Chapter 47 Sudden Cardiac Death
Definition
The term sudden cardiac death refers to unexpected natural death from a cardiovascular cause within a short period, generally less than 1 hour from the onset of symptoms.1 The time and mode of death are therefore unexpected.2 By definition, this occurs in individuals who do not have prior conditions that could be fatal in the short term. The use of 1 hour in this definition is arbitrary and therefore subject to different interpretations. It is also important to distinguish a primary arrhythmic cause of death from, for example, an episode of worsening heart failure that culminates in a life-terminating arrhythmia and from other causes of sudden death such as pulmonary embolism, cerebral infarction, and ruptured aneurysms. This distinction is important both for the proper identification of SCD and the study of this phenomenon. More recently, the use of the term sudden cardiac arrest (SCA, synonymous with SCD) has been advocated.
Epidemiology
SCD is a major cause of death in North America and other Western societies, accounting for 10% of all deaths and up to 50% of heart disease–related deaths.3 The incidence of SCD (emergency medical services [EMS]–assessed, out-of-hospital cardiac arrests) in the United States is generally estimated to be 95.7 per 100,000 person years.4 Approximately 60% of out-of-hospital cardiac deaths are treated by EMS personnel.5 Among these EMS-treated, out-of-hospital arrests, 23% have an initial shockable rhythm, and 31% of these receive bystander cardiopulmonary resuscitation (CPR).6 Median survival rate to hospital discharge after EMS-treated, out-of-hospital cardiac arrest with any first recorded rhythm is 7.9% and for ventricular fibrillation (VF) is 21%. However, such median statistics of survival do not reflect regional variations of community-specific survival rates. Of note, the quantification of SCD is so fraught with difficulties that no comprehensive record of all SCDs exists. Surrogate data often are used to estimate its incidence, especially in the out-of-hospital setting. This includes deaths from “coronary heart disease” and “cardiac arrest,” defined as coronary death that occurred within 1 hour of symptom onset in the out-of-hospital setting and without other probable causes of death.7
As medical interventions continue to evolve and improve, the incidence and distribution of risk factors that contribute to SCD continue to change. Although the morbidity and mortality rates of cardiovascular disease have declined in the past 30 years, much less improvement has been observed in the incidence of out-of-hospital cardiac arrests. However, the incidence of cardiac arrest with an initial recorded rhythm of VF specifically has decreased over time, which is a recent trend that reflects the overall decline in cardiac mortality.8,9 The reduction in the incidence of VF is likely multi-factorial in origin and is attributable to improvements in primary and secondary prevention of heart disease. Current epidemiologic data indicate that in developed countries, structural coronary arterial abnormalities and their consequences account for 80% of fatal arrhythmias.10,11 Dilated and hypertrophic cardiomyopathies account for the next largest group of SCD. The remainder are caused by a variety of other cardiac disorders such as congenital heart disease (CHD) and primary electrophysiological disorders.
The epidemiology of SCD in adolescents and young adults (aged 10 to 30 years) is distinctly different from that in the adult population. The incidence of SCD in this population is two orders of magnitude less than in the adult group (1 per 100,000 vs. 1 per 1000 individuals annually).12 Although coronary atherosclerosis accounts for the majority of cases of SCD in individuals older than 40 years, it is an uncommon cause in the younger age group.13 Instead, causes such as hypertrophic cardiomyopathy, myocarditis, right ventricular dysplasia, anomalous coronary arteries, Brugada syndrome, long QT syndrome (LQTS), idiopathic VF, and commotio cordis are the underlying etiologies in this group. Because some of these conditions are genetically determined, a modest age inverse relationship seems to exist in this group, with adolescents having a somewhat higher mortality risk compared with young adults.11 A unique subgroup in this younger population is composed of competitive athletes, among whom the rate of SCD currently is approximately 0.4 to 0.6 per 100,000 person-years.14,15 The large numbers of SCD and the wide range of survival rates have significant potential implications for public health; for example, in the United States and Canada, an additional 7500 lives would be saved if survival from SCD could be increased to 12%.
