Robert A. Bruce, the father of exercise cardiology, once quipped, “You would never buy a used car without taking it out for a drive and seeing how the engine performed while it was running, and the same is true for evaluating the function of the heart.” This eloquent statement succinctly explains both the past motivation of early cardiologists to develop exercise protocols and the current need to modernize our evaluation of pediatric cardiovascular disease.
With the creation of, first, the Master’s Two-Step test and, second, the Bruce standardized treadmill test, cardiologists were provided for the first time with a standardized means to examine their patients outside of the resting condition. The ensuing introduction of the Bruce exercise protocol into the patient evaluation of congenital heart disease allowed cardiologists not only to predict the success of cardiac surgery but also to detect occult cardiovascular problems in otherwise asymptomatic individuals. The continued use of not only exercise but also other forms of stress in evaluating cardiac patients represents an extension of the resting physical examination. As Bruce stated in 1956, “an exercise test represents physical examination of the patient in relation to a reproducible amount of work.”
Despite the advances in and documented usefulness of stress testing, most cardiovascular assessment today unfortunately continues to be performed almost exclusively while the patient is comfortably resting (sometimes even sleeping) in a clinic or echocardiographic examination room. These appraisals, while yielding valuable information about resting conditions, afford little clue as to the behavior of the cardiovascular system when the patient becomes active, which is the typical state during most of the patient’s waking moments. Applying stress assessment in the clinical setting provides the means to observe the patient under conditions that closely mimic these more typically active states.
Further, in the relatively few cases when they are used, stress assessments have traditionally relied on electrocardiographic responses only. Interestingly, when he conceived of the exercise evaluation, Bruce focused attention on and found predictive ability with the hemodynamic responses, not the electrocardiographic changes, occurring with exercise. For instance, he not only discovered that the mechanism of exercise-induced hypotension is a consequence of fixed stroke volume but also that these hemodynamic changes were predictive of adverse long-term outcome. These conclusions acquired both during and after the exercise test were founded on physical examination alone. Since then, echocardiography has revolutionized cardiovascular diagnostics. The coupling of echocardiography with exercise or other forms of stress is a natural progression of exercise science because it provides the window for more direct, accurate, and robust observations of the important and predictive hemodynamic responses discovered by Bruce more than 50 years ago.
EVOLUTION OF STRESS ECHOCARDIOGRAPHY SCIENCE
Stress echocardiography is the culmination of the parallel evolutions of exercise science and cardiac ultrasound imaging driven, primarily, by coronary artery disease as a major public health problem. Exercise science had its beginnings in 1918 when the first objective measure of cardiac dysfunction during stress was made by Bousfield, who observed ST-segment depression occurring with angina. Systematic electrocardiographic exercise testing began 10 years later in patients with angina. In 1935, Master became the first to standardize the exercise test by developing an exercise protocol using a 9-inch two-step. However, this test was too strenuous for most patients and did not allow continuous data acquisition, prompting Bruce to develop first, the one-stage treadmill exercise test in 1949 and then, the multistage test (the Bruce protocol) in 1963.
The origins of stress imaging began in 1935, when Tennant and Wiggers noted by direct observation that interruption of coronary blood flow resulted in abnormal myocardial wall motion. However, it was not until 1970 that this phenomenon was visualized by ultrasound when Kraunz and Kennedy detected abnormal wall motion in patients with coronary artery disease immediately following exercise. The introduction of dobutamine stress echocardiography in 1986 improved image resolution because hyperpnea and patient motion associated with exercise were eliminated. In addition, dobutamine stress echocardiography provided a means to evaluate nonambulatory patients.
Pediatric stress echocardiography use began in 1980 when Alpert et al. performed simultaneous high-fidelity catheter pressure measurements and M-mode echocardiography during supine cycle ergometry in children with left-sided congenital heart disease to assess functional reserve. Exercise echocardiography was used throughout the 1980s in children for detection of subclinical left ventricular dysfunction in aortic insufficiency, insulin-dependent diabetes mellitus, and coarctation of the aorta. Pharmacologic stress echocardiography in children began in 1992, first using dipyridamole in patients after repair of anomalous left coronary artery from the pulmonary artery and, later, using dobutamine in children with a variety of cardiac pathology. However, even with these validated uses, stress echocardiography is underutilized in most pediatric echocardiography laboratories today.
