There is a paucity of evidence on the impact of angiotensin-converting enzyme inhibitors (ACEi) and angiotensin receptor blockers (ARB) on long-term outcomes in patients with ejection fraction (EF) >40% after primary percutaneous coronary intervention for ST-segment elevation myocardial infarction (STEMI). We compared long-term all-cause mortality between patients with left ventricular ejection fraction (LVEF) >40% discharged on ACEi/ARB with patients who were discharged on neither of these agents. Patients discharged after percutaneous intervention for STEMI from our catheterization laboratories from January 2002 to December 2011 were considered for inclusion. Patients were excluded if they had LVEF <40% or chronic kidney disease or hypotension (systolic blood pressure <90 mm Hg any time after the procedure). Long-term mortality and discharge medications were determined using the Social Security Death Index and electronic medical record review, respectively. A total of 988 patients were included. The median follow-up duration was 4.6 years. Kaplan-Meier analysis showed no significant difference in long-term all-cause mortality in patients discharged on ACEi/ARB compared with those who were not discharged on these medications. The number needed to treat to prevent 1 death at 1 year was 714. In addition, multivariable Cox proportional hazard modeling failed to demonstrate any beneficial effect of ACEi/ARB similar to Kaplan-Meir analysis (hazard ratio 0.88, 95% confidence interval 0.57 to 1.36). In conclusion, we found no significant benefit in long-term mortality using ACEi/ARB in patients with LVEF >40% after primary percutaneous coronary intervention for STEMI.
The paucity of evidence on the impact of long-term angiotensin-converting enzyme inhibitors/angiotensin receptor blockers (ACEi/ARB) therapy on long-term mortality in patients without LV dysfunction after ST-elevation myocardial infarction (STEMI) is reflected in both the AHA/ACC and European guidelines. These groups provide a class IA recommendation for use of these agents only in patients with reduced left ventricular ejection fraction (LVEF <40%) or overt heart failure. However, their long-term use is not considered essential in patients who have neither LV systolic dysfunction nor symptomatic heart failure. The guidelines provide for a class IIA level of recommendation in the latter subset of patients because of conflicting evidence from major clinical trials. As a result, RAS inhibition therapy in patients with STEMI without reduced LVEF is largely based on the treating physician’s personal preference. We, therefore, sought to compare survival between patients in this group discharged from the hospital after primary percutaneous coronary intervention (pPCI) for STEMI who were given ACEi/ARB versus those who were not.
Methods
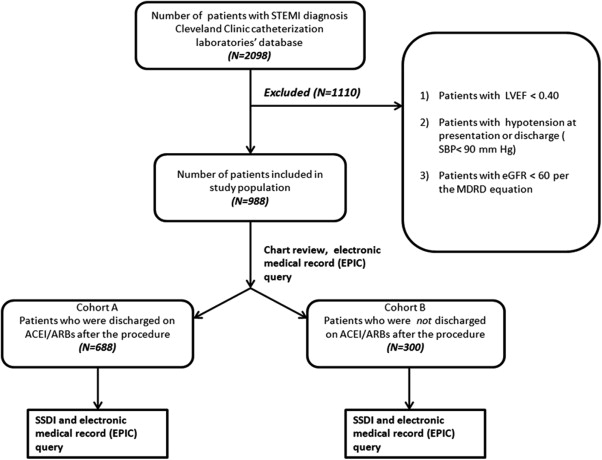
All adult patients who were discharged after they underwent pPCI for STEMI from January 2002 to December 2011 and without significant LV dysfunction (LVEF ≥40%) at the time of discharge were considered for inclusion. Patients were excluded if they had chronic kidney disease (estimated glomerular filtration rate <60 ml/min/1.73 m 2 ) using Modification of Diet in Renal Disease formula or hypotension (systolic blood pressure [BP] <90 any time after the procedure). The flow diagram for the study protocol is shown in Figure 1 . Patients were classified into 2 cohorts after a manual review of the discharge summary of the index hospitalization, namely (1) patients who were discharged on ACEi/ARB and (2) patients who were not discharged on ACEi/ARB. Patient information was reviewed at 6 months and 1, 5, and up to 10 years to ascertain the continuation of drug therapy, and data were appropriately censored based on the information obtained. The study was approved by the Cleveland Clinic Institutional Review Board. We queried the data in the electronic medical records, diagnostic catheterization database, and the PCI database for baseline characteristics, cardiac history, risk factors, and angiographic characteristics. The primary outcome was long-term all-cause mortality, which was determined using the Social Security Death Index and an extensive review of the electronic medical records. Continuous variables are presented as mean ± SD, and categorical variables are presented as proportions. The comparisons between the 2 study groups were performed using the Student’s t test for continuous variables with normal distribution and the Wilcoxon rank-sum test for continuous variables with skewed distributions (assessed by Shapiro-Wilk test). The chi-square test was used for comparing categorical variables. Discrete logistic regression modeling was done to determine odds ratios (adjusted and unadjusted) for mortality at 6 months and 1, 5, and 10 years.
We also used standard survival analysis strategies to determine differences between long-term all-cause mortality between the 2 cohorts. Unadjusted survival analysis was conducted using the Kaplan-Meier method, and statistical comparisons were drawn using the log-rank test. Adjusted survival analysis was carried out using multivariable Cox proportional hazard modeling. In this analytical approach, we adjusted for patient-level data, such as demographics and coronary risk factors including age, gender, body mass index (BMI), diabetes, hypertension, smoking status, and dyslipidemia, using stepwise regression approach with backward selection ( Supplementary Table 1 ). We also performed stratified analysis to determine hazard ratios for long-term mortality among different subgroups within our study population. Number needed to treat (NNT) was calculated at different time points using the survival probabilities obtained from the time-event analysis. If at some specified time, t, the survival probability in the control arm was S c (t), then the survival probability in the treatment arm was [S c (t)] h , where h is the hazard ratio comparing the treatment groups. The NNT may be estimated as: NNT = 1/[S c (t)] h − S c (t)]. All statistical tests were 2 tailed and confidence intervals (CIs) reported at 95% level (p value <0.05 was considered significant). The analyses were performed using the statistical software—Stata, version 12.1 (StataCorp, College Station, Texas).
Results
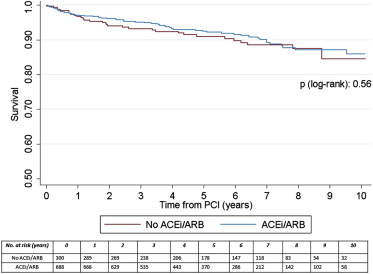
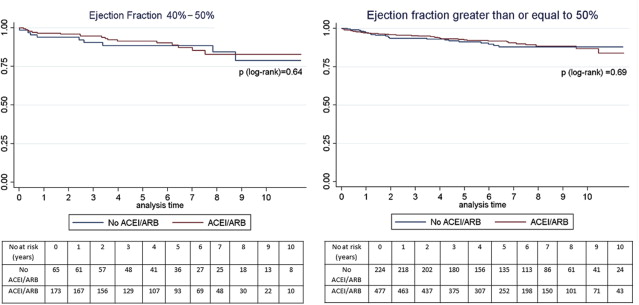
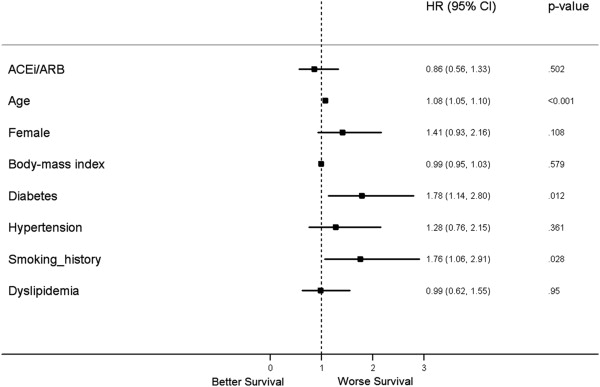
A total of 988 patients were included in this study, with a median follow-up of 4.6 years. Of these, 300 patients were not discharged on either ACEi or ARB. The remaining 688 patients were discharged on either ACEi or ARB. The median length of stay after PCI in our study population was 3 days (interquartile range 2 to 4 days). Table 1 demonstrates the baseline characteristics of the study population stratified by study group and the comparison of short-term and long-term mortality between the 2 groups. There was no significant difference in mortality at 6 months and 1, 5, and 10 years between the study cohorts. Figure 2 shows unadjusted Kaplan-Meir curves comparing all-cause mortality between the 2 cohorts. In Figure 3 , we present a stratified Kaplan-Meier analysis based on the LVEF values between 40% and 50% and >50%. As evident, we found no significant difference in mortality over the follow-up period in both overall and stratified study populations. Figure 4 demonstrates results from the adjusted survival analysis using the Cox proportional hazard method. Age (hazard ratio [HR] 1.08, 95% CI 1.05 to 1.10), smoking (former or present; HR 1.76, 95% CI 1.06 to 2.91), and diabetes (HR 1.78, 95% CI 1.14 to 2.80) were associated with worse long-term survival. However, similar to unadjusted analysis, we found no significant mortality benefit of ACEi/ARB (adjusted HR 0.86, 95% CI 0.56 to 1.33). Similarly, gender, BMI, hypertension, and dyslipidemia were not significantly associated with increased mortality in this statistical model. The NNT to prevent 1 mortality was estimated to be 714 at 1 year and 189 at 5 years, using the methodology described earlier. Separately, we did not observe any difference in mortality for ACEi (adjusted hazard ratio 0.78, 95% CI 0.53 to 1.23) or ARB (adjusted hazard ratio 1.14, 95% CI 0.63 to 2.05).
| Characteristic | All Patients | Patients not discharged on ACEI/ARB | Patients discharged on ACEI/ARB | p-value |
|---|---|---|---|---|
| N | N=988 | N=300 | N=688 | |
| Mean (SD) age, years | 57.9 ±12.3 | 58.4 ±11.6 | 57.8 ±12.6 | 0.50 |
| Women | 292 (29.6%) | 102 (34.1%) | 190 (27.6%) | 0.05 |
| Hypertension | 660 (66.8%) | 189 (63.1%) | 471 (68.5%) | 0.10 |
| Diabetes mellitus | 200 (20.2%) | 63 (21.1%) | 137 (19.9%) | 0.70 |
| Hyperlipidemia | 633 (64.1%) | 193 (64.3%) | 440 (63.9%) | 0.80 |
| Peripheral Vascular disease | 52 (5.3%) | 21 (7.1%) | 31 (4.5%) | 0.10 |
| Chronic obstructive pulmonary Disease | 100 (10.1%) | 39 (13.0%) | 61 (8.8%) | 0.05 |
| Mean (SD) ejection fraction (%) | 52.2± 5.7 | 52.7±5.8 | 52.1 ±5.7 | 0.10 |
| Mean (SD) body-mass index, (kg/m 2 ) | 29.9 ±6.3 | 29.1 ±6.8 | 30.2 ±6.1 | 0.10 |
| Mean (SD) creatinine, (mg/dL) | 0.86 ±0.19 | 0.83 ±0.19 | 0.87± 0.19 | 0.01 |
| Cerebrovascular disease (%) | 30± 3.0 | 7 ±2.3 | 23 ±3.3 | 0.40 |
| Smokers | 751 (76.1%) | 225 (75%) | 526 (76.4%) | 0.70 |
| Race (%) | 0.07 | |||
| White | 663 (67.1%) | 221 (73.7%) | 442 (64.2%) | |
| Black | 282 (28.5%) | 65 (21.7%) | 217 (31.5%) | |
| Others | 42 (4.3%) | 13 (4.3%) | 29 (4.2%) | |
| Mortality after PCI derived from time-event analysis | ||||
| Time after PCI | ||||
| 6 months | 18 (1.8%) | 5 (1.6%) | 13 (1.9%) | 0.81 |
| 1 year | 30 (3.0%) | 10 (3.3%) | 20 (2.9%) | 0.72 |
| 5 years | 71 (7.2%) | 25 (8.3%) | 46 (6.7%) | 0.35 |
| 10 years | 92 (9.3%) | 32 (10.6%) | 60 (8.7%) | 0.32 |
Note: Hypertension was defined as presence of any one of the following features:
- 1.
Systolic BP >140 mm Hg and/or diastolic BP >90 mm Hg on presentation.
- 2.
Documented hypertension by patient’s primary care provider (PCP) in patient’s problem list in electronic medical record. Patients were either diet/lifestyle controlled or pharmacologically controlled depending on PCP’s decision.
- 1.
Diabetes mellitus was defined as presence of any one of the following features:
- 1.
Any value of hemoglobin A1C >6.5 in patient’s electronic record prior to index PCI.
- 2.
Documented diabetes mellitus by patient’s primary care provider (PCP) in patient’s problem list in electronic medical record. Patients were either diet/lifestyle controlled or pharmacologically controlled depending on PCP’s decision.
- 3.
Patients on home insulin or oral anti-diabetes medications per our electronic medical records.
- 1.
Dyslipidemia for the purpose of this study was defined as presence of any one of the following factors:
- 1.
Total cholesterol >200 or LDL>160 or HDL <40 at the time of index PCI.
- 2.
Documented hyperlipidemia/dyslipidemia by patient’s primary care provider (PCP) in patient’s problem list in electronic medical record. Patients were either diet/lifestyle controlled or pharmacologically controlled depending on PCP’s decision. Notably, all patients who were on any cholesterol lowering drugs were NOT automatically labeled as dyslipidemia due to routine practice of placing patients on statins for secondary prevention of CAD.
- 1.
We also performed stratified analysis to determine hazard ratios for long-term mortality among different subgroups within our study population. As shown in the Supplementary Figure 1 , we stratified the study population based on gender, BMI, smoking status, site of MI, diabetes status, and dyslipidemia. We found no significant reduction in mortality in any subgroup. There was no statistically significant benefit in patients with dyslipidemia (HR 0.70, 95% CI 0.43 to 1.15), anterior wall MI (HR 0.81, 95% CI 0.42 to 1.56), and smokers (HR 0.82, 95% CI 0.51 to 1.31). We also performed propensity matching through calculated propensity scores. Notably, we analyzed matched data again and found no difference in mortality in patients treated with ACEi/ARB versus those not treated (HR 0.84, 95% CI 0.53 to 1.37; Supplementary Table 2 and Supplementary Figure 2 ).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