Mechanisms
From a clinical perspective, the causes of SCD can be divided into two broad categories: (1) ventricular tachyarrhythmias (VA) and (2) pulseless electrical activity (PEA) and asystole. The National Registry of CPR is a prospective, multi-site, in-hospital resuscitation registry sponsored by the American Heart Association. In a study using this database, of the 51,919 index arrests evaluated in 411 centers, pulseless VT was diagnosed in 7%, VF in 17%, PEA in 37%, and asystole in 39%.16 Subsequent ventricular tachycardia (VT) or VF occurred in 26% of patients with an initial documented rhythm of PEA and in 25% of patients with asystole. Thus VT or VF was seen in 44% of all adult in-hospital cardiac arrests. This must be compared with out-of-hospital cardiac arrests, where among cases of EMS-assessed cardiac arrest, the incidence of VT or VF was 13% and PEA and asystole were 33% and 47%, respectively, for cases in which the initial rhythm was unknown, not determined, or not analyzed by EMS.8 A factor that has important implications in out-of-hospital cardiac arrests (as opposed to in-hospital cardiac arrests) is the median time of 7.24 minutes from call to arrival of first advanced life support.8
Pathophysiology
In recent years, significant advances in the understanding of the mechanism of VF have taken place. Controversy exists regarding whether VF is maintained by wandering wavelets with constantly changing re-entrant circuits or by a mother rotor that consists of a sustained and stationary re-entrant circuit that, in turn, gives rise to variable, less-organized daughter wavelets spreading through the rest of the ventricle.17,18 Certain anatomic structures can serve as anchors for rotors, allowing stability within the re-entrant circuit.19 Weiss et al have reported from their studies on porcine hearts that these anatomic sites can be papillary muscles, blood vessels, Purkinje fibers, or locations near the interventricular septum.20 Studies have suggested that Purkinje fibers play an important role in the initiation of VF, whereas others have suggested that they play a role in the maintenance of VF.21,22 Predispositions to SCD may also occur at a cellular level. Ion channelopathies can initiate various electrical disturbances, ranging from torsades de pointes in LQTS to that of idiopathic VF in Brugada syndrome.1,23 Certain mutations are significant enough that their mere presence is associated with a very high risk of SCD. However, other mutations (e.g., the recessive long QT mutation in the HERG gene) may, by themselves, be insufficient to cause SCD but may predispose patients to torsades de pointes in the presence of other factors such as drugs that prolong the Q-T interval.
The role of ischemia as an initiating factor for ventricular arrhythmias has been extensively investigated and is particularly relevant because it is a frequent etiology implicated in SCD. Ischemia causes acute changes at the cellular level that alter local conduction velocity and refractoriness. The resulting dispersion of conduction and repolarization establishes an environment that is ripe for re-entry. In animal experiments, within the first few minutes after coronary occlusion, an arrhythmogenic period that slowly abates after 30 minutes has been observed. These first 30 minutes can be divided broadly into the first 10 minutes, during which the changes are caused by direct ischemic injury, and the second 20 minutes, during which either arrhythmogenicity occurs because of either reperfusion or the evolution of injury in the various layers of the myocardium.24,25 Local changes occur in the ischemic myocardium; these include decrease in local tissue pH to less than 6, increase in interstitial potassium (K+) levels to greater than 15 mmol/L, increases in intracellular calcium (Ca2+), and other neurohormonal changes. All these factors contribute to the altered electrophysiological properties of tissue, including slowed conduction velocity, reduced excitability and prolonged refractoriness, reduced cell-to-cell coupling, and even spontaneous electrical activity.26 In addition to the local micro–re-entrant and macro–re-entrant circuits that may be generated, regional increases in automaticity and triggered activity also occur because of afterdepolarizations.