THEORY BEHIND STRESS ECHOCARDIOGRAPHY
Stress echocardiography is a specific diagnostic modality categorized within a broader scheme of stress imaging protocols. However, all stress imaging protocols, including stress echocardiography, are unified by the concept that all use both a stressor (designed to stimulate patient hemodynamics) and a sensor (to evaluate the cardiovascular effects elicited by the specific stressor).
Stress echocardiography is applied for two basic diagnostic issues: (a) suspected impairment in myocardial perfusion or (b) hemodynamic behavior during stress of noncoronary cardiac pathology. In evaluating the first pathologic type (impaired myocardial perfusion) the theory underlying the utility of stress echocardiography simply relates to supply and demand. Myocardial oxygen demand is increased by applying the stressor. If the coronary arteries are normal, perfusion and myocardial oxygen supply also increase to meet the increased demands. However, if the coronary arteries are diseased, perfusion may not increase, creating a demand/supply mismatch, resulting in myocardial ischemia. The sensor is used to detect the resulting abnormality caused by this mismatch. For example, in the case of electrocardiography, demand/supply mismatch is manifest by ST-segment elevation. In the case of echocardiography, ischemia is manifest by a new or worsened myocardial wall motion abnormality. The manifestation of these abnormalities, and, therefore, the sensitivity of the sensors, is dependent on the degree of induced ischemic load (Fig. 34.1). Some sensors (e.g., positron emission tomography) are highly sensitive, and abnormalities (e.g., metabolic derangements) become evident with a brief and light ischemic load. Other sensors (e.g., ECG) are less sensitive, and the abnormalities sensed by them (e.g., ST-segment changes) become evident only with a long and heavy ischemic burden. The ischemia-induced wall motion abnormalities detected by echocardiography require an intermediate level of ischemic burden to become manifest and, therefore, echocardiography has an intermediate sensitivity.
In evaluating the second pathologic type (hemodynamic behavior of noncoronary heart disease) the theory underlying the utility of stress echocardiography is founded on the premise that stress data are more reflective of a patient’s typical diurnal activity state than are traditional data acquired in the resting state. In fact, data acquired during the resting state may be so dissimilar from data acquired during activity that the resting data may lead clinicians to a false sense of security regarding patient health. This premise has been similarly invoked for other cardiovascular tests that currently extend the patient evaluation beyond the office examination room such as ambulatory blood pressure and Holter monitoring. When using these two modalities, the clinician realizes that because symptomatology may not be present in the office milieu, additional data acquired during an active state are needed to capture symptoms and explore etiologies. Likewise, stress echocardiography, as a simulation of the patient’s active state, is used by clinicians to elicit and understand symptoms.
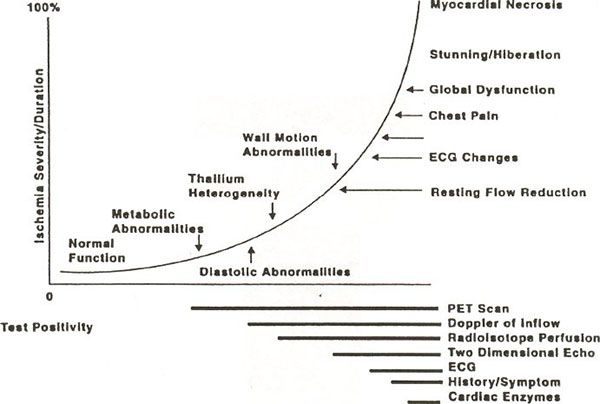
FIGURE 34.1. The ischemic cascade portrays the physiologic derangements (and the diagnostic sensors required to detect these derangements) occurring with a progressive ischemic burden. A low ischemic burden produces metabolic abnormalities that are detected by only highly sensitive sensors (e.g., positron emission tomography). A larger ischemic burden results in progressively deleterious derangements including diastolic dysfunction, wall motion abnormalities, myocardial stunning, and eventually myocardial necrosis. Angina develops with only a marked ischemic burden, making it a relatively insensitive indicator of coronary perfusion abnormalities. Wall motion abnormalities develop with an intermediate ischemic burden so that stress echocardiography has an intermediate sensitivity. (Reprinted with kind permission of Springer Science and Business Media.)
INDICATIONS
The indications for stress echocardiography must be discussed in the context of Bayes theorem which demonstrates that the clinical utility of a test, even with good sensitivity and specificity of the test, is related to the prevalence of disease in the population undergoing testing. For example, if a population has low prevalence of the disease, a positive test will have little predictive valve given the large number of false-positive results.
