Fig. 12.1
The position of all four members of both surgical teams and the scrub nurse for the “two-team approach” (From: Zieliński et al. [26])
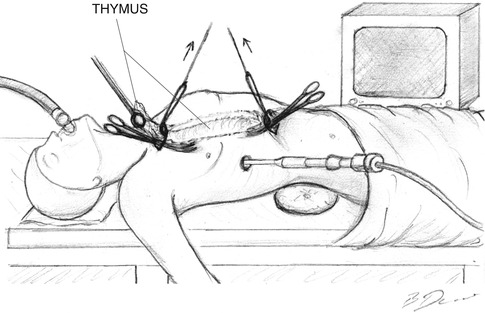
Fig. 12.2
Simultaneous dissection performed by two surgical teams
12.4.1 The Cervical Part of the Operation
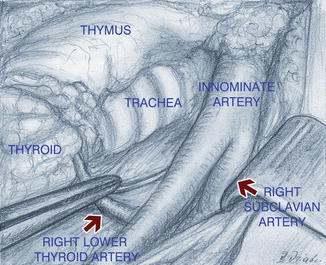
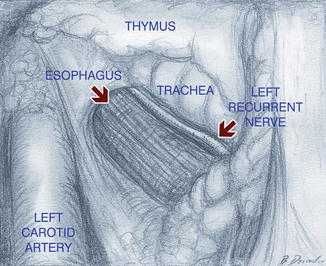
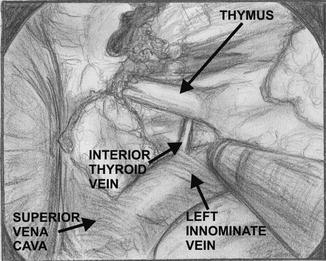
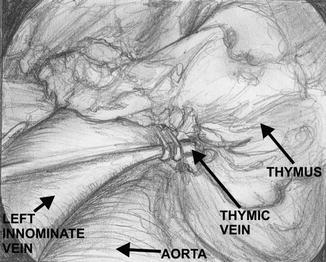
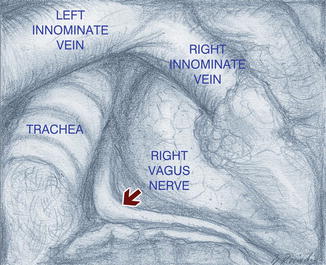
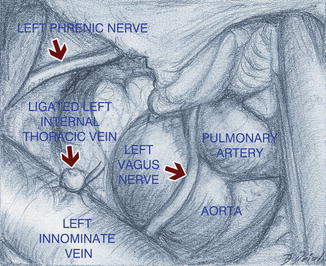
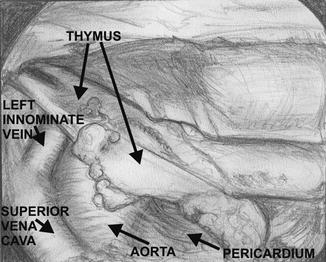
A transverse 5–8 cm incision is made in the neck above the sternal notch. The platysma and superficial cervical fascia are divided, and the anterior jugular veins are divided and suture ligated. The strap muscles are split along their median raphe and retracted laterally. The whole thyroid gland is visualized, and all foci of adipose tissue are removed downward from the level of the upper poles of the thyroid gland. The parathyroid glands and both laryngeal recurrent nerves are visualized and carefully preserved (Figs. 12.3 and 12.4). The fatty tissue containing the superior poles of the thymus is separated from the lower poles of the thyroid gland with 1–4 inferior thyroid veins ligated and divided close to thyroid gland. Alternatively, such devices as a harmonic knife, LigaSure, or vascular clips can be used to secure the vessels throughout the procedure. The thymus with the surrounding fat is then separated from the sternohyoid and sternothyroid muscles, the trachea, the internal surface of the sternum, the carotid arteries, the innominate artery, the aorta, and the right innominate vein. Finally, both upper poles of the thymus are divided close to the thyroid gland (Fig. 12.5). At this point a sternal retractor connected to the firm frame with a traction mechanism is inserted under the manubrium of the sternum to elevate it several centimeters to provide access to the anterior mediastinum. The lower thyroid veins (1–4) and the thymic veins (1–4) are dissected, clipped, and divided close to the left innominate vein (Fig. 12.6). The other option, if the two-team approach is used, is to dissect, manage with vascular clips, and divide these vessels from the chest approach, through the subxiphoid incision (Figs. 12.7 and 12.8). The fatty tissue from the area called “the aorta-caval groove” is removed. The boundaries of this space are the division of the innominate artery and the aorta (medially), the trachea (posteriorly), the right innominate vein and the right mediastinal pleura (laterally), and the right main bronchus, the azygos vein, and the superior vena cava (inferiorly) (Fig. 12.9). The dissection proceeds caudally, below the left innominate vein, and the specimen is separated from the pericardium at a distance of several centimeters. The most difficult, but very important, part of this operation when performed through the transcervical approach is the dissection of the adipose tissue from the aortopulmonary window. Further dissection of the two other branches of the left innominate vein, namely, the left internal thoracic vein and the accessory hemiazygos vein, is performed. These two veins are subsequently