Disease States Leading to Sudden Cardiac Death
Because the majority of cases of SCD result from CAD, it is not surprising that the risk factors for SCD mirrors those of CAD. The incidence of SCD increases with age and is more common in men than women.27 The incidence of SCD tends to be higher in whites than in other racial groups. Classic coronary risk factors have been noted to be associated with SCD in various studies such as the Framingham Study and the Paris Prospective Study. These risk factors include hypertension, diabetes, high cholesterol levels, smoking, lack of regular exercise, and structural changes such as left ventricular hypertrophy.28–31 These factors are prevalent but are limited by their moderate individual positive predictive value. Left ventricular dysfunction has been shown to be a strong independent predictor of SCD in both ischemic and nonischemic cardiomyopathies. Of note, in patients with severely decreased left ventricular function and advanced heart failure, competing causes of SCD such as electromechanical dissociation and asystole exist.
Observations from population-based studies demonstrate a marked increase in the risk of SCD in first-degree relatives of SCD victims. In a study from Seattle, first-degree relatives of patients with SCD (before age 65 years) had 2.7-fold higher risk of SCD compared with age-matched and gender-matched controls after adjustment for risk factors.32 A Dutch case-control study demonstrated that patients with VF during myocardial infarction (MI) are more likely to have a family history of SCD than those with MI but no VF.33 Polygenic traits leading to SCD and monogenetic SCD syndromes such as LQTS, Brugada syndrome, hypertrophic cardiomyopathy, and arrhythmogenic right ventricular dysplasia contribute to the genetic component of SCD.34 More recently, research has begun to elucidate the role of newly identified genetic variations at the population level.
Coronary Artery Disease
Approximately 80% of patients who experience SCD have coronary atherosclerotic arterial disease as an underlying substrate. In survivors of SCD, critical flow-limiting coronary stenoses are found in approximately 40% to 86% of patients, depending on the age and gender of the population.29,30,35 Although less than 50% of the resuscitated patients have evidence of an acute MI, autopsy studies have revealed that a recent occlusive coronary thrombus can be found in 20% to 95% of victims of SCD.31,36,37 The temporal pattern of SCD closely parallels the patterns of MI and acute ischemic events. In addition, healed infarctions are found in 40% to 75% of hearts of SCD victims at autopsy.36,38–40 The extent to which superimposed acute ischemia plays a role in the pathogenesis of SCD is unclear in patients who do not develop enzymatic or electrocardiographic evidence of an acute MI. However, rapid fibrinolysis of a ruptured plaque could occur such that no visible evidence remains at autopsy. Similarly, cholesterol-laden plaque could conceivably rupture and embolize microscopic debris into distal coronary vessels that could lead to microscopic necrosis and ventricular arrhythmias and yet not be visible at autopsy.41 Because the vast majority of patients die within minutes of onset of symptoms, histologic or enzymatic evidence of ischemia or infarction may be difficult to ascertain. In addition to the most common forms of CAD, nonatherosclerotic CAD includes congenital malformations such as anomalous origin of coronary arteries; inflammatory arteritis also can lead to SCD. These disorders typically manifest early in life but are relatively uncommon.