Bayes Theorem
Bayes theorem is a result in probability theory that demonstrates that the accuracy of a test with imperfect sensitivity and specificity is related to the prevalence of that disease in the population undergoing testing (Fig. 34.2). Specifically, the positive and negative predictive values of a test are dependent on the prevalence of the disease, so that low disease prevalence is associated with a high false-positive rate but a low false-negative rate. For example, in the evaluation of chest pain in an elderly, hypertensive adult patient, the positive predictive value of stress echocardiography would be appropriate and useful because the prevalence of coronary artery disease is high in elderly, hypertensive adults. The same would be true for a patient who has coronary artery strictures and thrombus due to Kawasaki disease. A positive test result would be highly likely to reflect advanced coronary artery disease. However, performing stress echocardiography in a healthy, thin adolescent complaining of chest pain would be of little help in detecting coronary artery disease because its prevalence is so low in healthy, thin adolescents. In this instance, Bayes theorem would predict that the test would have a high false-positive rate, so that a physician receiving a positive test result would still be left wondering if the patient truly has coronary artery pathology or, worse, establishing a false diagnosis of coronary artery disease. On the other hand, because Bayes theorem also predicts a low false-negative rate in this setting, the test is not totally without value. If the test were negative, a physician could conclude with very high certainty that the patient does not have coronary artery disease because Bayes theorem predicts a low false-negative rate in this setting. Proper application and interpretation of stress echocardiography are, therefore, essential in the pediatric population (Table 34.1).
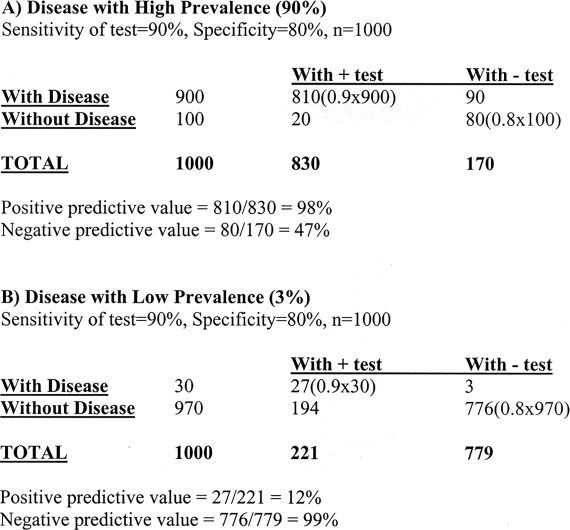
FIGURE 34.2. In general, diagnostic tests are evaluated by their sensitivity (the proportion of patients with disease who have a positive test) and specificity (the proportion of patients without the disease who have a negative test). However, Bayes theorem demonstrates that even with good sensitivity and specificity, a test may have limited clinical usefulness. Positive predictive value (the probability that a person with a positive result actually has the disease) and negative predictive value (the probability that person with a negative result does not have the disease) are better measures of overall clinical usefulness of a test, because they incorporate information on both the test (i.e., sensitivity and specificity) and the population being tested (i.e., prevalence). With high prevalence of disease in the population being tested (90% in Example A here), of 1000 patients, 900 will have the disease and 100 will not. A test with 90% sensitivity and 80% specificity will correctly identify 810 of the 900 patients with disease (90% of 900) and 80 of the 100 patients without disease (80% of 100). Bayes theorem demonstrates that the test has excellent positive predictive value; the likelihood of disease in a patient with a positive test is very high. On the other hand, a negative test would not rule out the disease; the patient would still have more than a 50% chance of having the disease. With low prevalence of disease (3% in Example B here), the test with the same sensitivity and specificity has poor positive predictive value. In other words, it is likely that a patient with a positive test does not have the disease. The test, therefore, would not be useful as a screening test because it would not be able to identify diseased individuals. On the other hand, a patient with a negative test result would be virtually ensured of not having the disease.
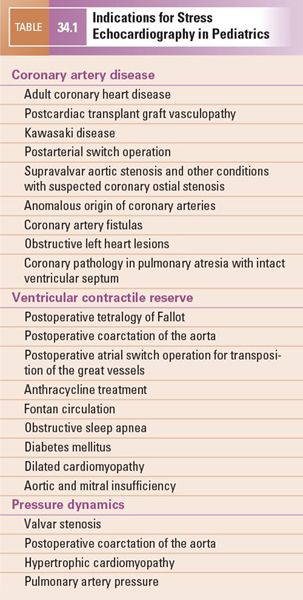
Coronary Artery Disease
Like most pathology, coronary artery disease consists of an anatomic substrate with physiologic consequences. It is important to assess both aspects of coronary pathology because even an impressive coronary artery narrowing may have minor or no physiologic consequences as a result of the development of collateral circulation. Intervention in such a case may be unwarranted because it will not improve physiology any more than has already occurred with the natural development of these collateral vessels. Before the advent of stress echocardiography, clinicians were only able to assess the anatomic severity of coronary artery disease. Diagnostic modalities such as coronary arteriography yield detailed images of coronary anatomy but reveal little information regarding actual myocardial perfusion. The application of stress echocardiography provides assessment of physiologic severity of coronary artery disease because it evaluates the degree of compromise in myocardial perfusion for any given anatomic abnormality. A main indication for performing stress echocardiography, therefore, is determining the physiologic significance of anatomically abnormal coronary arteries.
The child with adult coronary heart disease Much emphasis has appropriately been placed on providing care for the adult with congenital heart disease. Because congenital heart surgery survival rates have markedly improved, this heretofore relatively small population is growing.
A parallel situation is occurring in the pediatric population. It is known that the atherosclerotic process begins in childhood. For most children, vascular involvement has been minor, so that treatment has been preventive. However, in some disease states, such as familial hypercholesterolemia, diabetes mellitus, chronic kidney disease, Kawasaki disease, and rheumatologic diseases, the childhood atherosclerotic process is hastened, leading to coronary events in childhood. An even more disturbing problem is that society is in the midst of a childhood obesity epidemic, which is accelerating this process even in children without other disease. Not only has childhood obesity resulted in more adults with cardiovascular disease, but it has also caused adverse cardiovascular risk factor changes during childhood. The presence of coronary artery disease and risk factors in children has resulted in a burgeoning of a heretofore uncommon pediatric population—the child with adult coronary artery disease, which similarly finds itself in the pediatric-adult netherworld previously reserved only for adult patients with congenital heart disease. Recent reports demonstrate that myocardial infarction may occur in adolescents. In children with coronary risk factors such as insulin-dependent diabetes mellitus, left ventricular wall motion is compromised at an age as young as 10 years. The etiology of this remains unclear but may be related to damaged endothelial function. Stress echocardiography will be an important diagnostic tool in evaluating this population.
Post cardiac transplant coronary artery disease Coronary artery pathology in children is most prevalent in the post cardiac transplant population. Transplant graft vasculopathy remains a major cause of late transplant mortality because it can result in chronic graft failure and arrhythmogenic sudden death. The disease is insidious and rapidly progressive. Because the coronary arteries are affected in a diffuse manner, the sensitivity of coronary angiography, which relies on having normal coronary segments adjacent to diseased segments for diagnosis of arterial disease, is imperfect, and more accurate surveillance methods have been required. Intracoronary ultrasound is likely the most sensitive method but it is invasive and may also produce false-negative results. Dobutamine stress echocardiography has proved to be the most sensitive noninvasive test in detecting its presence and has been recommended by the American Heart Association as a means to follow these patients.
Kawasaki disease Myocardial perfusion may be impaired in patients who have had Kawasaki disease because of thrombosed aneurysms and/or strictures at aneurysm sites. In addition, there is evidence that patients without any echocardiographic coronary artery involvement have abnormal endothelial function, putting them at risk for early atherosclerotic heart disease. Stress echocardiography using both exercise and dobutamine has proved effective in following these patients for myocardial perfusion abnormalities. In addition, dobutamine stress echocardiography has been useful in the risk stratification of patients with coronary artery aneurysms and stenoses. Specifically, using dobutamine stress echocardiography, it has been shown that patients in the lowest four American Heart Association risk levels are unlikely to have coronary perfusion abnormalities. Patients in the highest risk level (Category 5) may or may not have perfusion abnormalities, depending on the presence/absence of collateral circulation. Kawasaki disease is another example of how coronary artery physiology may be different in children versus adults. Children and adolescents may have very impressive coronary artery obstruction but have normal stress tests because of the development of collateral vessels. In most of these instances, bypass grafting would not be indicated. Stress echocardiography is an important tool in differentiating those patients who need revascularization from those who may safely undergo observation alone.
Arterial switch operation for transposition of the great vessels The arterial switch operation involves reimplanting the coronary arteries from the native aorta to the main pulmonary artery stump (the neoaorta). Following the arterial switch operation, coronary artery lesions are common and progressive, necessitating routine serial evaluation of perfusion with stress testing and sometimes resulting in the need for revascularization. In addition, stress echocardiography has been able to detect perfusion abnormalities in the absence of symptoms or arteriographic stenoses. The significance of such findings has yet to be determined; a constant finding in these patients is right coronary artery dominance with a hypoplastic distal left anterior descending coronary artery, which may result in the perfusion abnormality. Interestingly, these abnormalities are usually not present after the Ross operation, a procedure that also involves coronary reimplantation.
Coronary ostial stenosis Ischemia can occur in patients with supravalvar aortic stenosis, particularly those with Williams syndrome, because of coronary ostial stenosis, fusion of an aortic valve leaflet to the supravalvar ridge, or diffuse left main coronary artery narrowing. Coronary ostial stenosis may also be seen with an anomalous origin of the left coronary artery from the right sinus of Valsalva or in patients with transposition of the great vessels. This pathology may be very difficult to diagnose angiographically because the catheter is usually engaged in the coronary artery downstream from the narrowing. Stress echocardiography may therefore be particularly helpful in these individuals.
Other congenital heart disease Dobutamine and dipyridamole stress echocardiography has been useful in delineating the need for surgical management of anomalous origin of the left coronary artery from the pulmonary artery and in documentation of ischemia in coronary artery fistula. Other anomalies of the coronary artery origins such as the left main coronary artery from the right sinus of Valsalva or the circumflex coronary artery from the right main coronary artery have a higher incidence of atherosclerosis. Obstruction of left heart structures (valvar aortic stenosis, coarctation of the aorta, hypertrophic cardiomyopathy) is also associated with premature atherosclerosis. Finally, infants with pulmonary atresia and intact ventricular septum may have right ventricular-dependent coronary circulation and focal areas of coronary narrowing or frank coronary arterial interruption or aortocoronary atresia. Stress echocardiography could help to risk stratify these patients.
Ventricular Contractile Reserve
A second indication for stress echocardiography is in the evaluation of ventricular reserve. The contractile response to exogenous catecholamines has prognostic value. Patients with compromised ventricular function have elevated circulating catecholamines, decreased myocardial beta-receptor density, and downregulation of myocardial receptors and, therefore, have minimal response to exogenous catecholamines. Patients with better ventricular performance will have better beta-receptor responsiveness and better response to catecholamine administration. The magnitude of augmentation of cardiac performance during cardiovascular stress is the contractile reserve.
Measurement of left ventricular contractile reserve by stress echocardiography has been helpful in the detection and management of subclinical compromise of ventricular function in pediatric patients at risk for cardiomyopathy. For instance, stress echocardiography has shown that right and left ventricular reserve is depressed in children following repair of tetralogy of Fallot. In children after coarctation of the aorta repair, the resting left ventricular function is enhanced relative to control patients but contractile reserve is preserved (Fig. 34.3). Other investigators have shown that stress echo can detect subclinical left ventricular dysfunction in childhood cancer survivors who have received cardiotoxic chemotherapeutic agents. Some investigators have combined echocardiography with catheter-derived intracardiac pressure measurements during exercise to provide sophisticated contractility data helpful in differentiating mechanisms of ventricular reserve in congenital left-sided lesions. In patients after Fontan operation as the result of single-ventricle physiology, exercise echocardiography demonstrates normal increases in stroke and cardiac index during exercise until late submaximal levels, at which point these indices decrease. In patients who have undergone atrial switch operations for transposition of the great vessels, it has been shown with dobutamine stress magnetic resonance imaging that right ventricular contractile reserve correlates and is a key determinant of exercise capacity. In patients with atrial switch and with decreased right ventricular reserve by dobutamine stress echocardiography, brain natriuretic peptide is elevated, suggesting that either test may be able to predict future cardiovascular compromise.
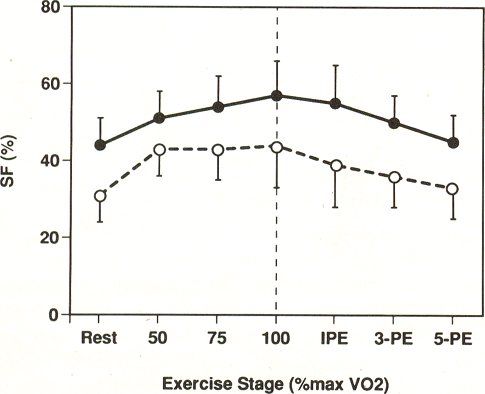
FIGURE 34.3. Despite elevated left ventricular function at rest, contractile reserve in postoperative coarctation of the aorta patients (filled circles) is maintained relative to that in control children (open circles
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


