Chapter 29 Stress Myocardial Perfusion Imaging in Patients with Diabetes Mellitus
INTRODUCTION
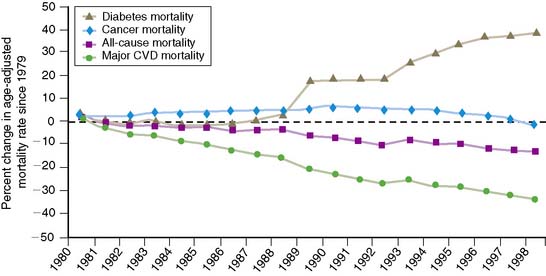
In 2005, the Centers for Disease Control and Prevention (CDC) estimated that there were approximately 21 million people with diabetes mellitus in the United States: 15 million with diagnosed diabetes mellitus and 6 million with undiagnosed diabetes. Greater than 95% of these individuals have type 2 diabetes.1 The number of patients with diabetes mellitus increases every year by 5%, adding approximately 1.5 million new cases annually. Compared to the nondiabetic population, patients with diabetes mellitus have an increased risk of developing cardiovascular disease and an increased risk for death from myocardial infarction or congestive heart failure. Although in the general population, the overall age-adjusted mortality from cardiovascular diseases decreased by 30% between 1990 and 2000, the mortality rate in patients with diabetes mellitus has increased by approximately the same amount (Fig. 29-1). Importantly, 80% of the mortality among diabetics can be attributed to cardiovascular causes. Because of these alarming statistics, the American Diabetes Association; the National Heart, Lung and Blood Institute; the Juvenile Diabetes Foundation International; the National Institute of Diabetes and Digestive and Kidney Diseases; and the American Heart Association issued a joint statement in 1999 indicating the importance of diabetes mellitus as a major risk factor for cardiovascular disease.2
EARLY DETECTION OF CORONARY ARTERY DISEASE IN DIABETES MELLITUS
To maximize the effect of appropriate treatment of cardiovascular disease, it is important that diabetic patients at risk of developing or who have already developed coronary artery disease (CAD) are identified as early as possible. A major hurdle toward this goal is that CAD in patients with diabetes is frequently silent; when clinically manifest, it is often in an advanced stage. Twenty-five percent of patients with diabetes mellitus in the Framingham Study had electrocardiographic evidence of prior unrecognized infarction, and half of these individuals were asymptomatic.3–5 Less than a third of diabetic patients with exercise-induced ischemia on myocardial perfusion imaging (MPI) had angina during exertion, compared to more than two-thirds of nondiabetic patients. In 1998, the American Diabetes Association published a consensus statement on diagnostic testing for CAD in people with diabetes mellitus.6 It was recommended that asymptomatic diabetic patients with two or more risk factors for CAD in addition to diabetes mellitus should have exercise stress testing. The consensus statement further recommended exercise electrocardiography (ECG) as the first diagnostic test. These recommendations were based on the clinical judgment of a panel of experts rather than on published scientific data in truly asymptomatic patients. At the time of the consensus statement, it was evident that a substantial gap existed in the knowledge about the prevalence of silent ischemia, how to detect preclinical CAD, and how to manage asymptomatic patients with diabetes in whom silent ischemia was demonstrated. In subsequent years, a number of studies have demonstrated unequivocally that the presence or absence of traditional risk factors for CAD in patients with diabetes are not helpful for predicting silent myocardial ischemia. Therefore, other clinical and diagnostic algorithms need to be explored for identifying diabetic patients at increased cardiovascular risk.
