Potential upstream determinants of coronary heart disease (CHD) include life-course socioeconomic position (e.g., childhood socioeconomic circumstances, own education and occupation); however, several plausible biological mechanisms by which socioeconomic position (SEP) may influence CHD are poorly understood. Several CHD risk factors appear to be more strongly associated with SEP in women than in men; little is known as to whether any CHD risk factors may be more strongly associated with SEP in men. Objectives were to evaluate whether cumulative life-course SEP is associated with a measurement of subclinical atherosclerosis, the ankle–brachial index (ABI), in men and women. This study was a prospective analysis of 1,454 participants from the Framingham Heart Study Offspring Cohort (mean age 57 years, 53.8% women). Cumulative SEP was calculated by summing tertile scores for father’s education, own education, and own occupation. ABI was dichotomized as low (≤1.1) and normal (>1.1 to 1.4). After adjustment for age and CHD risk factors cumulative life-course SEP was associated with low ABI in men (odds ratio [OR] 2.04, 95% confidence interval [CI] 1.22 to 3.42, for low vs high cumulative SEP score) but not in women (OR 0.86, 95% CI 0.56 to 1.33). Associations with low ABI in men were substantially driven by their own education (OR 4.13, 95% CI 1.86 to 9.16, for lower vs higher than high school education). In conclusion, cumulative life-course SEP was associated with low ABI in men but not in women.
Very little is known about whether life-course socioeconomic position (SEP) is associated with the ankle–brachial index (ABI), a subclinical measurement of atherosclerosis. ABI is the ratio of systolic blood pressure in the ankle to systolic blood pressure in the arm. It is well recognized that ABI is a measurement of generalized atherosclerosis and that an ABI <0.9 indicates peripheral arterial disease. In the Atherosclerosis Risk In Communities (ARIC) study and in a systematic review including longitudinal studies from the United States and Europe, low ABI was associated with increased incidence of total mortality, cardiovascular mortality, myocardial infarction, and stroke. The increased relative risks were shown to be independent of baseline cardiovascular disease and risk factors, suggesting that the ABI might have an independent role in predicting cardiovascular events. Consequently, the primary objective of this study was to investigate whether cumulative life-course SEP is associated with ABI in the Framingham Offspring Study cohort independent of classic coronary heart disease (CHD) risk factors.
Methods
The Framingham Heart Study is a community-based observational cohort study initiated in 1948 to investigate risk factors for CHD. The present investigation was based on participants in the Framingham Offspring Study, which began in 1971 with recruitment of 5,124 United States men and women who were offspring (or spouses of offspring) of the original cohort of the Framingham Heart Study. The design and selection criteria of the Framingham Offspring Study have been described elsewhere. Participants were examined every 4 to 8 years, undergoing medical history, physical examination, anthropometry, and laboratory assessment of CHD risk factors at each examination, as previously described. Framingham Study participants signed informed consent and the Framingham Study is reviewed annually by the Boston University Medical Center institutional review board.
Childhood SEP was measured by father’s educational attainment in primary analyses and father’s occupation in secondary analyses. Father’s education and occupation were obtained directly from the participants’ fathers who were enrolled in the Framingham Heart Study original cohort from 1948 through 1950 (mean age 44 years, range 28 to 62). Father’s education was categorized as 3 levels: lower than high school, completed high school, and higher than high school. Father’s occupation was categorized as 3 levels: laborer, clerical/sales, and professional/executive/supervisory/technical. Young adulthood SEP was measured by own educational attainment, obtained directly from the Framingham Offspring Study participants at examinations 2 (1979 to 1982) and 3 (1984 to 1987). Education was categorized as 3 levels: ≤12, 13 to 16, and ≥17 years of education. Active professional-life SEP was measured as own occupation, ascertained at examination 2 (1979 to 1982), and categorized as 3 levels: laborer, homemaker/clerical/sales, and professional/executive/supervisory/technical. Analyses testing the accumulation-of-risk framework used a cumulative SEP score that was created by summing values for SEP at 3 successive life-course periods: childhood SEP (measured as father’s education: lower than high school = 0, high school = 1, higher than high school = 2), young adulthood SEP (measured as own education: ≤12 years = 0, 13 to 16 years = 1, ≥17 years = 2), and active professional-life SEP (measured as own occupation: laborer = 0, clerical/sales/homemaker = 1, executive/professional/supervisory/technical = 2). Cumulative SEP score was categorized as low (score of 0 or 1), medium (score of 1 or 2), and high (score of 4 to 6) for analyses. Higher cutpoints were used for educational categories of offspring compared to fathers to account for secular trends of increased normative levels of education across generations.
Measurements of ABI were obtained at offspring examination 6 (1995 to 1998). Ankle–brachial systolic blood pressure measurements were performed by trained technicians according to standardized protocols. Systolic blood pressure was measured using an 8-MHz Doppler pen probe and an ultrasonic Doppler flow detector (Parks Medical Electronics, Inc., Aloha, Oregon) 2 times for each limb (right arm, left arm, right ankle, left ankle). ABI was then calculated for each leg as the ratio of average systolic blood pressure in the ankle divided by average systolic blood pressure in the arm with the higher blood pressure. The lower of the ABI values calculated for the left and right ankles was used for analyses. If ABI was missing for 1 ankle, data from the nonmissing ankle were used (n = 8 for the present investigation).
Emerging evidence has demonstrated increased risk for coronary and carotid atherosclerosis, coronary events, and cardiovascular disease mortality with ABI values up to 1.1. Consequently the ABI Collaboration defined normal ABI as >1.1 to 1.4. Therefore, ABI was dichotomized as low (ABI ≤1.1) versus normal (ABI >1.1 to 1.4) for the present investigation. However, additional analyses were carried out for women using a lower cutpoint of 1.0 to define low ABI. This was done in light of recent evidence suggesting that normal ABI values may be intrinsically lower in healthy women than in men. Participants with ABI values >1.4 were excluded because an ABI >1.4 has been demonstrated to confer increased risk for cardiovascular and total mortality, possibly because of poor arterial compressibility resulting from stiffness and calcification. Because of a very small number of subjects (n = 41) with an ABI value ≤0.9 (i.e., definite peripheral arterial disease), there was inadequate statistical power to carry out analyses with ABI dichotomized as ≤0.9 versus >0.9 to 1.4.
All covariates were measured at offspring examination 6 (1995 to 1998). Smoking status (current, former, or never) was determined by self-report. Systolic blood pressure was calculated as the average of the clinic physician’s 2 measurements of systolic blood pressure while a subject was seated. Body mass index was calculated as weight in kilograms divided by the square of height in meters. High-density lipoprotein (HDL) and total cholesterol concentrations were measured by automated enzymatic techniques. Participants were considered to have diabetes if they reported receiving treatment with insulin or a hypoglycemic agent or if they had fasting plasma glucose levels ≥126 mg/dl (7.0 mmol/L). Participants who were missing information on treatment status or fasting glucose were classified as having diabetes if they had a nonfasting glucose concentration ≥200 mg/dl (11.1 mmol/L), or a nonfasting glucose concentration from 126 to 200 mg/dl plus a history of diabetes, or if nonfasting glucose concentration was 126 to 200 mg/dl with a diabetes diagnosis at a subsequent Framingham examination. Use of antihypertensive and cholesterol-lowering medication was self-reported. Depressive symptomatology was measured using the Center for Epidemiologic Studies Depression scale (range 0 to 51).
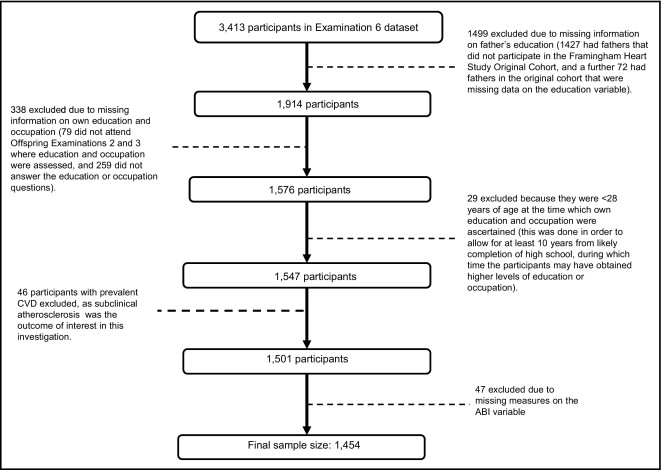
There were 3,413 participants in the dataset who completed offspring examination 6, on which the present investigation was based. After implementation of exclusion criteria (details shown in Figure 1 ), the final sample was 1,454 (782 women and 672 men). Cardiovascular disease events (as part of exclusion criteria) were identified in participants since the onset of the Framingham Offspring Study (1971 to 1975) and included recognized myocardial infarction, coronary insufficiency, cerebrovascular events (including cerebral atherothrombotic infarction, cerebral embolism, intracerebral hemorrhage, subarachnoid hemorrhage, and other cerebrovascular accident), and congestive heart failure. Those excluded (n = 1,913) were more likely to be older (mean age 60.0 vs 57.2 years, respectively, p <0.0001), to be taking antihypertensive medication (31.6% vs 23.5%, p <0.0001) and cholesterol-lowering medication (15.2% vs 10.0%, p <0.0001), and to be diabetic (11.3% vs 8.4%, p = 0.006). Included and excluded participants did not differ significantly for other variables including gender, body mass index, HDL/total cholesterol ratio, depression score, and current smoking.
Age-adjusted means and proportions were calculated for baseline covariates and compared across cumulative SEP categories. Multivariable logistic regression analyses evaluated associations between cumulative SEP (categorized as low [score of 0 or 1], medium [score of 1 or 2], and high [score of 4 to 6] as described earlier) and ABI (≤1.1 vs >1.1 to 1.4 for primary analyses, ≤1.0 vs >1.0 to 1.4 for secondary analyses in women). All analyses were adjusted for age. Subsequent models were also adjusted for the CHD risk factors smoking, body mass index, systolic blood pressure, total/HDL cholesterol ratio, antihypertensive medication, cholesterol-lowering medication, depressive symptomatology, and diabetes. Further analyses of individual SEP measurements (father’s education, own education, own occupation) in relation to ABI were performed to evaluate whether SEP at any of these life-course periods particularly contributed to associations of cumulative SEP with ABI. These latter analyses were adjusted for age with subsequent adjustment for other individual SEP measurements and final adjustment for the CHD risk factors described earlier. All analyses performed were gender-specific because there was evidence of effect modification by gender (p = 0.01 for interaction between cumulative SEP score and gender). Generalized estimating equations were used to account for clustering of outcomes by family. Pearson correlation coefficients and variance inflation factors were used to evaluate colinearity, and no evidence of colinearity was found. The 3 primary SEP variables (father’s education, own education, and own occupation) were not correlated highly enough to be of concern when simultaneously including all 3 in a single multivariable model (pairwise correlation coefficients ranged from 0.25 to 0.51). Power analyses were performed using PS Power and Sample Size Calculation 3.0.2 (Dupont and Plummer, Vanderbilt University, Nashville, Tennessee) according to methods for cohort studies with dichotomous outcomes.
Results
Participants in the study sample had a mean age of 57 years (range 38 to 80) and 53.8% were women. Mean ABIs ± SDs were 1.16 ± 0.10 in men and 1.09 ± 0.10 in women (p <0.0001). Prevalences of low ABI defined as ≤1.1 were 21% in men and 49% in women; low ABI defined as ≤1.0 demonstrated prevalences of 4.8% in men and 16% in women. In age-adjusted analyses in men lower cumulative SEP was associated with older age, lower ABI, higher body mass index, lower HDL cholesterol, higher total/HDL cholesterol ratio, higher prevalence of current smoking, and higher depression score. In women lower cumulative SEP was associated with older age, higher body mass index, lower HDL cholesterol, higher total/HDL cholesterol ratio, higher prevalence of diabetes and current smoking, and higher depression score ( Table 1 ). In addition, R 2 from univariate linear regression analyses showed that cumulative SEP explained 1.4% of the variance in ABI in men and 0.7% of the variance in women. Examples of the contribution of other specific CHD risk factors to the variance (R 2 ) in ABI were smoking (5.5% in men, 3.0% in women), hypertension medication (2.9% in men, 1.8% in women), systolic blood pressure (1.5% in men, 4.1% in women), and diabetes (1.3% in men, 0.1% in women).
| Cumulative SEP Score | |||
|---|---|---|---|
| 0 or 1 | 2 or 3 | 4–6 | |
| Men | 192 (28.6%) | 189 (28.1%) | 291 (43.3%) |
| Age (years) ⁎ | 58.9 (57.63–60.2) | 56.3 (55.1–57.6) | 55.6 (54.7–56.5) |
| Mean ankle–brachial index | 1.15 (1.14–1.16) | 1.15 (1.14–1.17) | 1.17 (1.16–1.19) |
| Body mass index (kg/m 2 ) | 29.0 (28.3–29.6) | 29.0 (28.3–29.6) | 28.2 (27.7–28.8) |
| Systolic blood pressure (mm Hg) | 128.1 (125.9–130.3) | 129.6 (127.4–131.7) | 128.5 (126.8–130.3) |
| High-density lipoprotein cholesterol (mg/dl) | 42.9 (41.1–44.8) | 43.1 (41.3–44.9) | 45.3 (43.8–46.8) |
| Total/high-density lipoprotein cholesterol ratio | 5.1 (4.8–5.4) | 5.4 (5.1–5.8) | 4.7 (4.4–5.0) |
| Antihypertensive medication use | 23.4% (17.8–30.0) | 26.9% (20.9–34.0) | 22.1% (17.6–27.5) |
| Cholesterol-lowering medication | 11.4% (7.6–16.6) | 12.3% (8.3–17.8) | 10.4% (7.3–14.5) |
| Diabetes mellitus | 9.4% (6.0–14.4) | 7.2% (4.3–11.8) | 8.4% (5.7–12.3) |
| Current smoker | 15.4% (10.9–21.4) | 19.5% (14.4–25.9) | 10.0% (7.0–13.9) |
| Depression score | 5.3 (4.3–6.2) | 5.3 (4.4–6.3) | 3.9 (3.1–4.7) |
| Women | 230 (29.4%) | 318 (40.7%) | 234 (29.9%) |
| Age (years) ⁎ | 61.1 (60.0–62.3) | 56.1 (55.1–57.0) | 55.9 (54.8–57.1) |
| Mean ankle–brachial index | 1.08 (1.07–1.10) | 1.09 (1.08–1.11) | 1.09 (1.08–1.11) |
| Body mass index (kg/m 2 ) | 27.9 (27.1–28.6) | 27.6 (27.0–28.3) | 26.4 (25.7–27.2) |
| Systolic blood pressure (mm Hg) | 126.1 (123.8–128.5) | 126.4 (124.4–128.3) | 124.0 (121.8–126.3) |
| High-density lipoprotein cholesterol (mg/dl) | 56.8 (54.7–58.9) | 57.5 (55.7–59.2) | 60.9 (58.9–62.9) |
| Total/high-density lipoprotein cholesterol ratio | 4.1 (3.9–4.2) | 4.0 (3.9–4.2) | 3.7 (3.6–3.9) |
| Antihypertensive medication use | 23.9% (18.7–30.0) | 22.3% (17.9–27.4) | 14.9% (10.8–20.2) |
| Cholesterol-lowering medication | 8.8% (5.8–13.2) | 6.2% (4.0–9.5) | 6.4% (3.9–10.4) |
| Diabetes mellitus | 7.9% (5.0–12.1) | 7.4% (4.9–10.9) | 4.5% (2.5–8.1) |
| Current smoker | 25.2% (19.8–31.5) | 16.2% (12.6–20.7) | 11.5% (8.0–16.2) |
| Depression score | 8.5 (7.4–9.6) | 6.5 (5.6–7.5) | 5.2 (4.1–6.3) |
Age-adjusted logistic regression analyses showed that lower cumulative SEP across the life course was associated with greater prevalence of low ABI in men (odds ratio [OR] 2.00, 95% confidence interval [CI] 1.28 to 3.14, for low vs high cumulative SEP score) and not in women (OR 0.94, 95% CI 0.63 to 1.38; Table 2 ). Further adjustment for CHD risk factors did not attenuate the association in men (OR 2.04, 95% CI 1.22 to 3.42). In analyses of individual SEP measurements own education was associated with low ABI in men with associations remaining after adjustment for age, other SEP measurements, and CHD risk factors (OR 4.13, 95% CI 1.86 to 9.16, for ≤12 years of education vs ≥17 years; Table 3 ). Own occupation was also associated with low ABI in men in age-adjusted analyses. Further adjustment for other SEP measurements and CHD risk factors attenuated the association for the laborer category (OR 1.22, 95% CI 0.70 to 2.11) but not for the homemaker/clerical/sales category (OR 1.92, 95% CI 1.01 to 3.62). No significant associations were observed between father’s education and ABI in men ( Table 3 ). In women no association was observed between own education and ABI (OR 1.23, 95% CI 0.76 to 2.00) or between own occupation and ABI (OR 1.36, 95% CI 0.76 to 2.41; Table 4 ). However, father’s education in the lower-than-high-school category was weakly associated with a lower prevalence of low ABI after adjustment for other SEP measurements and CHD risk factors ( Table 4 ). Additional analyses with low ABI alternatively defined as ≤1.0 in women revealed somewhat higher effect sizes; however, associations were still not statistically significant ( supplementary Tables 1 and 2 , available online). Patterns of association for cumulative SEP when using father’s occupation as the measurement of childhood SEP were similar to results obtained when father’s education was used ( supplementary Table 3 , available online). In addition, associations between father’s occupation and ABI were not significant in men or women (data not shown), similar to analyses using father’s education.
| Cumulative SEP Score | Subjects | Number of Events With ABI ≤1.1 (%) | Model Adjustment | |||
|---|---|---|---|---|---|---|
| Model 1 ⁎ | Model 2 † | |||||
| OR | 95% CI | OR | 95% CI | |||
| Men | ||||||
| 0 or 1 | 192 | 52 (27.1%) | 2.00 | 1.28–3.14 | 2.04 | 1.22–3.42 |
| 2 or 3 | 189 | 45 (23.8%) | 1.81 | 1.13–2.92 | 1.51 | 0.87–2.62 |
| 4–6 | 291 | 42 (14.4%) | 1.00 | 1.00 | ||
| Women | ||||||
| 0 or 1 | 230 | 117 (50.9%) | 0.94 | 0.63–1.38 | 0.86 | 0.56–1.33 |
| 2 or 3 | 318 | 153 (48.1%) | 0.93 | 0.67–1.31 | 0.94 | 0.65–1.36 |
| 4–6 | 234 | 117 (50.0%) | 1.00 | 1.00 | ||
† Adjusted for age, smoking, body mass index, systolic blood pressure, total/high-density lipoprotein cholesterol ratio, antihypertensive medication, cholesterol-lowering medication, depressive symptomatology, and diabetes.
| SEP Measurement | SEP Level | Subjects | Number of Events With ABI ≤1.1 (%) | Model Adjustment | |||||
|---|---|---|---|---|---|---|---|---|---|
| Model 1 ⁎ | Model 2 † | Model 3 ‡ | |||||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | ||||
| Father’s education | Lower than high school | 331 | 72 (21.8%) | 1.07 | 0.69–1.66 | 0.75 | 0.45–1.23 | 0.67 | 0.38–1.19 |
| High school | 157 | 32 (20.4%) | 1.2 | 0.71–2.04 | 0.96 | 0.54–1.71 | 1.00 | 0.52–1.92 | |
| Higher than high school | 184 | 35 (19.0%) | 1.00 | 1.00 | 1.00 | ||||
| Own education | ≤12 years | 216 | 59 (27.3%) | 4.82 | 2.57–9.05 | 5.82 | 2.86–11.83 | 4.13 | 1.86–9.16 |
| 13–16 years | 270 | 67 (24.8%) | 4.53 | 2.45–8.38 | 4.59 | 2.44–8.64 | 3.28 | 1.64–6.55 | |
| ≥17 years | 186 | 13 (7.0%) | 1.00 | 1.00 | 1.00 | ||||
| Own occupation | Laborer | 234 | 57 (24.3%) | 1.55 | 1.02–2.35 | 0.92 | 0.57–1.50 | 1.22 | 0.70–2.11 |
| Homemaker, clerical, or sales | 84 | 24 (28.6%) | 1.91 | 1.10–3.32 | 1.40 | 0.79–2.51 | 1.92 | 1.01–3.62 | |
| Professional, executive, supervisory, or technical | 354 | 58 (16.4%) | 1.00 | 1.00 | 1.00 | ||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


