A 72-year-old diabetic, hypertensive man presents with waxing and waning episodes of sharp chest pain that started 9 hours earlier. The current episode of pain has been ongoing for the past 3 hours. On physical examination, the pain appears to be reproducible with palpation, and the patient does not demonstrate any distress or diaphoresis. The first troponin I level is 0.03 ng/ml.
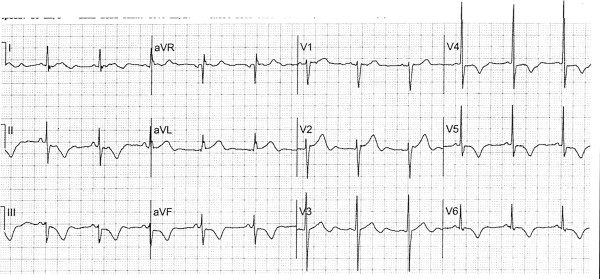
The presenting electrocardiogram ( Figure 1 ) shows sinus rhythm; one aberrantly conducted premature atrial complex; left anterior fascicular block; left ventricular hypertrophy by Cornell criteria; and subtle ST-T signs of inferior, lateral, and posterior injury. The ST-segment depression in leads V 1 through V 3 implies posterior ST-segment elevation of infarction. Although the ST segment is only slightly elevated in the inferior leads and in leads V 5 and V 6 (∼0.05 mV), it has a convex morphology with a wide, hyperacute T wave, particularly evident on the aberrant complex. This morphology suggests an injury pattern, even if the ST-segment elevation is subtle. Moreover, reciprocal ST-segment depression and T-wave inversion are seen in lead aVL, further confirming that the inferior ST-T changes represent an injury pattern.
Once it has been determined that ST-elevation injury is present, the next step is to identify the culprit artery. A left circumflex coronary arterial occlusion is associated with ST-segment depression in leads V 1 , V 2 , aVR, and ST-segment elevation in lead I (or, at the very least, a lack of ST-segment depression in lead I). Therefore, the left circumflex is the likely culprit artery in this case, rather than the right coronary artery. Subtle, overlooked ST-segment abnormalities are common with acute left circumflex occlusions.
Emergent primary percutaneous coronary intervention (PCI) is warranted in a patient continuing to have chest pain within 12 hours of onset. Even if the pain subsides with antithrombotic or nitrate therapy, emergent PCI is still warranted as long as the electrocardiographic abnormality persists. Although thrombolysis is a viable alternative in patients with ST-segment elevation myocardial infarction presenting to non–PCI-capable facilities, thrombolysis is not clearly indicated in this patient with subtle, <0.1-mV ST elevation (a case in which immediate coronary angiography is still recommended).
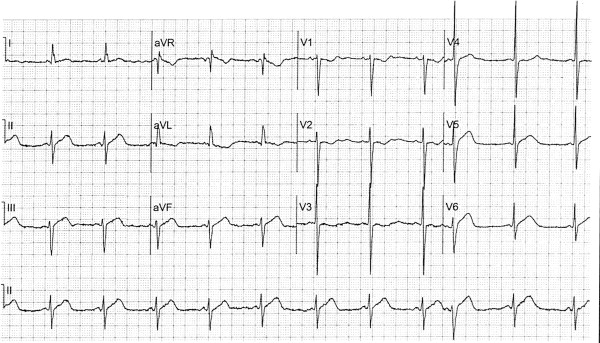
Unfortunately, the team initially involved with the patient’s care does not call for emergent reperfusion, and troponin I eventually peaks at 76 ng/ml. The patient’s pain subsides 1 hour after presentation. An electrocardiogram obtained 10 hours later shows evolution of the wide upright T waves into inverted T waves in the inferior leads and in leads V 5 to V 6 ( Figure 2 ). The upright T waves that are now seen in leads V 1 to V 3 are mirror images of inverted posterior T waves. Coronary angiography is performed the next day and shows a subtotal occlusion of a large second obtuse marginal branch with Thrombolysis in Myocardial Infarction (TIMI) flow of 2. The occlusion is successfully stented.