the enormous myocardial hypertrophy – as a bipartite (only inlet and outlet portion) or unipartite (only inlet portion) cavity on the bad end of the spectrum.
The occurrence of each type of ventricle in neonates was reported as tripartite in 59 %, bipartite in 34 % and unipartite in 7 % of the patients [2].
There is a correlation between the diameter of the TV annulus and the size of the RV cavity (Fig. 7.3), [9, 12]. The smaller the TV, the smaller is the RV.
Fig. 7.3
Correlation between the Z-value of the tricuspid valve and the right ventricular cavity size (echocardiography and/or angiography). Normal for age RV cavity size was assigned a value of 0, extreme hypoplasia −5 and +5 indicating the most extreme enlargement (Hanley et al. with permission [9])
This correlation has prompted some groups to advocate the use of the size of the TV as a guide to surgical management.
7.2.3 Coronary Arteries
A proportion of patients with PA and IVS may have unique coronary artery abnormalities unlike in other forms of CHD. These abnormalities are detectable especially in the subset of patients with a very small TV and RV. These coronary artery abnormalities range from clinically unimportant myocardial sinusoids through RV coronary fistulas (or connections) to an RV-dependent coronary circulation [13].
The survival is very much influenced by the presence of significant coronary anatomy anomalies [9]. For the decision making of the optimal therapy, a detailed assessment of possible RV coronary artery fistulas is mandatory.
The frequency of RV coronary artery fistulas in 145 patients was reported to be 45 % [9]. There is an inverse correlation between the diameter of the TV annulus – and therefore also to the RV size – and the probability of right ventricular coronary connections (Fig. 7.4) [9]. The probability of RV coronary artery fistulas was 98 % at a Z-value of −5, whereas only 5 % at a Z-value of 0.
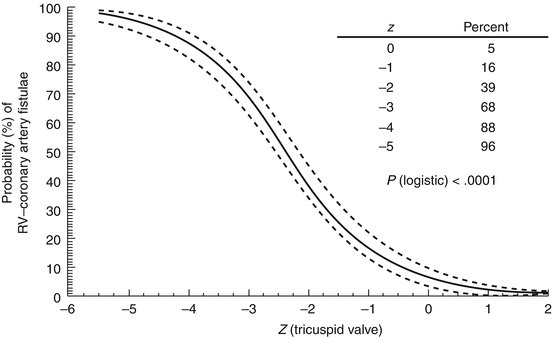
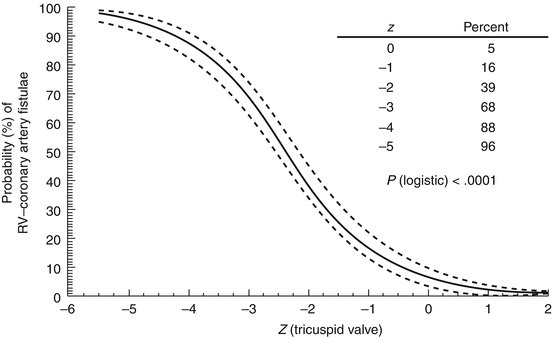
Fig. 7.4
Relation between the Z-value of the tricuspid valve annulus and the probability of RV coronary artery fistulas. The solid line is the continuous point estimate of the value, and the dashed line encloses the 70 % confidence interval. RV right ventricle (Hanley et al. with permission [9])
The frequency of RV-dependent coronary artery circulation ranges between 4.4 and 9 % according to some of the largest studies on PA and IVS [9, 14, 15].
The only correlate of RV-dependent coronary artery circulation was also the small size of the tricuspid valve [9]. At a TV Z-value of −5, the probability of an RV coronary artery-dependent circulation was 19 %.
7.3 Treatment Options for a Small TV with the Arrangement of PA with IVS
The key question for the treatment is whether the TV is large enough to accommodate the total systemic venous flow into the RV and from there into the pulmonary arteries.
The size of the TV is an important parameter for the therapeutic decision, but it would be far too simplistic to rely only on this single parameter.
The entity “pulmonary atresia with intact ventricular septum” is a good example on how to deal with the decision making in patients with a small TV.
For the decision making the following parameters are important to be assessed:
Size of the tricuspid valve (Z-value)
Size and morphology of the RV (tri-, bi- or unipartite) including the morphology of the RVOT (membranous vs. muscular atresia)
Anomalies of the coronary arteries
RV coronary artery fistulas
RV-dependent coronary artery circulation
The aim of the therapy is to have a low mortality, if possible a biventricular repair and as few as possible interventions.
As the primary step of treatment in the neonatal period, there are three options:
Aortopulmonary shunt (AP shunt)
Opening of the RVOT (by intervention or surgery)
Combination of both (by intervention or surgery)
7.4 Treatment Algorithms
7.4.1 Primary Treatment in the Neonatal Period
The neonate with PA and IVS has a duct-dependent pulmonary artery circulation requiring PGE1 infusion to maintain ductal patency.
After stabilisation and evaluation of the neonate, the best treatment options are selected on an individual basis according to the TV size, the RV morphology and the coronary artery anatomy.
With the exception of patients with an RV-dependent circulation and very tiny TV and RV, there is nowadays a trend to decompress the RV in most patients with a tripartite and possible bipartite RV and membranous atresia of the RVOT.
A decompression of the RV is a prerequisite to promote growth of the RV and to achieve a biventricular repair.
There are several large – mostly retrospective – studies concerning the management and outcome in patients with PA and IVS and a small TV and RV [2, 9, 11, 14]. Due to the great diversity of the morphology and the low prevalence of this pathology, the treatment algorithms are not conclusive.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


