Fig. 26.2 Atrial fibrillation (AF). Marked irregularity to the baseline, with no discernable P waves, and an irregular QRS response indicate that the rhythm is atrial fibrillation. Heart rate, 75 b/min. Unremarkable QRS complexes. Conclusion is AF with no other ECG evidence of heart disease.
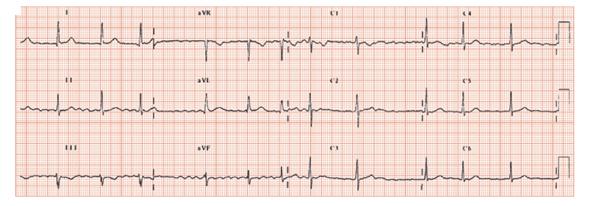
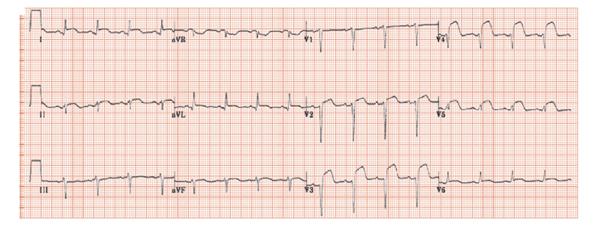
Fig. 26.3 Myocardial infarction (MI). Sinus rhythm, unremarkable P waves, normal PR interval. QRS complex show left axis deviation (−38° positive in lead I, negative in lead II and III). Very deep S wave in leads V1–4, with just a tiny preceding R wave – in practical terms, these are the same as pathological Q waves. ST elevation in lead I, II ( just), aVL, V2–5, indicating an evolving antero-lateral MI. Conclusion: recent (≤ 1 or 2 days) anterior wall MI. Some 1% of untreated MIs are complicated by a stroke, a risk reduced by streptokinase.
Stroke is a common disabling condition. The ECG can help determine aetiology; sometimes it changes as the consequence of stroke.
Aetiological clues to stroke from the ECG
- Left ventricular hypertrophy (LVH) (Fig. 26.1) is an important risk factor for stroke, partly as it is very strongly associated with prolonged hypertension (itself associated with stroke), and partly for other little understood reasons (meta-analyses suggest that LVH is an risk factor for stroke, independent of other confounders such as hypertension).
- Atrial fibrillation (Fig. 26.2) is a powerful risk factor for stroke, particularly in the elderly, those with hypertension, and those with structural heart disease. It usually needs to be present for ≥ 24 h to cause stroke. It is often present at the time of hospitalization for the acute stroke though some data suggests that it may be intermittent, and should be screened for in all those who present with stroke with an initial ECG showing sinus rhythm.
- Myocardial infarction (MI), especially transmural infarction in the early stages, is a potent risk factor for stroke (Fig. 26.3). Usually the MI is obvious, and causes typical symptoms, and either ST elevation or Q waves are seen on the ECG. Sometimes it is silent, and the ECG changes may be subtle; loss of R wave height, or ST/T wave changes only.
- Left ventricular (LV) dysfunction, especially if associated with heart failure, is another important risk factor for stroke. The ECG clues to LV dysfunction are:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


