Patients with tetralogy of Fallot (TOF) have abnormal aortic properties. It is not known if this increases the risk for aneurysm formation. We sought to identify clinical and cardiovascular magnetic resonance (CMR) imaging patient characteristics associated with worsened aortic pulse wave velocity (PWV) and aortic strain in patients with repaired TOF. In 124 patients with TOF undergoing CMR (median age 24.6 years, interquartile range 17.8 to 34.2), left and right ventricular volumetric data, aortic PWV, and aortic strain were evaluated. Increased PWV positively correlated with age at repair (r = 0.3, p = 0.001) and cross-sectional ascending aortic area (r = 0.34, p <0.001) and was associated with a history of shunt placement (p = 0.01). Decreased aortic strain also correlated with age at TOF repair (r = −0.5, p <0.001), cross-sectional ascending aortic area (r = −0.43, p <0.001), aortic regurgitation (r = −0.46, p ≤0.001), and history of shunt placement (p <0.001). In a multivariate regression model controlling for history of shunt placement, use of cardiac medication, and aortic regurgitation, age at CMR was significantly associated with PWV (p = 0.005), whereas age at repair trended toward significance (p = 0.06). In conclusion, patients with TOF have abnormal aortic properties correlated with greater age, which may be associated with later repair. Longitudinal data are necessary to assess the risk of aortic aneurysm and dissection as the TOF population grows older. Functional imaging of the aorta by CMR may be useful in predicting risk and assessing vascular health.
Patients with repaired tetralogy of Fallot (TOF) are at risk for aortic pathology. Although longitudinal data are lacking in the TOF population, aortic dilatation in the general adult population is recognized as a crucial risk factor for dissection, a rare but highly lethal event. Aortic root replacement is a common practice when marked dilation occurs, but in patients with TOF, timing for this operation is variable and controversial because of unclear risk. Functional tests of the aorta, including measurements of stiffness and strain, are predictors of deteriorating vascular health. Pulse wave velocity (PWV) is a validated, accurate, and reproducible measure of arterial stiffness that can be used to predict poor cardiovascular outcomes. Likewise, aortic strain is an early marker of central arterial stiffness. In TOF, patients have been shown to have increased aortic stiffness as evidence of aortic pathology. However, contributing factors to aortic pathology are not fully understood in this population. We sought to describe patient characteristics and cardiovascular magnetic resonance (CMR) parameters associated with worsened aortic PWV and strain in patients with repaired TOF.
Methods
This retrospective study included a chart review of all patients with TOF who underwent CMR at the University of Michigan Congenital Heart Center from 2007 to 2011, as identified through the internal CMR database. Approval for this Health Insurance Portability and Accountability Act–compliant study was granted by the institutional review board. Informed consent was waived. Patients diagnosed with TOF including absent pulmonary valve, pulmonary atresia, and double-outlet right ventricle with subaortic ventricular septal defect and pulmonary stenosis were included in the analysis. Patients were excluded if they had repair after 20 years of age, exposure to sedation or anesthesia during CMR, history of aortic stenosis, aortic coarctation or previous aortic root or valve replacement, and inadequate images for measurements of strain and stiffness. Patient demographic information, body surface area, clinical history, and standard CMR measurements were recorded. The use of cardiac medication was defined as β blockers, angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, and calcium channel blockers. Aortic area was measured at the aortic annulus, sinuses of Valsalva, sinotubular junction, and the ascending aorta through double-oblique images orthogonal to the long axis of the vessel.
CMR was performed using a commercially available 1.5-T scanner (Intera Achieva; Philips, Best, the Netherlands). Cine images for ventricular measurement were obtained in the short-axis plane using a breath-hold, electrocardiographically gated, segmented k-space, steady-state free precession sequence, with slice thickness of 6 to 8 mm, in-plane spatial resolution of 1.5 to 1.8 mm, and 30 phases obtained through the cardiac cycle. The left and right ventricular end-diastolic and end-systolic volumes were measured using a commercially available software (ViewForum; Philips, Best, the Netherlands). Aortic strain was chosen to evaluate elasticity because blood pressure measurements during the CMR examination were not available to calculate distensibility. Aortic strain was defined by the formula: (Amax−Amin)/(Amin)×100
( A max – A min ) / ( A min ) × 100
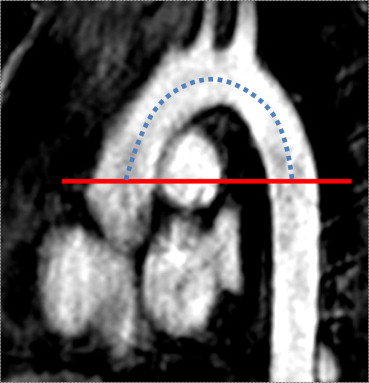
, where A max and A min are the maximum and minimum luminal areas (mm 2 ), respectively, of the aorta between the sinotubular junction and the level of the right pulmonary artery, as measured from magnitude images of electrocardiographically gated, velocity-encoded, phase contrast images, performed free breathing with multiple signal acquisitions. Aortic and pulmonary insufficiencies were calculated by direct measurement of retrograde flow compared with forward flow in phase contrast imaging. PWV was used as a measure of aortic stiffness and defined as the distance of the thoracic aortic arch divided by the time for the pulse wave foot to travel from the ascending to the descending aorta ( Figure 1 ). The distance from ascending to descending aorta was determined by crossreferencing the plane of phase contrast images to the long axis of the aortic arch from a gadolinium-enhanced, 3-dimensional magnetic resonance angiogram of the chest, after the administration of 0.2 mmol/kg of contrast: gadopentetate dimeglumine (Magnevist; Bayer Pharmaceuticals, Leverkusen, Germany) or gadoteridol (ProHance; Bracco Diagnostics, Princeton, New Jersey) and measuring the distance through the aortic arch in the center of the vessel. The time between the pulse wave foot at the ascending and descending aorta was measured manually from phase contrast image data.
All statistical analyses were performed using SAS, version 9.3 (SAS Institute Inc, Cary, North Carolina). Data are presented as mean ± SD or median (interquartile range [IQR] or range) for continuous variables and frequency (percentage) for categorical variables, as appropriate for the data distribution. Univariate associations of patient and clinical characteristics with aortic strain and stiffness were evaluated using Pearson or Spearman correlation coefficient for continuous variables and t test or Wilcoxon rank-sum test for dichotomous variables. Variables found to be significantly associated with PWV in the univariate analysis (p <0.05) were investigated further by building multivariate linear regression models to determine independent relations of patient and clinical characteristics with aortic stiffness. The log of the percent change in age at repair was used because of distribution of data and made no difference in significance during statistical analysis. Model fit was evaluated by adjusted R 2 and mean square error. p Values <0.05 were considered statistically significant.
Results
Of 227 patients with repaired TOF who had CMR performed during the study period, 124 patients met inclusion criteria and were analyzed ( Figure 2 ). Patient characteristics and CMR measurements are listed in Tables 1 and 2 , respectively. Hypertension, smoking, and diabetes occurred rarely in our patients and were not considered in the analysis. Left and right ventricular volumes and ejection fraction were similar to other published cohorts with TOF.




