Introduction
Medical standards are applicable to a number of occupational groups. Some of these are voluntary codes of practice, some statutory. The police and armed forces are examples, as is the offshore oil industry. Employers have a duty of care to protect employees from harm as well as guarding against medical conditions which may have a detrimental effect on performance in the workplace. Likewise, employees have an obligation to indicate any medical condition which might erode ability in the discharge of duty.
Medical standards exist for all transport modalities including roads, railways, shipping and in the air to protect both the individual as well as third parties. The development of these standards was initially empiric rather than evidence based. This no longer applies to aviation, and to some extent to road transport, both of which have based their fitness requirements on risk of event. As it is impossible in one short chapter to review the evidence base for the breadth of cardiologic standards across the workplace, it is intended to consider road and, more specifically air transport as examples of the application of evidence-based medicine (EBM) to achieve the twin goals of safety and good practice.
Passenger transportation does not have to be completely safe and the controling legislation does not require it to be so. It has to be “safe enough.” It is self-evident that the good conduct of a means of transport requires it to be fit for purpose. Design, construction, maintenance and operation should be sound and reliable. This implies the need for regulation. The concept of safety criticality suggests that the consequences of failure of any aspect of the envelope need to be identified, minimized and tolerable in the operational environment. Sometimes systems are duplicated (redundant) but not always if a sufficiently low target failure rate can be achieved without. How, then, can these targets be identified and met?
People operate motor cars, railway trains and aircraft and may fail due to health or other considerations. This event rate, like the vehicles they operate, can be to some extent predetermined. Age makes a contribution. Decrement in human function or performance may be associated with sudden catastrophic failure or subtle, with gradual loss of efficiency. The safe operation of a system of transportation involves a level of medical fitness of those responsible for the lives of others.
Operational standards (including medical standards) in civil aviation are agreed by international statute1 and are implemented by national agencies (e.g.. the Civil Aviation Authority (CAA) in the UK). There may be additional supranational oversight (e.g.. the European Aviation Safety Agency (EASA)). There are also agreed European standards for the regulation of driving, including medical standards.2,3 Medical fitness to fly and to drive has been swept up into the legal frameworks of the Western world, and elsewhere. Some medical conditions are inconsistent with driving or flying status and an adverse decision may terminate employment. Some cardiologic conditions such as coronary artery disease, on account of their large outcome databases, lend themselves to risk modeling. Others such as atrial fibrillation, due to symptomatic capriciousness, are more difficult. And there are orphans such as the long QT syndrome where risk stratification is based on slender outcome data, but where decisions still have to be taken. Third-party safety takes precedence but best practice is paramount to avoid the adoption of clinical courses of action solely for the purpose of the preservation of employment. The need for good governance in the decision-making process requires no further emphasis.
Modes of transport and regulation
Regulation got off to an early start and in 2500 years BC the Cretans required maintenance and loading inspection of their ships, a practice which was revived in Europe in the Middle Ages. It was not until 1894 in the UK that the load line on a ship was made law in an attempt to reduce the number of vessels and crews lost from overloading. In 1930 international agreement was achieved. In Europe, the development of the European Union led to a harmonization process for all land (and air) based activities. This was to include competition, taxation (inevitably), safety and technical requirements, track rules and signaling, where appropriate. The endpoint was to be interoperability of road and rail across the continent. Currently 1.2 million lives are lost in road transport accidents each year, with some 0.5 billion injuries, worldwide. Although observational data are scarce, medical incapacitation accounts for only 0.1% of road traffic accidents of which some 25% may be attributed to cardiologic causes.4 Historically, but with certain exceptions, the railways have had the best safety record on land.
Aviation also has an impressive safety record and is tightly regulated. In 2006, 2.1 billion passengers were carried in some 35 million scheduled and non-scheduled flying hours for the loss of 863 passengers. The average sector length is now 2 hours. This has doubled in the last 30 years. Aviation is the only system of mass transportation that is regulated by international statute. All contracting states have treaty status with the International Civil Aviation Organization (ICAO), a safety directorate of the United Nations Organization. All are bound to maintain the standards in Annex 1 to the Convention on International Civil Aviation (ICAO Annex 1).1 The Standards and Recommended Practices (SARPs) are promulgated in Annexes to the Convention and are regularly updated. The Standards are safety directed and obligatory. Recommended Practices are not so binding.
The ICAO cardiologic Standard is enshrined in eight brief paragraphs but may be interpreted by “accredited medical conclusion” to permit ongoing licensing provided flight safety will not be jeopardized. ICAO also publishes guidance material. In Europe and elsewhere, an operational multi-crew limitation (OML) may be imposed to prevent a pilot from flying on single-crew operations if the risk of medical (cardiologic) event is perceived as too high.
The Joint Airworthiness Authorities framework in Europe was set up in 1970, later becoming the Joint Aviation Authorities (JAA). The medical standards in the Joint Aviation Requirements FCL part 3 Medical5 related guidance material were the first comprehensive approach, worldwide, to provide a written protocol. The cardiologic standards originated from four cardiologic workshops6–9 specifically tasked to the interface with aviation. These have been amplified in the UK by a series of algorithms showing pathways of problem management which guide medical fitness and certification. This material has been adopted outside Europe but has no regulatory status elsewhere. The EASA10 is the legally based successor to the JAA. Within the curtilage of this chapter, the terms certificate and license (to fly) are used synonymously whilst fitness indicates fitness to fly. The class 1 certificate relates to professional aircrew and the class 2 certificate to private pilots These are regulatory terms and should not be confused with classes of recommendations and levels of evidence as used in this book.
Aviation accident experience due to medical cause
Eighty percent of fatal aircraft accidents are attributable to “human factors.” One-third of airline pilots admit to some level of incapacitation whilst on duty at some time during their career,11 most commonly due to gastroenteritis. Significant medical cause incapacitation is rare, mainly because such events are rare in the population of pilot age (<65 years for professional pilots). Subtle incapacitation (see above) leading to error may be as important as complete incapacitation. It can be caused by illness, fatigue or the effects of medication. Routine medical scrutiny, which includes resting electrocardiography, identifies a few of those at increased risk of cardiologic mishap, allowing intervention, e.g. hypertension, diabetes. Alternatively, problems may present spontaneously, e.g. myocardial infarction, stroke. Notwithstanding, the UK license loss from cardiovascular cause remains low at <0.1%/thousand professional license holders per annum.
There were 29 airline accidents, worldwide, attributable to medical incapacitation during the years 1946 – 1985. There were five fatal accidents attributed to acute coronary events during the years 1961 – 1968.12–14 In 1972 the HS Trident G-ARPI (known as Papa India) crashed 150 seconds into its flight when it stalled due to premature retraction of a leading edge lift device. This fatal error was attributed in part to incapacitation of the captain by an acute coronary event. One hundred and eighteen people died.15
In the aftermath of the Papa India disaster a number of initiatives were taken nationally and internationally. The ICAO required regular incapacitation training of multi-crew pilots; flight deck voice recorders were also mandated. Some well-travelled cardiologists were so shaken by the event that the American College of Cardiology16 and the Royal College of Physicians of London17 called for increased cardiologic scrutiny of pilots. This was to include exercise electrocardiography. But middle-aged otherwise fit males have a low probability of fatal/non-fatal coronary event and this recommendation was not evidence based in safety terms, nor justifiable in (Bayesian) terms of conditional probability. Had exercise electrocardiography been adopted it would have led to many more pilots being investigated for disease they did not have (false-positive responders) than those who did (true-positive responders). And, as an investigation for coronary artery disease, exercise electrocardiography is only 60 – 70% sensitive in the asymptomatic middle-aged male.
The Papa India disaster is the worst UK aviation accident to date. The pilot population at the time was relatively old and there was no crew training for recognition of incapacitation of a colleague. Following the accident, pilots were subsequently reviewed more rigorously but inconsistently as there were no agreed protocols of review. Since 1974, improved crew training, better cockpit resource management, better safety systems and better aircraft design have all contributed to the exceptional safety levels which are now being achieved in multi-crew (more than one pilot) airline operations. There have been almost no accidents/ incidents attributable to pilot incapacitation in the 2/3 billion hours flown since, in spite of deaths and incapacitations which have continued to occur whilst aircrew are on their duty period.
Evidence-based medicine and workshops in aviation cardiology
Pre-empting Sackett et al18 by nearly two decades, it was evident that there was a need for an authoritative overview of the evidence base on the presentation, natural history, outcome and impact of intervention on the common, and sometimes not so common, cardiologic conditions to make regulatory decisions more scientific, objective and fair. This led to the four workshops in aviation cardiology which took place between 1982 and 1998.6–9 They followed the same pattern. Twenty-five cardiologists and epidemiologists who were leaders in their field, together with directly relevant specialists, were tasked to produce position papers on chosen topics. This resulted in one of the most comprehensive statements available on cardiologic problems and aircrew certification available at the time, or since.
Devereaux et al19 produced a Venn diagrammatic model for the evolution of evidence-based clinical decisions. The key elements include research evidence, patient preferences and actions, the clinical state and circumstances, with clinical expertise being in the command or “overarching” position. In the regulatory environment an extra dimension is introduced. Transport safety is concerned with the probability of an incapacitating event in the operator but the decision to grant medical fitness is a binary one. The subject is either fit or unfit for the task with the exception of a detente where there is an OML. There are, therefore, potential conflicts between patient choice and the boundaries of regulation.
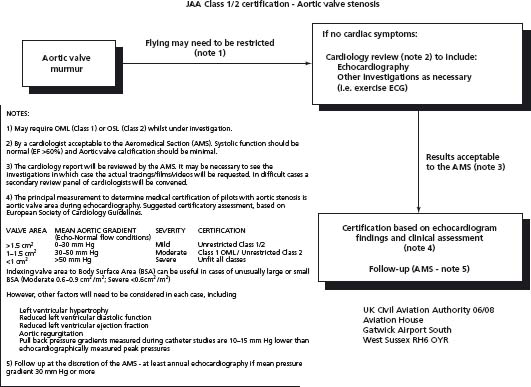
The regulator is not the pilot’s physician and must play no part in clinical management. Certain clinical choices may deny subsequent fitness – the use of a mechanical valve in the management of aortic stenosis in a pilot, for example. The clinical indication for warfarin in this context is associated with fitness denial at present in Europe on account of the summative risk of bleeding from the treatment and the risk accruing from the underlying pathology. Thus although the thromboembolic rate of the tissue and mechanical valves in the aortic position is comparable, the risk of bleeding in the patient with an anticoagulated mechanical valve is significantly higher,20 exceeding the target event rate (see below). The choice of a tissue valve may, however, be agreed between the patient and his/her cardiologist in spite of its long-term poorer performance20 without pre-emption towards regaining flying status. This represents operation of the fourth dimension in Devereaux’ s Venn diagram. The decision to replace the valve will have been a clinical one,21 assuming that the pilot with aortic stenosis was asymptomatic. Provided the UK CAA algorithm (Fig. 7.1), for example, can be subsequently navigated successfully, a favorable fitness statement should be possible.
Figure 7.1 Algorithm for certification to fly following the diagnosis of aortic stenosis. The cut-off points relate to the hierarchy of increasing risk assumed by reduction in valve area, and the prognostic implications of the presence of valvular calcification, left ventricular hypertrophy and the presence or absence of reduced left ventricular ejection fraction (Class I). Note that in the regulatory process, the terms “Class 1” and “Class 2” refer to the level of fitness assessment for professional and private aircrew respectively.
The “1% rule” and best evidence
Although the workshop proceedings were to become manuals of regularly updated informal guidance material, their ground-breaking contribution was the evolution of what was to become known as the “1% rule.” Credit is due to Tunstall-Pedoe22,23 who related the chance of “failure” of a pilot in medical terms to the risk of failure of any major system in the aircraft. It is derived as follows: the industry target fatal accident rate for large jet aircraft is 1 in 10 million flying hours. Not more than 1 in 10 of such events should be due to a major system failure (i.e. the pilot) and not more than 1 in 10 of those due to failure of a subsystem (i.e. medical incapacity). This makes for an objective of 1 fatal accident in 1000 million hours from all-cause medical incapacitation.
This target will be met provided the all-cause crew medical failure rate does not exceed 1%/annum – the approximate cardiovascular mortality of a 66-year-old male in North West Europe. This is argued as follows: there are 10 000 hours in a year (actually 8760 hours). If incapacitation occurs at 1% each year, the risk in any one hour will be 1 in 100 × 10 000 – 1 in 1 million. But there are two crew members and only 10% of the flight is critical (take off, climb out, approach and landing) and with adequate training (based on simulator data) only 1 in 100 such incidents will lead to an accident.
Thus the medical incapacitation of one of the two crew members should not lead to an accident more often than 1 in 1 million 1 in 10 × 1 in 100, i.e. 1 in 1 000 million hours. This coincides with the industry target for an unpredicted total loss which experience has shown to be realistic and appropriate. The chance of both pilots suffering medical incapacitation in the same hour will be the square of the individual risk (1 in 1 million × 1 in million – 1 × 1012) which is extremely remote. The carriage of two pilots should, therefore, guarantee safety in all but the most adverse circumstances. In contrast, the single-pilot operation is uniquely vulnerable.24,25
In modeling the 1% rule, total cardiovascular mortality and coronary artery mortality were used as these are the most easily defined endpoints in the expression of cardiovascular risk. Co-morbid, non-lethal events, including stroke and unstable angina, will be 2 – 3 times as common but in the regulatory environment, screening by self-declaration following event will have removed some of this risk. Thus a 1% mortality in the general population is equivalent to a 1% event rate in the regulatory environment.23
Further development of the rule by Mitchell and Evans26 has suggested that the target event rate could be relaxed to 2% for multi-crew operations without appreciable increase in risk to flight safety. This they based on a number of factors including reduced relative flight criticality brought about by longer flight duration and better equipment. Furthermore, since the late 1970s, cardiovascular mortality in the UK has fallen 46%27,28 in the under-65 year age group but in actuarial terms this risk reduction is “lost” in 3 – 4 years.29,30 In other words a subject’s “cardiologic age” at somatic age 64 years, now, is the equivalent of what it used to be at age 60, 25 years ago. Partly as a result of this, the age of professional pilot retirement from passenger-carrying operations has been increased from 60 to 65 years.
The impressive safety achievement in multi-crew operation is impossible in single-crew operations where the whole flight is critical in the context of pilot “failure” from any cause, including medical. In this environment the fatal accident rate due to failure by the single crew member will always be significantly worse than the medical incapacitation rate. The chance of being killed as a passenger in a single-pilot machine from any cause is likely to be one or two orders of magnitude ([mult]10 – 100) greater than in the multi-crew operation.
The foregoing arguments are predicated on the aviation environment but the principles are applicable elsewhere. In road and rail transportation, with a single crew operator, there may be sufficient warning of illness to permit safe conduct of a machine to a standstill. In rail transport the “dead man’ s handle” safety device is designed to stop the vehicle in the event of incapacitation of the driver. It is not universally fitted.
The 1% rule was evolved to define an appropriate cut-off point for denying multi-crew operational fitness to a pilot; it is not a yardstick for judging single crew fitness. In the context of coronary artery surgery, for example, if the predicted risk of event is < 1%/annum, the pilot may be fit for multi-crew, but not single-crew operation. With the geometric increase in risk of occult coronary artery disease with age, it is not easy to determine placement of the risk cursor with its all-or-nothing impact on certification to fly. Doubling cardiovascular risk at age 60 years will be associated with a substantial increase in absolute risk when compared with age 40 years.30
Specific cardiologic issues in aircrew
Fitness to fly has evolved significantly over the years in tandem with the diagnostic, pharmacologic and interventional progress that has been made in medicine. The boundaries of fitness are under constant review as challenges to stretch the envelope in regulatory terms are made. The interface between regulation and cardiology is as broad as the specialty itself and for this reason only two of the most common cardiologic conditions will be considered in more detail – coronary artery disease and atrial fibrillation, whilst a third, rare, condition will also be examined. A fuller treatment of the subject is available.31
Health maintenance
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