Dilated Cardiomyopathy
Idiopathic dilated cardiomyopathy accounts for approximately 10% of cases of SCD in the adult population (Figure 47-1). Depending on the severity of the myopathy, the annual incidence can range from 10% to 50%.36 Bundle branch reentrant VT appears to represent an important cause of VAs in this population.37 However, as the myopathy progresses and congestive heart failure worsens, the incidence of VT or VF decreases, and the primary terminal event more frequently becomes electromechanical dissociation or asystole.42 As with ischemic heart disease, the overall left ventricular ejection fraction (LVEF) is an important prognostic factor. Worsening New York Heart Association (NYHA) functional class and the occurrence of syncope are both important clinical prognostic factors for SCD in patients with dilated cardiomyopathy.40
Hypertrophic Cardiomyopathy
Hypertrophic cardiomyopathy (HCM) is now regarded as the most common cause of SCD in young people, including competitive athletes (Figure 47-2).43–45 The annual mortality rate in patients with HCM in select regional and community-based cohorts is thought to be approximately 1%. The architectural myocardial fiber disorganization, scarring, and the presence of microvascular disease likely account for the proarrhythmic substrate. The conventional risk factors for HCM assume greater weight in patients younger than 50 years and include family history of one or more HCM-related form of SCD, more than one episode of unexplained recent syncope, massive LVH (thickness ≥30 mm), nonsustained VT on 24-hour Holter monitoring, and hypotensive or attenuated blood pressure response to exercise. Although implantable cardioverter defibrillators (ICDs) for primary prevention in this population usually require meeting at least two of these criteria, the need for ICD interventions for VT or VF in patients with single risk factors must be kept in mind when deciding about ICD implantation in this population.46 Of the above criteria, nonsustained VT and blood pressure response have poor positive predictive value.47 It has recently been demonstrated that certain mutations such as nonsarcomeric LAMP2 cardiomyopathy, double sarcomere mutations, and delayed enhancement on cardiac magnetic resonance imaging (MRI) are associated with SCD.48–51 Conversely, the apical variant of hypertrophic cardiomyopathy has been demonstrated to carry a relatively lower risk for SCD.52
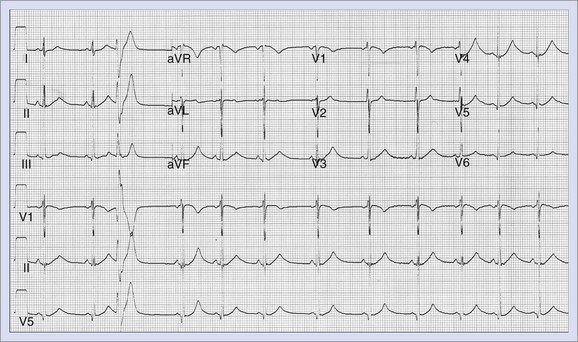
Long QT Syndrome
LQTS (Figure 47-3) is a primary cardiac arrhythmogenic disorder typically characterized by prolongation of the Q-T interval corrected for heart rate (QTc) and abnormal T waves. Subjects with LQTS may present with a nearly normal electrocardiogram (ECG) or with a prolonged Q-T interval. The syndrome is associated with a specific ventricular arrhythmia called torsades de pointes and often presents as recurrent syncope. Hundreds of mutations have been identified, and these have been described in up to 12 genes.47 This is most often caused by decreased outward K+ current, IKs (LQT1, LQT5) or IKr (LQT2, LQT6), or by enhanced activity of mutant inward sodium (Na+) current (LQT3). Polymorphic VT associated with a prolonged Q-T interval is believed to be initiated by early afterdepolarizations (EADs) in the Purkinje system and maintained by transmural re-entry in the myocardium. Clinical presentations vary with the specific gene affected and the specific mutation. Some patients with LQTS mutations may not manifest any phenotypic abnormality. In high-risk LQT1 and LQT2, patients should be routinely managed with β-blockers as a first line-therapy and should be referred for primary ICD implantation if they become symptomatic during therapy or when compliance or intolerance to medical therapy is a concern.53 Patients with LQT3, those with frequent and recent syncope, those with excessive Q-T prolongation (>550 ms), and women with LQT2 and a QT interval greater than 500 ms may be at increased risk and may require ICD implantation.
Congenital Short QT Syndrome
Congenital short QT syndrome (SQTS) is a relatively recently described disorder characterized by a very short Q-T interval (<320 ms) and a susceptibility to atrial fibrillation (AF) and VF. At electrophysiology study, short atrial and ventricular refractory periods with easily inducible AF and polymorphic VT have been identified. Gain-of-function mutations in genes encoding K+ channels have been identified, which explains the abbreviated repolarization seen in this condition. The suggested treatment is ICD implantation. The ability of quinidine to prolong the Q-T interval has the potential to be effective pharmacological therapy.54
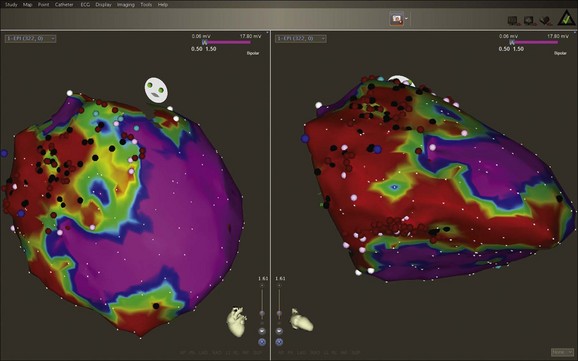
Arrhythmogenic Right Ventricular Cardiomyopathy
Arrhythmogenic right ventricular cardiomyopathy (ARVC) is a progressive, heritable myocardial disorder with a broad phenotypic spectrum that can present with VT, SCD, or both (Figure 47-4). The classic form of the disease has an early predilection for the right ventricle, but left-dominant and biventricular subtypes have been also recognized.55 Desmoplakin and plakophilin-2 are two desmosomal genes that have been implicated in ARVC. A familial form, originally described in people living on the Greek island of Naxos, can present with cardiomyopathy in association with palmo-plantar keratoderma (Naxos disease) and is caused by a defect in the gene for a cellular structural element, plakoglobin.56 ARVC causes progressive fatty replacement of the ventricular wall. Cardiac MRI is a highly sensitive imaging tool to identify the presence and degree of fatty infiltration in the myocardium; however, because this is not specific, formal criteria have been proposed for the diagnosis of ARVD. Phenotypic heterogeneity and the nonspecific nature of its associated features complicate clinical diagnosis, which often requires multiple tests rather than a single test.57 The Revised Task Force criteria for the diagnosis are specific and have helped reduce diagnostic ambiguity, but the sensitivity is low, especially in the “concealed” phase of ARVC.57
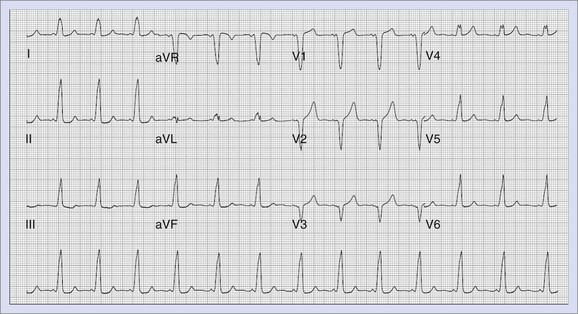
Brugada Syndrome
Brugada syndrome is associated with right ventricular conduction delay and ST elevation in the right precordial leads, characterized by syncope and premature SCD caused by VF (Figure 47-5). This syndrome appears to be responsible for a sudden death syndrome seen among Southeast Asian men.58,59 ECG manifestations of the syndrome can often be dynamic. Typical ST-segment changes, if absent at baseline, can be revealed by administration of sodium channel–blocking agents such as ajmaline or procainamide. Mutations in the SCN5A gene cause loss of function in the Na+ current Ina that can lead to accentuation of unopposed Ito currents in the right ventricular epicardium. This leads to loss of the action potential “dome,” resulting in heterogeneity of repolarization, and phase 2 re-entry that precipitates VT or VF. The strategy for risk stratification in Brugada syndrome is controversial with respect to the role of electrophysiology testing in patients who do not present with SCD. ICD is the only treatment with demonstrated efficacy in Brugada syndrome. In general, ICD implantation is recommended for patients with symptoms and for asymptomatic patients with inducible ventricular arrhythmias, especially if they have a spontaneous type I ECG pattern. In asymptomatic patients without a family history of SCD and whose type I ECG pattern is documented only after the administration of sodium channel blockers, periodic follow-up is recommended, but an EPS for risk stratification is not required.60,61 The role of EPS, however, still remains controversial, with some studies not supporting its role in risk stratification.57
Wolff-Parkinson-White Syndrome
Wolff-Parkinson-White (WPW) syndrome can lead to SCD if the accessory pathway is able to conduct rapidly in the antegrade direction in the presence of rapid atrial arrhythmias such as AF (Figure 47-6). More recently, a long-term follow-up of patients with WPW syndrome reported a mortality rate of 0.02% per year.62 Two additional studies with more than 4000 patient-years of follow-up, estimated mortality rates at approximately 0.05% per year.63,64 However, a study from Italy that prospectively followed up patients with WPW syndrome for 3 years, recorded a much higher event rate (defined as death or potentially lethal arrhythmia recorded on monitoring) at 0.5% per year.65 Predictors for the development of VF include rapid ventricular response during induced AF, with the shortest R-R interval of less than 240 ms and short antegrade pathway refractory periods. High-risk and symptomatic patients are treated with catheter ablation with very high success rates overall.66
Catecholaminergic Polymorphic Ventricular Tachycardia
Patients with catecholaminergic polymorphic ventricular tachycardia (CPVT) can present with exercise-induced syncope, SCD, or both in the absence of any structural heart disease or prolonged Q-T interval. Inheritance can be autosomal dominant or recessive. These patients often have normal resting ECGs, which makes the diagnosis difficult. Stress-related bi-directional VT has been described classically, but patients can present with polymorphic VT or even frequent ventricular ectopy. Responsible mutations have been shown to reside in the cardiac ryanodine receptor and calsequestrin genes.67–70 Treatment modalities include ICD placement along with β-blocker therapy for symptomatic patients.
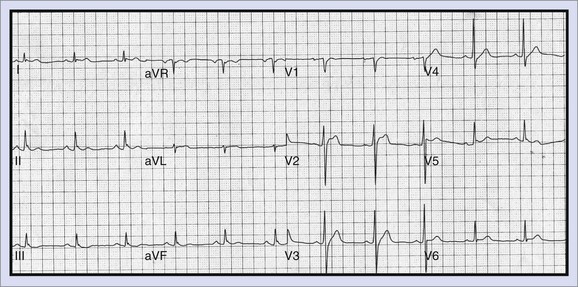
Early Repolarization
A multi-center study recently documented an association between idiopathic VF and the presence of early repolarization (ER) abnormalities in inferolateral leads (Figure 47-7).71 Repolarization changes have also frequently been observed in inferolateral precordial leads in patients with Brugada syndrome, mimicking the abnormalities typical of the population presented in the study of Haïssaguerre et al, suggesting a possible overlap of these conditions.72 This subset of idiopathic VF continues to be further studied and, in addition to ICDs, newer therapies such as quinidine and isoproterenol have been noted to play a role in controlling VF storms that can occur in these patients.
Congenital Heart Disease
Patients with CHD represent an anatomically heterogeneous patient group in which risk stratification can be difficult. Current guidelines indicate ICD implantation for survivors of SCD; ICD is considered a reasonable therapy for patients with sustained VT that is not amenable to either ablation or surgery and for those with unexplained syncope and impaired ventricular function. Tetralogy of Fallot (ToF) represents one of the commonly encountered conditions in adult CHD patient populations. Older age at surgery, residual hemodynamic lesions with right heart failure, impaired LVEF, complex ventricular ectopy, inducible ventricular arrhythmias at EPS, and prolongation of the QRS complex represent some of the associations noted in SCD in patients with ToF.73–75
Noncompaction of the left ventricle is a rare congenital cardiomyopathy characterized anatomically by excessive prominent trabeculae and deep intertrabecular recesses in the left ventricle without other major congenital cardiac malfunction. Ventricular arrhythmias and SCD are known to occur, and ICD therapy often is indicated.76–78
Commotio Cordis
The term commotio cordis refers to a blunt, nonpenetrating, and usually innocent-appearing chest blow that can cause VF. The location of the blow to the chest (directly over the heart) and its timing relative to the cardiac cycle (on the upstroke of the T wave, 10 to 20 msec before its peak) are the primary determinants of commotio cordis.79,80
Other Genetic Associations in Patients with Structurally Normal Hearts
SCD likely has a strong genetic component, but only a fraction of the genetic variants that underlie the risk are known; the allelic architecture of SCD thus remains poorly defined.81 Genome-wide association studies have indicated that common variants in NOS1AP are associated with Q-T interval duration and SCD risk in general populations.82 The common polymorphism S1103Y-SCN5A is disproportionately represented in patients with arrhythmia and black patients who have experienced SCD.83 These variants by themselves are unlikely to be sufficient causes of SCD.
Risk Stratification for Sudden Cardiac Death
In SAECG, the terminal part of the QRS complex is evaluated for microvolt potentials that reflect delayed activation in the scarred myocardial substrate, thereby detecting areas of slow conduction.84 In patients with prior MI, the negative predictive value of this test has been demonstrated to be excellent. However, the usefulness of this test has been limited by its low positive predictive value, and its routine use is not common.85–87 However, the presence of an abnormal SAECG continues to have a clinical role in ARVC as a minor criterion for its diagnosis.
Q-T interval dispersion examines the difference between the maximal and minimal Q-T intervals from various standard ECG leads, whereas TWA is defined as microvolt changes in the T-wave amplitude from beat to beat.88,89 Studies evaluating the Q-T interval for prediction of SCD risk in individuals who do not have LQTS have demonstrated mixed results but have generally linked prolonged Q-T interval with increased risk. In recent studies, Q-T interval dispersion has not been shown to be a consistent predictor of SCD.87,90
TWA describes alterations in the amplitude of the T wave at modestly increased heart rates (105 to 110 beats/min) elicited by either exercise or atrial pacing. A number of observational cohort studies have suggested that microvolt TWA may work at least as well as electrophysiological testing to predict SCD or major arrhythmic events in ischemic and nonischemic cardiomyopathy.91–94 The Microvolt T-Wave Alternans Testing for Risk Stratification of Post-Myocardial Infarction Patients (MASTER) study, a prospective study of patients with prior MI and LVEF less than 30%, found that the TWA test results did not influence the frequency of the composite endpoint of arrhythmic death or “appropriate” shock over a 3-year follow-up.93 The recent Alternans Before Cardioverter Defibrillator (ABCD) trial compared the usefulness of EPS versus TWA testing in patients with ischemic cardiomyopathy and LVEF less than 40%.96,97 The results led the authors to conclude that EPS and TWA testing were comparable in terms of predicting risk and were complementary to each other. In contrast, a prospective substudy of the Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT) showed that TWA was not predictive of arrhythmia or death and therefore was not a useful marker in identifying patients who would benefit from an ICD.98,99 These contrasting results have limited the generalized applicability of TWA in the risk stratification for SCD.
Evidence from both clinical and experimental studies supports a role for the autonomic nervous system in the genesis of VT or VF. An association exists between increased sympathetic activity, reduced vagal activity, or both, with a propensity for VF during myocardial ischemia.99 The two major measures of autonomic function that have been tested in clinical studies include heart rate variability (HRV) and baroreflex sensitivity (BRS).40 HRV reflects both the sympathetic and parasympathetic effects on the heart and is measured as the standard deviation of R-R intervals in the heart rate over a 24-hour period. BRS, in contrast, is an indicator of the reflex capacity of the autonomic nervous system and usually is measured by the phenylephrine method.100 Studies suggest that BRS has potential for SCD risk stratification in patients with CAD and that HRV is a predictor of total mortality but may, in fact, be a better marker of nonarrhythmic death.101,102 Further studies are needed to establish the clinical usefulness of these parameters for risk stratification and at this time are of limited utility.
LVEF is a well-established and consistent reported risk factor for overall mortality and SCD. It has been used in the risk stratification schema on many primary prevention clinical trials of SCD. In addition, the more recent Multicenter Autonomic Defibrillator Implantation Trial II (MADIT II) used only LVEF (<30%) for risk stratification for inclusion into the protocol. The results of MADIT II indicate that the use of LVEF alone for risk stratification is associated with significant mortality benefit from prophylactic ICD therapy.103 Impaired EF in certain patient populations, such as in those with early previous MI, have been shown to not be predictive of SCD from trial data.104 Of note, although low LVEF identifies a group with relatively increased risk, most instances of SCD occur in patients with a more preserved LVEF, which highlights the limited sensitivity of this technique.105,106 Heart failure itself also can contribute to arrhythmogenesis in patients with ventricular dysfunction and can increase the mortality rate in patients with dilated cardiomyopathy independent of EF. Qualitative descriptions of functional capacity such as NYHA class, although limited by subjectivity, have been well studied. NYHA classes II and III continue to be accepted as criteria to identify at-risk individuals with impaired left ventricular function for whom ICD is indicated.107–109 The presence of ventricular arrhythmias (premature ventricular contractions [PVCs] and nonsustained ventricular tachycardia [NSVT]) has also been examined in various studies to assess their role in predicting SCD. In one major trial, the positive predictive value of ventricular ectopy after MI for predicting cardiac arrhythmic events or death was limited to 5% to 15%.103 Frequent ectopy or NSVT is insensitive, failing to identify 47% to 94% of those who experience sudden cardiac arrhythmia.110 However, if combined with low LVEF, ventricular ectopy becomes a stronger risk factor for death.
Patients with nonischemic cardiomyopathy frequently have high-grade ventricular ectopy and NSVT. However, the relationship with cardiac arrest is much less clear than is the case of ischemic cardiomyopathy. In general, the incremental use of ambient ventricular arrhythmias is limited and may actually reflect the degree of heart failure rather than providing a specific marker of SCD. NSVT, in particular, has been identified as a risk factor for SCD in patients with HCM. In summary, the role of ambient nonsustained ventricular arrhythmias in predicting SCD appears to be limited. In patients with a history of previous MI, the induction of VT during an EPS has been shown to predict a high risk for recurrent arrhythmias and SCD.111,112 EPS has also been established in a number of other clinical situations, such as in patients with a history of cardiac arrest.113–115 The predictive value of EPS is highest in patients with a history of MI as opposed to those with nonischemic cardiomyopathy.1 Although a positive test result predicts increased risk for SCD, a negative result does not exclude risk, particularly in patients with severe left ventricular dysfunction. In MADIT II, ICD use was associated with a significant survival benefit even in the absence of EPS.103 In the previously reported MADIT I, inducibility in study patients was associated with an increased likelihood of VT; however, the noninducible study subjects had a considerable VT or VF event rate.116 EPS in patients with normal LVEF is of limited clinical benefit. In patients with conditions such as hypertrophic cardiomyopathy, the role of EPS is uncertain, and negative EPS findings do not exclude high risk for SCD. VF is commonly induced in these patient populations and is of uncertain clinical significance.117,118 EPS can discriminate between patients with high risk versus low risk for SCD, but if used in isolation, the sensitivity is inadequate, especially in patients with EF less than 30%. EPS is of more value when used in patients with equivocal results after noninvasive testing than as an initial screening test.119
SCD in competitive athletics generates considerable attention and concern. Although the American Heart Association consensus panel does not endorse mandatory ECG screening for all competitive athletes, it does not discourage screening initiatives by individual organizations.120 In contrast, the European Society of Cardiology recommends that evaluation include electrocardiography, chest radiography, and echocardiography.121
Another risk stratification technique that continues to evolve is that of contrast-enhanced MRI, which, if supported by clinical data, could possibly provide information on susceptibility to VAs and therefore SCD. When assessing risk with algorithms, one should be aware that no single risk factor possesses adequate sensitivity but that the presence of multiple risk factors will inappropriately reduce the number of patients who qualify for ICD therapy. Overcoming such limitations requires balancing the sensitivity and specificity of various risk stratification approaches.103
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree