Replacement of dysfunctional native cardiac valves is very common in the practice of congenital heart disease. A subset of patients with congenital heart disease will require multiple “re-replacements” of valvular prostheses secondary to growth or prosthesis degeneration. Therefore, appropriate longitudinal evaluation of prosthetic valves is critical to clinical practice. Transthoracic echocardiography is the most useful tool in the routine evaluation of valve prostheses, but transesophageal echocardiography, cardiac catheterization, and fluoroscopy are all important adjuncts to the clinical evaluation of a dysfunctional prosthesis. As a reference for longitudinal follow-up, a transthoracic echocardiogram should be obtained early after valve implantation in all patients.
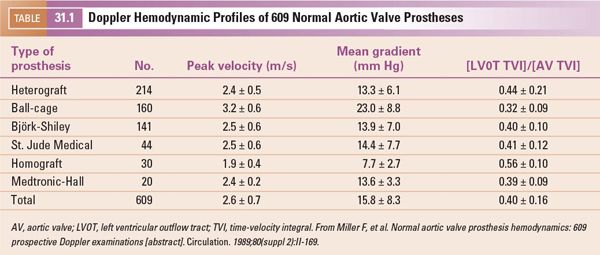
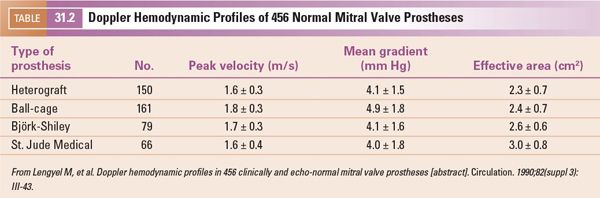
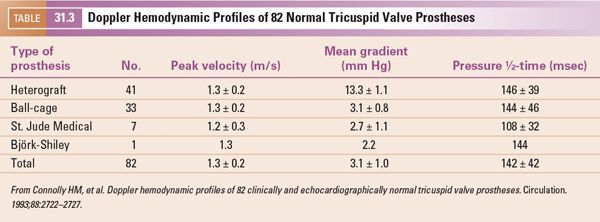
Prosthetic valves can be divided into two large categories: tissue and mechanical. The tissue prostheses include porcine or bovine heterografts and human allografts/homografts (Fig. 31.1). The mechanical prostheses include tilting disc prosthetics (e.g., the St. Jude bileaflet and the Medtronic-Hall single disc) and the ball-cage prosthesis (e.g., the Starr-Edwards) (see Fig. 31.1). To accurately interpret echocardiographic findings, the exact type and size of the prosthesis should be known, as the various valve types demonstrate different hemodynamic profiles (Tables 31.1 through Table 31.4) and regurgitation characteristics. Prosthetic valve dysfunction may be caused by valve thrombosis, pannus formation, senescent changes (bioprostheses), and infection (Fig. 31.2).
EVALUATION OF THE MITRAL PROSTHESIS
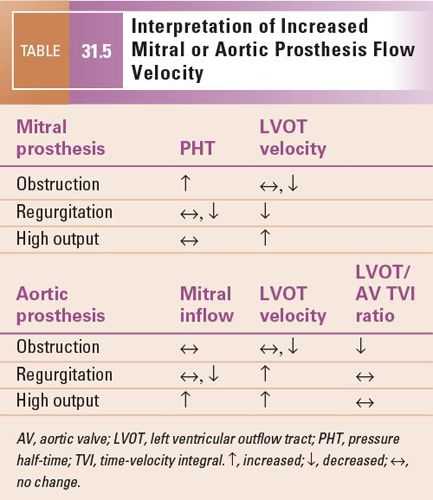
Doppler interrogation of a mitral prosthesis is crucial in determining the functional status of the valve. However, the transthoracic echocardiographic evaluation of a mitral prosthesis should begin with a two-dimensional evaluation of valve stability and surrounding structures. A large vegetation, thrombus, or valve dehiscence can be identified. The leaflets of a bioprosthetic valve can be evaluated for symmetric excursion and evidence of calcification. The mechanical mitral prosthesis produces reverberation artifact, which limits the two-dimensional interrogation of the prosthesis itself and the surrounding structures, especially the left atrium (Fig. 31.3). Flow velocity through the prosthetic valve and determination of the maximal and mean pressure gradients should be obtained using continuous-wave Doppler interrogation. The pressure gradient can be elevated secondary to valve stenosis, regurgitation, or increased cardiac output. The pressure half-time measurement and the left ventricular outflow tract (LVOT) velocity can help distinguish between these two scenarios. The pressure half-time should be prolonged if the valve is obstructed, but normal or shortened if the increased pressure gradient across the valve is secondary to regurgitation. The LVOT velocity will be decreased if the increased velocity across the mitral prosthesis is secondary to severe regurgitation, as the forward flow across the LVOT will be decreased (Table 31.5). It is important to recall that the pressure half-time method used to determine the area of a native mitral valve will overestimate the area of a mitral prosthesis. If there is no significant aortic or mitral regurgitation, the continuity equation is a valid and more optimal method for determining the area of a mitral prosthesis. The continuity equation for this calculation is as follows:
MP area = LVOT area × ([LVOT TVI]/[MP TVI])
= LVOT diameter2 × 0.785 × ([LVOT TVI]/[MP TVI])

Figure 31.1. Prosthetic valves. A: St. Jude bileaflet mechanical prosthesis. B: Starr-Edwards prosthesis. C: Porcine bioprosthesis.
where MP is mitral prosthesis, LVOT TVI is the LVOT time-velocity integral, and MP TVI is the time-velocity integral of the mitral prosthesis inflow velocity obtained by continuous-wave Doppler.
Regurgitation should be evaluated with color flow imaging, spectral Doppler interrogation, and two-dimensional evaluation of the valve. If there is regurgitation, it is important to distinguish periprosthetic regurgitation from prosthetic regurgitation (Fig. 31.4), as the mechanism for each is different. The degree of regurgitation should then be assessed. The degree of prosthetic regurgitation can be assessed both by semiquantitative methods and quantitative methods (proximal isovelocity surface area [PISA]) if the jet is well seen. Severe regurgitation is indicated by the following:
1.Increased mitral inflow peak velocity 2.5 m/s or greater with normal mitral inflow pressure half-time (≤150 m/s)
2.Dense mitral regurgitant continuous-wave Doppler signal
3.Regurgitant fraction 55% or greater
4.Systolic Doppler flow reversals in the pulmonary vein
While prosthetic regurgitation can be detected by color flow imaging, the mechanical mitral prosthesis poses special challenges. The artifact produced in the left atrium may limit the ability to detect even significant degrees of prosthetic and periprosthetic regurgitation. In this situation, indirect indicators of significant regurgitation should be used. These include two-dimensional evidence of valve instability or periprosthetic tissue changes, increased left ventricular dimension, increased inflow gradient with a normal or reduced pressure half-time, and decreased LVOT velocity. Transesophageal echocardiography is very useful in defining the presence and degree of mechanical mitral prosthesis regurgitation (Fig. 31.5), as the posterior-to-anterior direction of the ultrasound beam allows visualization of the left atrium without imaging artifact.
When evaluating a prosthesis for regurgitation, it must be remembered that a small degree of prosthetic regurgitation is inherent for most mechanical prostheses. The Doppler fingerprint of this regurgitation varies by prosthesis type. A Medtronic-Hall prosthesis has one central jet of regurgitation, the St. Jude Medical mechanical prosthesis has two side jets and one central jet, the Starr-Edwards prosthesis has two curved side jets, and the Björk-Shiley prosthesis has two unequal side jets (Fig. 31.6). These normal regurgitant jets should be small, with a jet area <2 cm2 and a jet length <2.5 cm. Periprosthetic regurgitation is always abnormal. It may be a small amount of regurgitation related to a gap in the sutures placed at the anastomosis, or it may be secondary to an infectious process with perivalvular extension. Periprosthetic regurgitation that is significant may require treatment. Surgical intervention has traditionally been required, but transcatheter placement of devices to eliminate periprosthetic leakage is now possible in selected patients who are not surgical candidates without evidence of active infection (Fig. 31.7, Video 31.1).
EVALUATION OF THE AORTIC PROSTHESIS
An aortic valve prosthesis should be evaluated with an approach similar to the evaluation of the mitral prosthesis, with a few caveats. The spectral Doppler assessment of the left ventricular outflow tract and the aortic valve are usually best obtained with transthoracic imaging. Transesophageal imaging often does not allow optimal alignment of the Doppler beam to obtain the most accurate velocities through the valve and outflow tract. Left ventricular size, wall thickness, and function are also often most reliably measured during transthoracic imaging. Regurgitation can be demonstrated by both transthoracic and transesophageal imaging, but anterior periprosthetic jets are best seen on transthoracic images and posterior jets are best demonstrated by transesophageal images secondary to the location of the transducer and the artifact produced by the valve. Transesophageal images in general are better for the detection of a vegetation.
Obstruction of an aortic prosthesis results in increased flow velocity across the prosthesis and is best quantitated by Doppler echocardiography. Doppler interrogation should be performed in multiple imaging windows to obtain the maximal velocity across the prosthesis. To completely evaluate the prosthesis, continuous-wave Doppler should be obtained. From the highest velocity signal, a maximum instantaneous pressure gradient and a mean pressure gradient should be calculated. Pulsed-wave Doppler interrogation of the LVOT and measurement of the LVOT TVI is critical in determining the etiology of the increased blood flow velocity across the aortic prosthesis. Care should be taken to place the Doppler sample volume for this measurement below the area of flow acceleration. If the valve is truly obstructed, the LVOT velocity should not be increased. If the increased velocity across the valve is secondary to aortic regurgitation or a high output state, the LVOT velocity will be increased. The ratio of LVOT velocity or TVI versus AV velocity or TVI is helpful. If the prosthesis is obstructed, the ratio decreases (LVOT TVI/AV TVI ≤0.2 with normal 0.3; see Table 31.2).
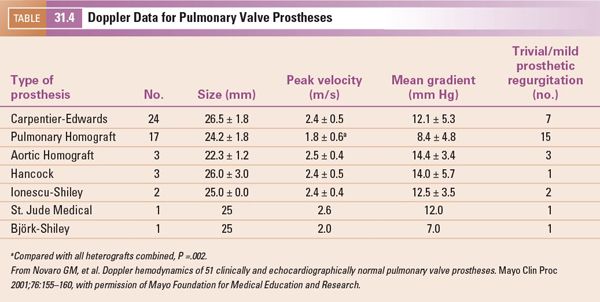
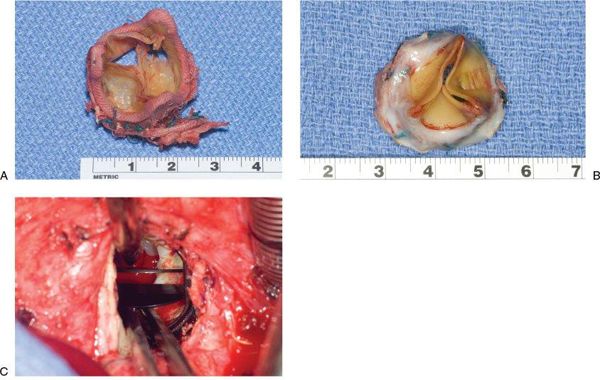
Figure 31.2. Prosthetic valve dysfunction. A: Bioprosthetic valve with cusp perforation secondary to senescent changes. B: Bioprosthetic valve with severe cusp thickening. C: Mechanical valve compromised by pannus formation.
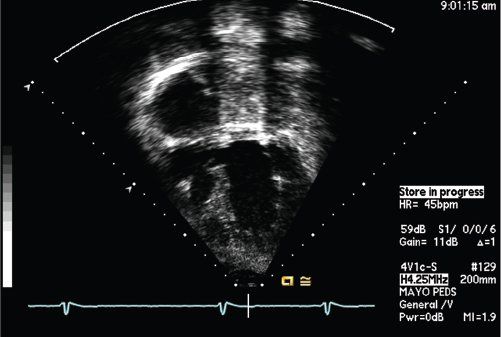
Figure 31.3. Apical four-chamber view showing reverberation artifact obscuring the left atrium in a patient with a mechanical mitral prosthesis.
The area of the aortic prosthesis can be estimated by the continuity equation as follows:
AP area = LVOT area × ([LVOT TVI]/[AP TVI])
= SROD2 × 0.785 × ([LVOT TVI]/[AP TVI])
where AP is aortic prosthesis and SROD is sewing ring diameter.
Evaluation of aortic prosthetic regurgitation should include two-dimensional evaluation of the valve and surrounding structures, color flow imaging to determine the jet characteristics and location (prosthetic versus periprosthetic), pressure half-time of the regurgitant jet, mitral inflow pattern, diastolic reversal flow in the descending thoracic aorta, and regurgitation fraction (if the jet is suitable for quantification). The normal regurgitation patterns of mechanical prosthetic valves should be kept in mind so as not to be confused with pathologic regurgitation. Severe aortic valve regurgitation is indicated by the following.
1.Pressure half-time of regurgitant jet of 250 ms or less
2.Restrictive mitral inflow pattern (if the aortic regurgitation is acute)
3.Holodiastolic flow reversal in the descending thoracic aorta Doppler signal
4.Regurgitant fraction of 55% or greater
EVALUATION OF TRICUSPID AND PULMONARY PROSTHESES
Tricuspid and pulmonary valve replacements are common in patients with congenital heart disease. The evaluation of these prostheses is analogous to the evaluation of the aortic and mitral prosthetic valves, with a few exceptions. The tricuspid and pulmonary valves are usually anterior structures. Therefore, imaging of these valves is often best with transthoracic imaging. The posterior location of the echo transducer in transesophageal imaging can diminish the ability to evaluate these anterior structures. If transesophageal imaging is used, transgastric images are usually best for evaluation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