Stress Modality
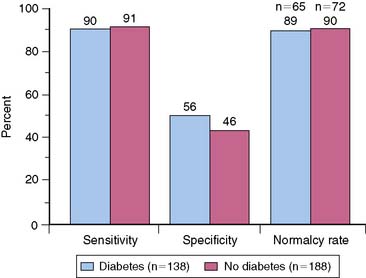
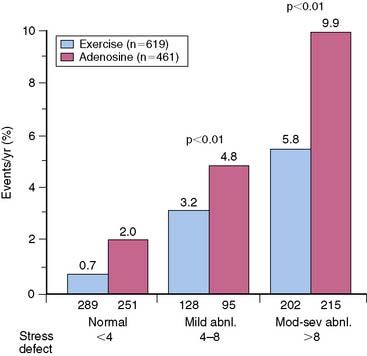
In the general population, the preferred stress modality for detecting myocardial ischemia is physical exercise on a treadmill or bicycle. However, many diabetic patients have diminished exercise ability because of obesity, deconditioning, peripheral neuropathy, or peripheral vascular disease. Several studies have observed that about a third to half of diabetic patients were unable to achieve adequate exercise levels for diagnostic testing.7 Therefore, pharmacologic stress may be the more appropriate stress modality in many patients with diabetes. Stress MPI has been shown to have comparable sensitivity and specificity in nondiabetics and diabetic patients for detecting CAD (Fig. 29-2).8 Moreover, the incremental prognostic value of pharmacologic MPI was similar to that using physical exercise (Fig. 29-3).9,10
Prevalence of Silent Myocardial Ischemia
Screening for CAD is a controversial issue in clinical cardiology. To avoid an unacceptably large number of false-positive test results, the prevalence of the disease for which screening is to be performed must be at least intermediate. The true prevalence of silent myocardial ischemia in asymptomatic patients with diabetes was until recently unknown because most estimates were based on retrospective database analyses. The results of the prospective Detection of Ischemia in Asymptomatic Diabetics (DIAD) study made very clear that indeed most previous studies were significantly biased owing to patient selection. Retrospective database analyses may not be accurate because patients were most likely referred for stress testing to investigate symptoms suspected to be due to CAD. The available published information consisted of three types of analyses: retrospective analysis of large, combined nuclear cardiology databases, retrospective analysis of single laboratory databases, and prospective epidemiologic studies. In two large retrospective database studies, the prevalence of abnormal myocardial perfusion images ranged from 41% to 58%.8,11,12 Detailed information on patients’ symptoms was not available, and it was unclear how many patients were truly asymptomatic. In other retrospective analyses of apparently asymptomatic patients with diabetes, 26% to 59% had abnormal stress myocardial perfusion images.13–16 These patients were referred for risk assessment before general surgery or because of the presence of multiple risk factors for CAD. Several prospective studies have been performed in Europe in asymptomatic patients with diabetes. The observed prevalence of ischemia in these studies varied as well. Whereas Janand-Delenne and colleagues17 reported a prevalence of silent myocardial ischemia of 18.4%, Gazzaruso and colleagues18 and the Italian MiSAD group19 reported a prevalence of 8.6% and 6.4%, respectively. In the latter studies, characteristically, exercise electrocardiography was the first stress test, and MPI was only performed if exercise electrocardiography was positive or equivocal. Because of the known low sensitivity of exercise electrocardiography, a substantial number of patients may have been missed in these studies.
The prospective multicenter DIAD study20 published in 2004 shed a different light on the practical problem of silent myocardial ischemia in asymptomatic patients with diabetes. It is important to consider the entry criteria for the DIAD study. All patients enrolled in the study had type 2 diabetes mellitus, were 50 to 75 years of age, had no symptoms suggesting CAD (including a negative Rose questionnaire for angina or chest discomfort), had a normal resting electrocardiogram, and had no prior cardiac stress testing. In addition to carefully ruling out symptoms of angina and anginal equivalents, the requirement of a normal rest ECG is an important characteristic of this study. Well over 1100 patients were recruited and randomized to either screening for CAD with adenosine technetium 99mTc sestamibi gated single-photon emission computed tomography (SPECT) imaging or no screening. The prevalence of silent myocardial ischemia, defined as regional myocardial perfusion abnormalities on imaging or ischemic ECG changes during adenosine infusion, was lower in the DIAD study than previously suggested in the literature. Although 22% of asymptomatic subjects had abnormal screening test results, in only 6% of participants were the myocardial perfusion abnormalities severe.20 Thus, 1 out of every 5 asymptomatic patients with diabetes may have silent CAD, and 1 of 16 may have markedly abnormal screening results. In a recent French study, similar to the DIAD study in design, age appeared to be an important factor for the occurrence of silent ischemia. Whereas asymptomatic patients with diabetes younger than 60 years had a prevalence of about 30%, patients older than 60 years had a prevalence of 43%.21
Endothelial Dysfunction
Many patients with diabetes mellitus have evidence for endothelial dysfunction.22,23 Persistent hyperglycemia may be in part responsible for impaired endothelial-dependent vasodilation. Oxidative stress and hyperproduction of superoxide are common in diabetes and might cause impaired endothelial nitric oxide synthesis. In addition, the insulin-resistant state itself may blunt nitric oxide–mediated vasodilation. Impaired regional coronary flow reserve has been observed in patients with diabetes mellitus, in particular in conjunction with cardiac autonomic dysfunction. The presence of microvascular endothelial dysfunction is of relevance for MPI. Regional myocardial perfusion abnormalities may occur in the absence of significant epicardial CAD.24 Whether such myocardial perfusion abnormalities have the same prognostic implications as those associated with epicardial CAD is as yet unclear. Emmett et al.25 reported that transient ischemic left ventricular dilation (TID) on SPECT imaging was strongly associated with diabetes mellitus and left ventricular hypertrophy, rather than with the amount of ischemia or severity of CAD. Thus, microvascular disease and endothelial dysfunction may play an important role in the etiology of TID.
ABNORMAL MYOCARDIAL PERFUSION IMAGING IN PATIENTS WITH SUSPECTED OR KNOWN CORONARY ARTERY DISEASE (See Chapter 16)
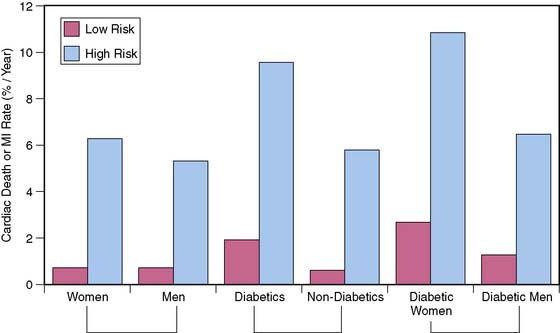
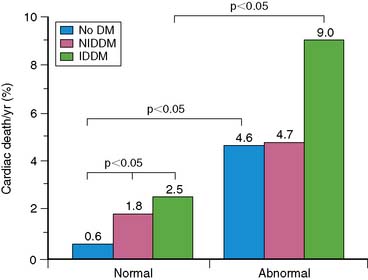
Observations in selected patient populations suggest that SPECT myocardial perfusion abnormalities in patients with diabetes mellitus carry a significantly worse prognosis than similar abnormalities in patients without diabetes mellitus. The most extensive retrospective five-center database analysis published thus far involved 4755 patients, of whom 929 had diabetes mellitus.11 More patients with diabetes were unable to exercise adequately and had vasodilator stress. Abnormal SPECT MPI was an independent predictor of cardiac death and nonfatal myocardial infarction in both nondiabetic patients and diabetic patients. However, in spite of higher revascularization rate, patients with diabetes had an almost two times higher cardiac event rate than nondiabetic patients. Unadjusted cardiac survival rate was lower for diabetic patients but became comparable to that in nondiabetic patients after adjustment for pretest clinical risk and severity of MPI abnormalities. An important observation was that diabetic women had a significantly worse outcome for any given extent of myocardial ischemia on SPECT imaging (Fig. 29-4).11,26 Another study that evaluated specifically the value of adenosine stress SPECT MPI in women confirmed the preceding observations.10 Although men and women without diabetes mellitus had similar outcomes for any given MPI abnormality, women with diabetes mellitus had significantly higher cardiac mortality. Furthermore, insulin-dependent patients were at higher risk than non-insulin-dependent diabetic patients (Fig. 29-5).10
Not unexpectedly, many asymptomatic patients with diabetes mellitus who are screened have entirely normal stress myocardial perfusion images. In the general population, patients with normal exercise myocardial perfusion images have an excellent prognosis with a low hard cardiac event rate of less than 1% per year.27 However, in patients with diabetes mellitus, this expectation appeared invalid. In a retrospective database analysis, Giri and colleagues11
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree