Transcatheter aortic valve implantation (TAVI) is associated with a significant learning curve. There is paucity of data regarding the effect of hospital volume on outcomes after TAVI. This is a cross-sectional study based on Healthcare Cost and Utilization Project’s Nationwide Inpatient Sample database of 2012. Subjects were identified by International Classification of Diseases, Ninth Revision, Clinical Modification procedure codes, 35.05 (Trans-femoral/Trans-aortic Replacement of Aortic Valve) and 35.06 (Trans-apical Replacement of Aortic Valve). Annual hospital TAVI volumes were calculated using unique identification numbers and then divided into quartiles. Multivariate logistic regression models were created. The primary outcome was inhospital mortality; secondary outcome was a composite of inhospital mortality and periprocedural complications. Length of stay (LOS) and cost of hospitalization were assessed. The study included 1,481 TAVIs (weighted n = 7,405). Overall inhospital mortality rate was 5.1%, postprocedural complication rate was 43.4%, median LOS was 6 days, and median cost of hospitalization was $51,975. Inhospital mortality rates decreased with increasing hospital TAVI volume with a rate of 6.4% for lowest volume hospitals (first quartile), 5.9% (second quartile), 5.2% (third quartile), and 2.8% for the highest volume TAVI hospitals (fourth quartile). Complication rates were significantly higher in hospitals with the lowest volume quartile (48.5%) compared to hospitals in the second (44.2%), third (39.7%), and fourth (41.5%) quartiles (p <0.001). Increasing hospital volume was independently predictive of shorter LOS and lower hospitalization costs. In conclusion, higher annual hospital volumes are significantly predictive of reduced postprocedural mortality, complications, shorter LOS, and lower hospitalization costs after TAVI.
The treatment options for high- and extreme-risk patients with severe symptomatic aortic stenosis have changed significantly over the past decade because of advances in transcatheter aortic valve implantation (TAVI). TAVI presently provides a valuable therapeutic option for select patients. The Food and Drug Administration (FDA) approval of the first TAVI device in November 2011 and subsequent Centers for Medicare and Medicaid (CMS) coverage in May 2012 have resulted in widespread dissemination of the procedure with more than 250 clinical sites in the United States currently performing TAVI. The initial results from clinical registries have shown promising “real-world” outcomes comparable to trial data. However, TAVI is a complex procedure with constantly evolving technology and a steep learning curve that necessitated a supervised initial rollout. Although hospital and operator experience requirements exist, there are limited data on the relation between postprocedural outcomes and hospital procedural volumes. The primary objectives of our study were (1) to evaluate the postprocedural outcomes after TAVI from one of the largest publicly available nationwide databases and (2) to further apprise predictors of TAVI outcomes with specific focus on the effect of hospital volume.
Methods
The study cohort was derived from the National Inpatient Sample (NIS) database of 2012, a subset of the Healthcare Cost and Utilization Project (HCUP) sponsored by the Agency for Healthcare Research and Quality (AHRQ). The NIS is the largest publicly available all-payer inpatient care database in the United States, including data on approximately 7 to 8 million discharges per year, and is a stratified 20% sample of discharges from US community hospitals, excluding rehabilitation and long-term acute-care hospitals. National estimates are produced using sampling weights provided by the sponsor. The details regarding the NIS data have been previously published.
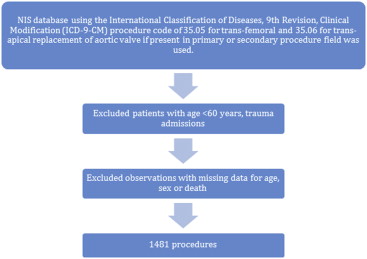
The International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) Volume 3 procedure code subcategory 35.0 was expanded effective October 1, 2011, and new codes were added to report TAVI. We queried the NIS database using the ICD-9-CM procedure code of 35.05 for transfemoral/transaortic and 35.06 for transapical replacement of aortic valve if present in the primary or secondary procedure field. We identified 1,481 procedures after excluding patients aged <60 years, trauma admissions, and observations with missing data for age, gender, or death ( Figure 1 ).