The relation between C-reactive protein (CRP) and coronary atherosclerosis is not fully understood. This study aims to investigate the associations among high-sensitivity CRP, coronary plaque burden, and the presence of high-risk coronary lesions as measured by intravascular ultrasound (IVUS) and 1-year cardiovascular outcome. Between 2008 and 2011, grayscale and virtual histology IVUS imaging of a nonculprit coronary artery was performed in 581 patients who underwent coronary angiography for acute coronary syndrome (ACS) or stable angina pectoris. Primary end point consisted of 1-year major adverse cardiac events (MACEs), defined as all-cause mortality, ACS, or unplanned coronary revascularization. After adjustment for established cardiac risk factors, baseline CRP levels were independently associated with higher coronary plaque burden (p = 0.002) and plaque volume (p = 0.002) in the imaged coronary segment. CRP was also independently associated with the presence of large lesions (plaque burden ≥70%; p = 0.030) but not with the presence of stenotic lesions (minimal luminal area ≤4.0 mm 2 ; p = 0.62) or IVUS virtual histology-derived thin-cap fibroatheroma lesions (p = 0.36). Cumulative incidence of 1-year MACE was 9.7%. CRP levels >3 mg/L were independently associated with a higher incidence of MACE (hazard ratio 2.17, 95% confidence interval [CI] 1.01 to 4.67, p = 0.046) and of all-cause mortality and ACS only (hazard ratio 3.58, 95% CI 1.04 to 13.0, p = 0.043), compared with CRP levels <1 mg/L. In conclusion, in patients who underwent coronary angiography, high-sensitivity CRP is a marker of coronary plaque burden but is not related to the presence of virtual histology-derived thin-cap fibroatheroma lesions and stenotic lesions. CRP levels >3 mg/L are predictive for adverse cardiovascular outcome at 1 year.
C-reactive protein (CRP) is a prognostic marker of cardiovascular outcome in patients with stable coronary artery disease and patients with acute coronary syndrome (ACS). Although CRP has also been postulated to reflect the extent of coronary atherosclerosis and plaque vulnerability, these relations are not yet fully understood. Previous studies have only shown weak associations between CRP and the extent of coronary artery disease on angiography and the degree of coronary calcification on computed tomography. Furthermore, the associations between CRP and the presence of high-risk vulnerable plaque morphology have not been investigated yet. Grayscale intravascular ultrasound (IVUS) imaging of the coronary arteries allows for accurate measurement of coronary plaque burden and plaque volume and identification of large or stenotic lesions. Additionally, intravascular ultrasound virtual histology (IVUS-VH; i.e., analysis of IVUS radiofrequency backscatter) allows tissue characterization and identification of virtual histology-derived thin-cap fibroatheroma (VH-TCFA) lesions. This study aims to investigate the associations between high-sensitivity CRP, coronary plaque burden, and presence of high-risk coronary lesions (i.e., VH-TCFA lesions, lesions with large plaque burden, and stenotic lesions) as measured by grayscale and radiofrequency IVUS and 1-year cardiovascular outcome.
Methods
The design of The European Collaborative Project on Inflammation and Vascular Wall Remodeling in Atherosclerosis–Intravascular Ultrasound (ATHEROREMO-IVUS) study has been described in detail elsewhere. In brief, 581 patients who underwent diagnostic coronary angiography or percutaneous coronary intervention (PCI) for ACS or stable angina pectoris have been included between 2008 and 2011 in the Erasmus MC, Rotterdam, The Netherlands. The ATHEROREMO-IVUS study was approved by the medical ethics committee of the Erasmus MC. The study was performed in accordance with the criteria described in the Declaration of Helsinki. Written informed consent was obtained from all included patients. This study is registered in ClinicalTrials.gov (number NCT01789411 ).
Blood samples were drawn from the arterial sheath before the coronary angiography procedure. The blood samples were stored at a temperature of −80°C within 2 hours after blood collection. CRP was measured in the stored serum samples (n = 576) using a immunoturbidimetric high-sensitivity assay (Roche Diagnostics Ltd, Rotkreuz, Switzerland) on the Cobas 8000 modular analyzer platform (Roche Diagnostics Ltd). The diagnostic range of this assay is 0.3 to 350 mg/L with a coefficient of variation of 1.3% at a mean value of 2.63 mg/L. In 5 patients, serum samples were not available for CRP measurement.
After the standard coronary angiography procedure, IVUS imaging of the most proximal part of a nonculprit coronary artery was performed. Selection of the nonculprit vessel was predefined in the study protocol. The order of preference for selection of the nonculprit vessel was (1) left anterior descending artery, (2) right coronary artery, and (3) left circumflex artery. All IVUS data were acquired with the Volcano s5/s5i Imaging System (Volcano Corp., San Diego, CA) using a Volcano Eagle Eye Gold IVUS catheter (20 MHz). An automatic pullback system was used with a standard pull back speed of 0.5 mm/s. The baseline IVUS images were sent to an independent core laboratory (Cardialysis BV, Rotterdam, The Netherlands) for offline analysis. The core laboratory personnel were blinded for baseline patient characteristics and clinical outcomes data. The grayscale IVUS and IVUS-VH analyses were performed using pcVH 2.1 and qVH (Volcano Corp.) software.
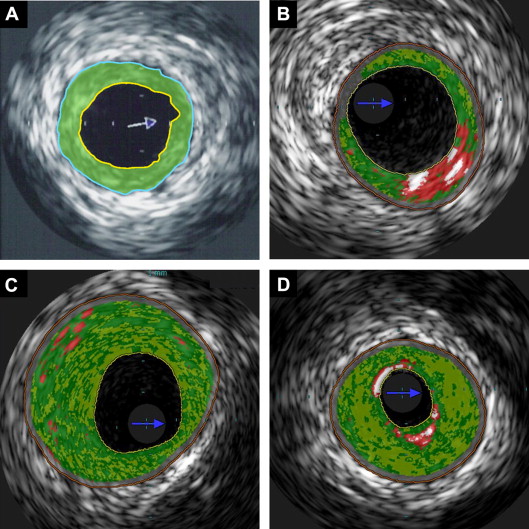
The external elastic membrane and luminal borders were contoured for each frame (median interslice distance, 0.40 mm). Extent and phenotype of the atherosclerotic plaque were assessed. Plaque burden was defined as plaque and media cross-sectional area divided by external elastic membrane cross-sectional area ( Figure 1 ). A coronary lesion was defined as a segment with a plaque burden of >40% in at least 3 consecutive frames. Using IVUS-VH, the composition of the atherosclerotic lesions was characterized into 4 different tissue types: fibrous, fibro-fatty, dense calcium, and necrotic core. Three types of high-risk lesions were identified: (1) VH-TCFA lesion, defined as a lesion with the presence of >10% confluent necrotic core in direct contact with the lumen in at least 3 consecutive frames; (2) lesion with large plaque burden, defined as a lesion with a plaque burden of ≥70% in at least 3 consecutive frames; and (3) stenotic lesion, defined as a lesion with a minimal luminal area of ≤4.0 mm 2 in at least 3 consecutive frames ( Figure 1 ).
Clinical follow-up started at inclusion and lasted 1 year. Postdischarge survival status was obtained from municipal civil registries. Postdischarge rehospitalizations were prospectively assessed during follow-up. Questionnaires focusing on the occurrence of major adverse cardiac events (MACEs) were sent to all living patients. Subsequently, hospital discharge letters were obtained, and treating physicians and institutions were contacted for additional information (i.e., discharge letters and coronary angiogram) whenever necessary. All events were adjudicated as related to a coronary site that was treated during the index procedure (culprit lesion-related event) or as related to a coronary site that was not treated during the index procedure (nonculprit lesion-related event). Events that were related to both the culprit lesion and a nonculprit site (e.g., revascularization of multiple vessels) were classified into both categories. When information was not sufficient to classify an event as either culprit lesion related or nonculprit lesion related, the event was classified as indeterminate. The end points were adjudicated by a clinical event committee that had no knowledge of the CRP and IVUS data.
The primary clinical end point was MACE, defined as all-cause mortality, ACS, or unplanned coronary revascularization. ACS was defined as the clinical diagnosis of ST-segment elevation myocardial infarction (STEMI), non-STEMI, or unstable angina pectoris in accordance with the guidelines of the European Society of Cardiology. Unplanned coronary revascularization was defined as unplanned repeat PCI (either culprit or nonculprit coronary artery) or coronary artery bypass grafting. The secondary end point was defined as the composite of all-cause mortality or ACS. Additional analyses were performed on nonculprit lesion-related and indeterminate events only (definite culprit lesion-related events were excluded in these analyses).
The distributions of the continuous variables, including CRP levels and the IVUS parameters, were tested for normality by visual examination of the histogram. CRP was not normally distributed and was, therefore, ln-transformed when analyzed as continuous variable. CRP levels were also categorized as low (<1 mg/L), average (1 to 3 mg/L), or high (>3 mg/L) according to the recommendations from the Centers for Disease Control and Prevention and the American Heart Association. Categorical variables are presented as numbers and percentages. We examined associations of CRP concentration with plaque burden, plaque volume, and presence of high-risk coronary lesions. Plaque volume was normalized for the imaged segment length (normalized plaque volume = plaque volume/imaged segment length × median segment length of study population). To test for trends, we used linear regression and logistic regression analyses with continuous ln-transformed CRP concentration as independent variable. Z test for heterogeneity was performed to test for differences in effect estimates between patients admitted with and without ACS. In multivariable analyses, the variables age, gender, diabetes mellitus, hypertension, hypercholesterolemia, smoking, peripheral artery disease, history of PCI, statin use at time of hospital admission, and indication for coronary angiography were considered as potential confounders (specifically, the variables age, gender, diabetes mellitus, hypertension, hypercholesterolemia, and smoking represent the traditional cardiac risk factors; the variables peripheral artery disease and history of PCI represent the presence of clinically manifest atherosclerosis; statin use may modulate baseline CRP levels; and the different indications for coronary angiography represent different patient risk classes) and were, therefore, entered into the each multivariate model.
Patients lost to follow-up were considered at risk until the date of last contact, at which time point they were censored. Cumulative event rates were estimated according to the Kaplan-Meier method. Cox proportional hazards regression analyses were performed to evaluate the associations between CRP and study end points. The final results are presented as crude and adjusted hazard ratios (HRs) with 95% confidence interval (CI). All data were analyzed with SPSS software (SPSS 20.0; IBM Corp., Armonk, NY). All statistical tests were 2 tailed, and p values <0.05 were considered statistically significant.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