divided and their ends are secured with clips or sutures (preferably) (Fig. 12.10). The division of these veins provides much better access to the aortopulmonary window above the left innominate vein which is retracted toward the aorta. The next step is the visualization of the left phrenic nerve which runs very close to the left internal thoracic vein and the left vagus nerve which runs laterally to the left common carotid artery. With blunt dissection using a peanut sponge, the fatty tissue of the aortopulmonary window is dissected from these nerves, the aorta, and the left mediastinal pleura. At the bottom of the aortopulmonary window, the left pulmonary artery is visualized (Fig. 12.11). The other option, if the two-team approach is used, is to dissect the adipose tissue of the aortopulmonary window from the subxiphoid incision, without touching the left internal thoracic vein and the accessory hemiazygos vein.
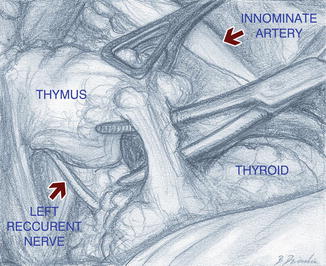
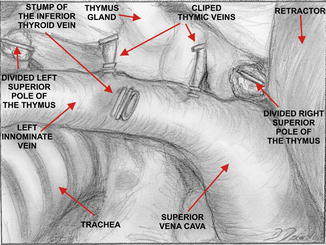
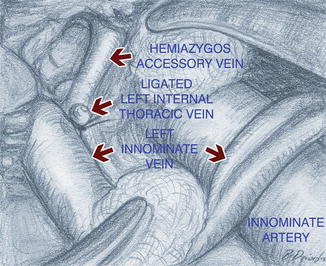
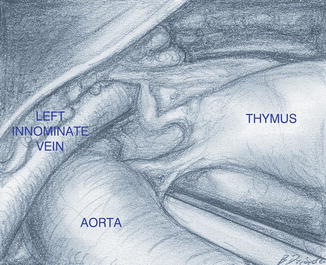
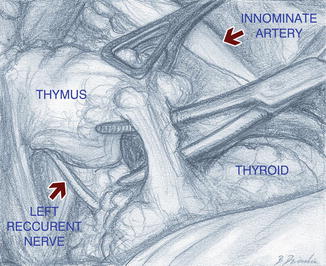
Fig. 12.5
Dissection of the left upper pole of the thymus close to the thyroid gland (From: Zieliński et al. [27])
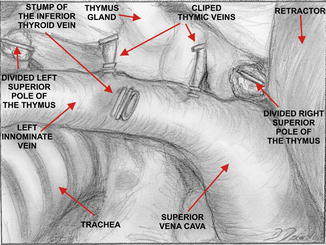
Fig. 12.6
Clipping and division of the lower thyroid veins and the thymic veins close to the left innominate vein (From: Zieliński et al. [27])
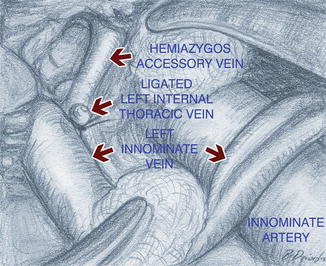
Fig. 12.10
The view on the hemiazygos accessory vein after division of the left mammary vein through the neck (From: Zieliński et al. [27])
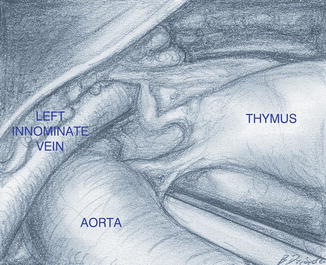
Fig. 12.13
Dissection of the thymus from the pericardium – view from the right VATS approach (From: Zieliński et al. [27])
12.4.2 The Subxiphoid Part of the Operation
A transverse 4–6 cm incision is made above the xiphoid process. The subcutaneous tissue is cut and the medial parts of the rectus abdominis muscles are cut near the insertions to the costal arches. The xiphoid process is divided transversely and left without removal. The selective left lung ventilation is started resulting in the collapse of the right lung. The anterior mediastinum is opened below the sternum. A second sternal retractor connected to the traction frame (the same as one which is used for traction of the manubrium) is placed under the sternum, which is elevated to facilitate access to the anterior mediastinum from below. A thoracoscopic port for 5 mm, 30° oblique thoracoscope is inserted into the right pleural cavity in the 6th intercostal space in the anterior axillary line. The right mediastinal pleura is cut near the sternal surface up to the level of the right internal thoracic vein which is left intact (Fig. 12.12). The prepericardial fat and right and left epiphrenic fat pads are dissected from the pericardium and diaphragm with blunt dissection, using a peanut sponge, and sharp dissection, using scissors. Dissection of the prepericardial fat containing the thymus gland proceeds upward under the control of the VATS camera with en bloc fashion, without any attempt to dissect the thymus gland separately (Fig. 12.13). The right phrenic nerve is the margin of dissection. At this moment the thymus is attached to the pericardium only with its left lower pole. Ventilation of the right lung is resumed and the ventilation of the left lung is disconnected. A thoracoscopic port for 5 mm, 30° oblique thoracoscope is inserted into the left pleural cavity, as on the right side. The operating table might be rotated on the right side with elevation of the left side which lowers the mediastinum, improving access to the left pleural cavity. Under the control of the VATS camera, the left mediastinal pleura is divided along the sternum, and the left prepericardial fat is dissected from the pericardium above the level of the left internal thoracic vein previously divided. The left lower pole of the thymus is separated from the pericardium and the specimen is removed. Dissection of the aortopulmonary window is completed, if necessary, at this stage of the operation (Fig. 12.14). Hemostasis is checked, the VATS ports are removed, and the chest tubes are inserted into both pleural cavities through the incisions made for the insertion of the ports. Ventilation of both lungs is resumed. The cervical and subxiphoid incisions are closed in the standard manner. Generally, the patient is extubated immediately after the operation.
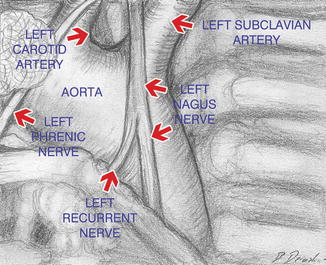
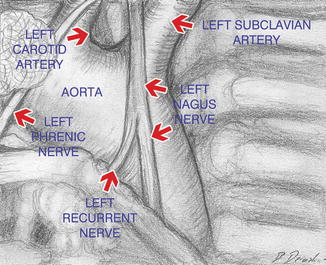
Fig. 12.14
View of the aortopulmonary window from the left VATS approach (From: Zieliński et al. [27])
12.5 Results
There were 390 patients including 315 women and 75 men. There were 383 patients with nonthymomatous MG and 7 patients with thymomas. The age of the patients was 11–69 years (mean 29.7 years). Duration of myasthenia was 2–180 months (mean 28.3 months). Osserman score was I–III. 27.3 % of patients were taking steroids or immunosuppressive drugs preoperatively. Mean operative time was 201.5 min (120–330 min) for the one-team approach and it was 146 (95–210 min) for the two-team approach (p < 0.05). There was no postoperative mortality and the postoperative morbidity was 9.2 %. The complications are listed in the Table 12.1. The incidence of ectopic thymic foci was 65.9 % overall, with localization of the ectopic foci shown in the Fig. 12.15. The rates of complete remission after 1–5 years of follow-up after three different technique of thymectomy for nonthymomatous MG including transcervical-subxiphoid-VATS maximal thymectomy are presented on Fig. 12.16 [12]. We have shown a statistically significant difference in complete remission rates and the negative results rates (lack of improvement or deterioration of myasthenia gravis in comparison to the preoperative state) between the basic and the extended thymectomy and the transcervical-subxiphoid-VATS maximal thymectomy groups after 1–5 years of follow-up, with no significant differences between the two last groups. The only explanation for such a difference in results is the technique of thymectomy, with the removal of ectopic foci of the thymic tissue in the extended thymectomy and the transcervical-subxiphoid-VATS maximal thymectomy groups.
Table 12.1




Complications in 390 patients with myasthenia gratis operated on with transcervical-subxiphoid-VATS “maximal” thymectomy
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree