Surgical Management of Empyema
Naveed Z. Alam
Raja M. Flores
Empyema, or empyema thoracis, can be defined as a purulent fluid collection in the pleural space. The etiology is varied and includes contamination from adjacent organs, most commonly the lungs, or direct inoculation by trauma or iatrogenic interventions. It is an ancient disease that often requires therapy that harkens back to ancient times.
HISTORY
Empyema thoracis was first described in the 5th century BC by Hippocrates. He wrote that the most common cause was the entrance of foreign bodies into the lungs, either by inhalation or drinking. They may also be caused by parapneumonic effusions if the chest is not cleared by expectoration within 14 days. Symptoms were described as fever, rigor, and thoracic pain and signs included copious sweating, cough, red eyes, bent nails of the hands, and anorexia. On physical examination, Hippocratic physicians asked patients to sit on a chair and then shook them. By placing their ears to the chest wall (immediate auscultation), they could hear a typical rippling sound, similar to that produced by a bottle halffilled with fluid. If no sound was heard, the empyema was noted on the side of the chest that was more swollen and painful.
Management was conservative initially, with the application of plant roots and honey as well as physiotherapy in the form of warm baths and inhalation of vapors with subsequent shaking of the patient to achieve eruption and expectoration of the pus. If this failed, then surgery was pursued. “First, cut the skin between the ribs with a bellied scalpel; then wrap a lancet with a piece of cloth, leaving the point of the blade exposed a length equal to the nail of your thumb, and insert it. When you have removed as much pus as you think appropriate, plug the wound with a tent of raw linen, and tie it with a cord; draw off the pus once a day; on the tenth day, draw all the pus, and plug the wound with linen. Then make an infusion of warm wine and oil with a tube, in order that the lung, accustomed to being soaked in pus, will not be suddenly dried out. When the pus is thin like water, sticky when touched with a finger, and small in amount, insert a hollow tin drainage tube. When the cavity is completely dried out, cut off the tube little by little, and let the ulcer unite before you remove the tube (Papavramidou).”
This remarkable treatise on the management of empyema with open tube drainage as its hallmark defined the standard of care for the disease for more than two millennia. During the world influenza pandemic of 1918 to 1919, there was a crisis. Draftees in crowded military camps were particularly susceptible to the streptococcal pneumonia and empyema that often accompanied influenza. A survey by the Surgeon General of the Army found a mortality rate of 30% for empyema drainage at base hospitals with deaths frequently occurring within 30 minutes of the procedure. This prompted the appointment of Major Evarts A. Graham to head a commission to study the problem. Dr. Graham cautioned against early drainage due to the risk of open pneumothorax and advocated operation only after the development of frank pus as this is usually accompanied by an abscess isolated from the remaining pleural cavity. He also recommended closed drainage rather than open drainage. Adoption of these changes to practice decreased the mortality rate to close to 5%.
CLASSIFICATION
Empyema follows a natural progression that has been classified by the American Thoracic Society into three distinct stages. In the exudative stage, or acute phase, the inflamed pleural membranes swell and discharge a thin effusion with associated bacterial contamination. The fluid is clear and has a low cell count. As the disease progresses to the fibrinopurulent stage, or transitional phase, deposition of fibrin occurs resulting in loculation formation and turbid, or frankly purulent, fluid. In the final stage, the organizing or chronic phase, in-growth of fibroblasts, and associated collagen fibers render the lung trapped and relatively functionless.
ETIOLOGY
As mentioned above, empyemas generally result from either contamination from a contiguous septic organ or direct inoculation during trauma or iatrogenic maneuvers. The most common cause is parapneumonic. Other contiguous sources include esophageal ruptures, deep cervical abscesses, paraspinal infections, and subphrenic collections. Rarely, hematogenous spread from distant sources can result in empyema, particularly in the immunocompromised population.
Post traumatic empyemas are associated with either penetrating injuries or the presence of a hemothorax. As the hemothorax represents an ideal growth medium for bacteria, any instrumentation of the chest cavity, particularly in less than ideal conditions, increases the risk of development of an empyema. Chest tubes inserted in nonsterile conditions, multiple reinsertions of chest tubes, excessive manipulations of chest tubes, residual blood from incompletely evacuated hemothoraces, and prolonged drainage are factors all associated with the development of empyema. Other factors in blunt trauma associated with empyema include the presence of a hemopneumothorax, suggestive of parenchymal injury and ongoing bacterial contamination of the pleural space.
Iatrogenic causes of empyema range from minor interventions, such as needle biopsies and thoracentesis, to postoperative occurrence following lung or esophageal surgery. The management of a postpneumonectomy empyema with or without associated bronchopleural fistula is particularly challenging.
BACTERIOLOGY
The spectrum of causative organisms of empyema varies somewhat with geography; hence, local data are often required to guide
therapy. In developed countries, the most common organisms isolated in adult community acquired empyema are Streptococcus milleri, Streptococcus pneumoniae, and anaerobes. In hospital-acquired empyema, Streptococcus aureus, including methicillin-resistant S. aureus (MRSA), is the most commonly isolated organism. In pediatric empyema, the most common organism is S. pneumoniae.
therapy. In developed countries, the most common organisms isolated in adult community acquired empyema are Streptococcus milleri, Streptococcus pneumoniae, and anaerobes. In hospital-acquired empyema, Streptococcus aureus, including methicillin-resistant S. aureus (MRSA), is the most commonly isolated organism. In pediatric empyema, the most common organism is S. pneumoniae.
 COMPLICATIONS
COMPLICATIONSThe complications of empyema occur with increasing likelihood as the disease progresses, with the majority developing in the chronic or organizing stage. Pulmonary fibrosis due to increased scar tissue within the lung and pleura can develop. Similarly, scarring of the chest wall and intercostal muscles can lead to contraction. Complications associated with local drainage may occur as well as the infection follows a path of least resistance to suppuration. Contiguous contamination can result in a myriad of complications. In the pursuit of the path of least resistance to suppuration, patients can develop empyema necessitatis with drainage through the skin. Alternatively, the infection can travel to the lung parenchyma, resulting in bronchopleural fistulae. Similarly, mediastinitis, pericarditis, subphrenic abscesses, and osteomyelitis of the ribs or vertebrae can develop.
RADIOLOGY
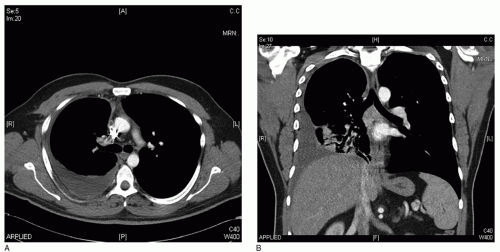
Radiological investigations facilitate diagnosis, enable planning of therapeutic approaches, and allow monitoring of progress. Ultrasound of the thoracic cavity can demonstrate septations and loculations and assist in making thoracentesis safer. Chest radiography is the first step in the evaluation of any suspected pleural pathology. Computed tomography (CT) is also very valuable in patients who do not have simple effusions. It permits visualization of the precise location of loculations, which can be helpful at the time of surgery, particularly with minimally invasive approaches.