Fig. 5.1
Radiograph of flail chest with underlying lung contusion (indicated by arrow)
Lung ultrasound: Many of the injuries resulting from thoracic trauma are better demarcated by ultrasonography than on a radiograph. Ultrasound (USG) also has the advantage of being carried out bedside when compared to a CT thorax. USG can be very helpful to detect the presence of hemothorax, pneumothorax, and pulmonary contusion. Once diagnosed, USG can also be very helpful to quantify and drain the hemothorax (Fig. 5.2).


Fig. 5.2
Ultrasound guided drainage of a retained hemothorax (see text for details). Courtesy of www.Criticalecho.com with permission
On an USG, absence of lung sliding and the presence of lung point are considered diagnostic of pneumothorax. On the M mode, the absence of lung sliding is seen as absence of the normal granular pattern of the lung below the pleural line (Fig. 5.3). Other signs of pneumothorax can also be found. In Fig. 5.3, the linear pattern of the chest wall seems to extend below the pleural line. This is also called the stratosphere sign [2].
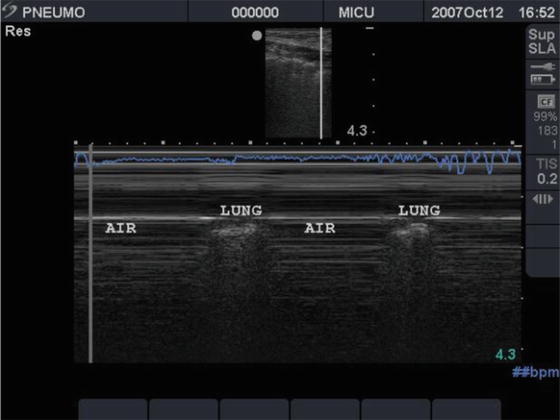
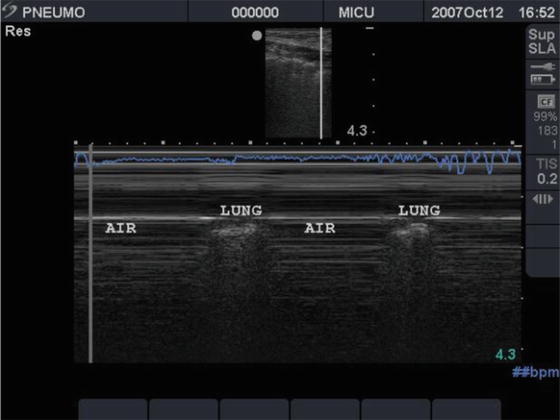
Fig. 5.3
Ultrasound demonstrates several findings consistent with a pneumothorax (see text for details). Courtesy of www.Criticalecho.com with permission
Lung USG can be used to diagnose pulmonary contusion and helps distinguish basal atelectasis from contusion after thoracic trauma (Fig. 5.4). The presence of a pulmonary contusion is associated with significant morbidity and long-term sequelae.
CT thorax: is the gold standard for estimating the extent of thoracic injury, though difficulty in mobilizing the patient limits its value. Figure 5.5 shows a CT thorax with flail chest and underlying lung contusion and pneumothorax.
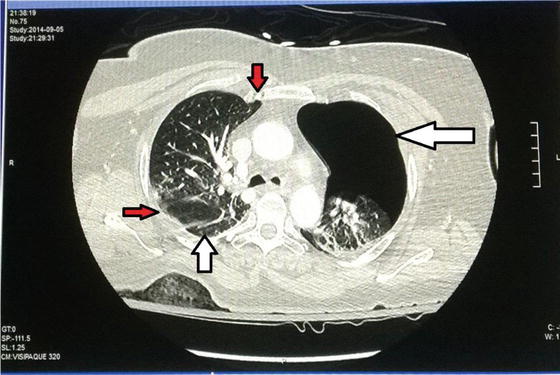
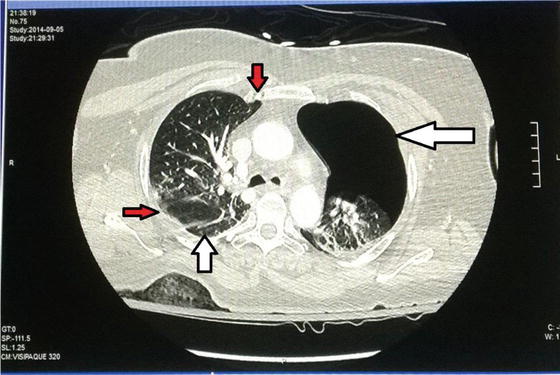
Fig. 5.5
CT thorax: showing a right-sided pneumothorax (white arrow), sternal fracture (downward arrow), left-sided flail segment (red-colored sideward arrow), and contused lung (upward white arrow)
Nonoperative Treatment
The role of surgery in management of a flail chest has been limited in the past, and nonsurgical management alone has been the gold standard.
The principles of nonoperative treatment include:
Immediate recognition and treatment of accompanying life-threatening injuries like hemo-/pneumothorax
Bronchial hygiene and chest physiotherapy
Adequate analgesia
Optimizing fluid therapy
Ventilation and treatment of hypoxemia
Immediate Therapy
Sandor [3], while evaluating their case series, reiterated the importance of accompanying lesions in flail chest and stated that survival was based on correction of hypoxemia by decompressing a tension pneumothorax and aspiration of the bronchi. Undetected and untreated pneumothorax may account for many of the fatal cases.
In a series by Miller et al., of the 82 patients studied, 70 had associated pneumothorax or hemothorax. Immediate evacuation of the pleural space is life saving in thoracic trauma [4].
Bronchial Hygiene
Retained secretions along with compromised cough due to pain can worsen hypoxemia. In the series by Sandor [3], delay in aspirating bronchial secretions caused three of the patients to deteriorate and two of them recovered immediately after bronchoscopy and lavage. Due to discontinuity of the flail segment with the rest of the thoracic cavity, coughing is not effective. The forceful expulsive component of cough is dissipated in paradoxical motion of the chest wall [4]. Chest physiotherapy, deep breathing exercises, and incentive spirometry are an integral part of the management of flail chest. Preventing basal atelectasis goes a long way in preventing hypoxemia.
Analgesia
Pain contributes significantly to increased respiratory insufficiency in flail chest. Limited ability to cough and splinted, shallow breathing contribute to retained bronchial secretions and atelectasis. Analgesia therefore is a crucial component of management in flail chest. The various modalities of pain relief available are:
Intravenous narcotics
Epidural narcotic/anesthetic
Intercostal nerve block
Intrapleural anesthesia
Thoracic paravertebral block
IV Narcotics
Administration of narcotics has evolved from intermittent administration with poor pain control to patient-controlled analgesia (PCA). The latter enables the patient himself to control administration of bolus doses, in addition to a baseline flow in the wake of increased pain. This has increased patient comfort manifold.
However, the disadvantages of narcotics limit their usefulness in thoracic trauma. In the cohort of patients with flail chest, with a compromised breathing reserve, narcotic-induced respiratory depression is always a concern. Sedation, cough suppression, and hypoxemia are the other worrisome features of narcotic use.
Epidural Analgesia (EA)
The pain management guidelines for blunt thoracic trauma provide a level 1 recommendation for epidural analgesia. The advantage of this modality is that it provides analgesia while the patient remains awake and cooperative for bronchial toileting. EA has been found to reduce the duration of mechanical ventilation in comparison to parenteral opioids [5, 6], improve pulmonary function (Forced Vital Capacity, lung compliance, decrease airway resistance) at 72 h [7], reduce the incidence of nosocomial pneumonia [5], and improve pain control with cough and deep breathing [7–9].
However, a meta-analysis of randomized controlled trials on the effect of epidural analgesia in patients with traumatic rib fractures showed no benefit of EA on primary outcomes such as mortality, ICU length of stay, and hospital length of stay [10].
Adverse Effects
EA results in a higher incidence of hypotension than other modalities [7–9]. Other disadvantages of EA are that it is technically more challenging and needs expertise. Epidural hematoma, epidural abscess, and respiratory insufficiency due to a higher level of insertion are rare possibilities. Combining a narcotic with an anesthetic agent can help reduce the anesthetic-induced adverse effect.
Applicability
By extracting the data from the national trauma data bank, Dehghan et al. found that EA was utilized in only 8 % of the patients. EA, however, was the preferred mode of analgesia [11]. In ventilated patients where motor assessment is not feasible, this mode of analgesia has significant risk and is not preferred.
Intercostal Nerve Block
This modality involves injection of anesthetic agent into the posterior segment of the intercostal space of one rib above and below the fractured rib. Continuous infusion of anesthetic agent is feasible to produce effective analgesia. However, shorter duration of effect, multiple injections, and difficulty in cases of higher rib fractures makes this modality less favorable.
Intrapleural Analgesia
This technique involves injection of anesthetic agent into the pleural cavity through a pleural catheter or through an existing thoracostomy tube. Introduction of a catheter runs the risk of creating a pneumothorax, whereas injection through an existing chest tube may warrant the tube to be clamped which can result in the development of a tension pneumothorax. For these reasons, intrapleural analgesia has not been a very popular modality of pain relief.
Thoracic Paravertebral Block
This modality involves injection of anesthetic agent into the paravertebral space. Though it has a few advantages with respect to a lower incidence of hypotension and easier technique in comparison to EA, it is not much preferred due to lack of evidence regarding the benefit of this technique.
Nonsteroidal Anti-inflammatory Drugs
When used alone, they are not good for pain relief in thoracic trauma. However, they are of immense importance when used in conjunction with opioids, as they reduce the dose needed for effective analgesia. Increased risk of coagulopathy, gastritis, and platelet dysfunction are factors unfavorable for their use in trauma.
Newer Modalities of Pain Relief
A multimodal approach using concomitant use of multiple agents is preferable as a single agent leads to an unacceptable side effect profile. There cannot be a standardized protocol for choice of analgesic agent. It needs to be individualized based on factors such as site of involvement, number of ribs fractured, age, and accompanying thoracic and extrathoracic injuries.
Fluid Therapy
The landmark results from Trinkle et al. [12], in 1975, revolutionized the management of flail chest. They emphasized the damage from excessive fluid therapy which worsened the already contused lung. The management protocol devised by Trinkle et al. [12] included:
1.
Restriction of IV fluids to less than 1,000 ml during resuscitation and 50 ml per hour thereafter.
2.
Lasix 40 mg given intravenously immediately upon admission and daily for 3 days.
3.
Salt-poor albumin 25 g (100 ml) given daily to maintain plasma oncotic pressure.
4.
Blood loss replacement only with plasma or whole blood, or a combination of these, not with crystalloid solutions.
This sets the trend for increasing use of colloids rather than crystalloids to reduce lung edema. Animal studies have reiterated this approach [13].
The use of colloids in intensive care has undergone a periodic change from the safe trial [14] suggesting albumin to be safe to the CHEST trial [15] which concluded that starch (hydroxylethyl starch) increased mortality. Fluid restriction to an absolute volume is also not recommended to prevent hypoperfusion and organ damage. Dynamic assessment of intravascular volume status using stroke volume variation, pulse pressure variation, inferior venacaval collapsibility index and passive leg raise is routinely used in the ICU to judge fluid administration. The emphasis now is on preventing fluid overload rather than fluid restriction or on the choice of fluid.
Ventilation
Fundamentals of ventilation in flail chest: Management of flail chest underwent a transition when external splinting using adhesives and bandages gave way to internal pneumatic stabilization with the advent of mechanical ventilation [16]. The aim of treatment was based on the myth that spontaneous respiratory effort would increase the paradoxical movement, thereby increasing respiratory insufficiency. Hence, management of flail chest without prolonged mechanical ventilation and often tracheostomy was considered to be fatal [17].
In animal models, it was clearly shown with electromyographic evidence that there was increased force generated by external intercostal muscles, the most important for spontaneous inspiration. Therefore, cranial movement of a flail segment was not affected even when there was paradoxical inward movement in the anteroposterior dimension [18]. The mechanics of respiration were thus not much affected.
Trinkle et al. were the first to elaborately prove that associated parenchymal injury, if dealt with efficiently, would yield good results even in the absence of ventilation [12]. Shackford et al. demonstrated that ventilation increased mortality and suggested that it should be used only to correct gas exchange abnormalities rather than chest wall instability [19]. The strongest proponents of internal pneumatic stabilization also agree on the fact that prolonged continuous positive pressure ventilation using deep sedation and muscle relaxants has a role only in anterior rib fractures. For posterolateral fractures, ventilation cannot prevent the flail segment from falling back on the lung parenchyma and increasing the damage [20].
Mode of ventilation: Avery et al. introduced the concept of invasive mechanical ventilation (IMV) as a mode of stabilizing the chest wall in comparison to external surgical fixation [16]. However, the concept of prolonged ventilation with complete cessation of any spontaneous effort by using muscle relaxants and requirement of tracheostomy was not very appealing. Antonelli et al., for the first time, compared invasive with noninvasive ventilation (NIV) and showed no benefit of the former for mortality, while NIV reduced the incidence of serious complications and shortened the ICU stay [21]. Tanaka et al., using historical controls treated with IMV, compared the efficacy of NIV in patients with flail chest and found that the latter reduced the incidence of pulmonary complications and lowered the need for IMV [22]. The prospective controlled trial by Gunduz et al. reiterated that NIV caused fewer deaths (7 Vs 4) and pulmonary complications (10 Vs 4) in comparison to intermittent positive pressure ventilation IPPV. Oxygenation was poorer in the first 48 h in this group, probably due to difficulty in adjusting to the interface and pain. However, there was no need to intubate any patient on this account [23]. A recent systematic review and meta-analysis comparing NIV in chest trauma concluded that NIV did not have a mortality benefit. However, NIV significantly improved oxygenation, reduced serious complications and reduced need for invasive mechanical ventilation [24].
The positive airway pressure delivered keeps the airway open and prevents chest wall distortion, and positive end-expiratory pressure (PEEP) prevents collapse and atelectasis. This improves gas exchange and reduces respiratory insufficiency. Gunduz et al., while comparing continuous positive airway pressure CPAP to IPPV, found better chest wall stability with CPAP. The high flows of 80–100 l/min causing positive pleural pressure and minimal load of the high gas flow system help sustain the chest wall stability [23].
Contraindication of NIV: NIV would be contraindicated in instances where the interface between face and mask would be harmful or the positive pressure would be deleterious. This would include the following:
1.
Apnea
2.
Shock
3.
Faciomaxillary injury
4.
Head injury
5.
Esophageal injury
6.
Low sensorium
7.
Excessive airway secretion and poor cough
The use of NIV warrants close monitoring and repeated bedside evaluation of the patient for early recognition of worsening respiratory insufficiency and need for intubation.
Indication for IPPV: It is now indisputable that routine use of IPPV is not needed in the management of flail chest [12]. IPPV is indicated based only on clinical criteria. Richardson et al. [25] outlined clinical criteria for intubation and use of IPPV while evaluating the efficacy of selective management of flail chest and pulmonary contusion. These were:
1.
Hypoxia and respiratory distress
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree