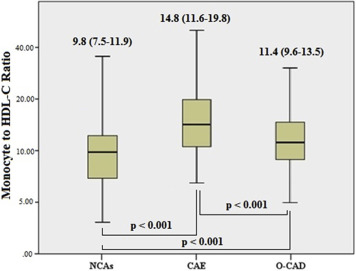
The aim of this study was to investigate an easily available inflammatory and oxidative stress marker and monocyte to high-density lipoprotein cholesterol ratio (MHR) in patients with coronary artery ectasia (CAE). The study population included 405 patients of which 135 patients had isolated CAE, 135 patients had obstructive coronary artery disease (CAD), and 135 patients had normal coronary angiograms (NCAs). The severity of isolated CAE was determined according to the Markis classification. The MHR was significantly greater in patients with isolated CAE than those with obstructive CAD and NCAs: 14.8 (11.6 to 19.8), 11.4 (9.6 to 13.5), 9.8 (7.5 to 11.9), respectively. Linear regression analyses showed that MHR and C-reactive protein were significantly related with the severity of isolated CAE. In conclusion, the MHR is significantly greater in patients with CAE compared to controls with obstructive CAD and NCAs, and MHR is associated with the severity of CAE.
Macrophages and monocytes are the most important cell types for secretion of proinflammatory cytokines at the site of inflammation. In addition, high-density lipoprotein cholesterol (HDL-C) has been shown to defend endothelial cells against the unfavorable effects of low-density lipoprotein cholesterol (LDL-C) and to prohibit oxidation of LDL molecules. Therefore, it was believed that HDL-C exhibits anti-inflammatory actions. Recently, Kanbay et al reported monocyte to high-density lipoprotein cholesterol ratio (MHR) as a new cardiovascular prognostic marker in chronic kidney disease. Canpolat et al also investigated that MHR is an independent predictor of atrial fibrillation recurrence after cryoballoon-based catheter ablation and significantly and independently associated with the presence of slow coronary flow. To the best of our knowledge, no studies up to date investigated MHR in patients with isolated coronary artery ectasia (CAE) and compared the results with obstructive coronary artery disease (CAD) and normal coronary angiograms (NCAs). Because inflammation is the main constituent of CAE and increased monocyte count and decreased HDL-C levels were shown to be associated to inflammation, we hypothesized that MHR may be related with the presence and severity of isolated CAE.
Methods
In this study, we included 405 patients after gaining approval for the study protocol by local ethics committee of our hospital, and we retrospectively analyzed the electronic patient record system of our hospital. Of these, 135 patients with isolated CAE constituted the first group. During this period, initial 135 consecutive patients who had obstructive CAD without CAE comprised the second group, and 135 consecutive patients with NCAs comprised the last group.
Arterial hypertension was considered in patients with repeated blood pressure measurements of >140/90 mm Hg or current use of antihypertensive drugs. Diabetes mellitus was defined as fasting plasma glucose levels ≥126 mg/dl on multiple measurements or current use of antidiabetic medications. Hypercholesterolemia was considered as total serum cholesterol of >200 mg/dl or the use of lipid-lowering medication. Family history of CAD was considered in case of history of CAD or sudden cardiac death in a first-degree relative before the age of 55 years for men and 65 years for women.
Patients with an acute coronary syndrome defined as ST-elevation myocardial infarction (STEMI) and non-STEMI were excluded from the study. We also excluded patients with left ventricular systolic dysfunction (left ventricular ejection fraction [LVEF] <40%), malignancy, and liver, kidney, or other acute or chronic inflammatory diseases or the ones that had undergone percutaneous coronary intervention and coronary artery bypass grafting previously.
Coronary angiography was performed for the investigation of ischemic heart disease based on clinical indications (abnormal stress test results such as dobutamine stress echo, positive treadmill test, and myocardial perfusion scintigraphy or typical chest pain). All patients were clinically stable. The standard Judkins technique and 6Fr catheters (Expo; Boston Scientific Corporation, Massachusetts) were used to perform baseline angiography through the femoral artery, and Siemens Axiom Sensis XP device was used. The vessel diameter was calculated quantitatively in case of conflicts about CAE. The CAEs were defined based on the criteria used in the Coronary Artery Surgery Study. According to the angiographic definition used in that study, a vessel was considered to be ectasic when its diameter was ≥1.5 times that of the adjacent normal segment in segmental ectasia. When there was no identifiable adjacent normal segment, the mean diameter of the corresponding coronary segment in the control group served as the normal value. Isolated CAE was defined as CAE without significant coronary artery stenosis. The severity of isolated CAE was determined according to the Markis classification. In decreasing order of severity, diffuse ectasia of 2 or 3 vessels was classified as type 1, diffuse disease in 1 vessel and localized disease in another vessel as type 2, diffuse ectasia of only 1 vessel as type 3, and localized segmental ectasia as type 4. Obstructive CAD was described as stenosis of >50% of the diameter at 1 or more major epicardial artery and which has no coronary ectasia.
Peripheral venous blood samples of the patients were obtained on their admission to the inpatient ward. An automated blood cell counter (Beckman Coulter analyzer, California) was used for measuring complete blood count parameters. Blood biochemistry parameters levels that were measured were creatinine, total cholesterol, HDL-C, LDL-C, and total bilirubin. High-sensitivity C-reactive protein (hsCRP) measurement was done using an automatized analyzer (Beckman Coulter analyzer) using nephelometric measurement before the coronary angiography. Transthoracic echocardiography was performed in all patients, and LVEF was calculated using the Simpson method.
SPSS 22.0 statistical package program (SPSS Inc., Chicago, Illinois) was used to perform all data analyses. The Kolmogorov–Smirnov test was used to analyze the distribution pattern. Normally distributed numerical variables were presented as mean ± standard deviation, and the ones not normally distributed were presented as median and interquartile range. Categorical variables were presented as number and percentage (%). The Spearman rank test was performed to define the correlation between MHR and hsCRP. Logistic regression analysis was performed to find independent predictors of presence of isolated CAE. Variables that had an unadjusted p value of <0.10 in logistic regression analysis were identified as potential risk markers and then included in the full model. We eliminated potential risk markers with likelihood ratio tests with reduced model using multivariate logistic regression analyses. A p value of <0.05 was considered statistically significant with a confidence interval of 95%. Receiver operating characteristic (ROC) curve analysis was performed to detect the cut-off value of the MHR in predicting CAE.
Results
A total of 405 patients were included into the study. Clinical and angiographic characteristics and biochemical and hematologic measurements of the study population are presented in Tables 1 and 2 , respectively. There are no differences among 3 groups for LVEF, smoker, family history of CAD, hypertension, hypercholesterolemia, and values of hemoglobin, total bilirubin, total cholesterol, creatinine, LDL-C, and HDL-C. The patients with obstructive CAD and isolated CAE were significantly older and had higher prevalence of male gender and history of diabetes mellitus. The patients with obstructive CAD and isolated CAE have significantly greater white blood cells, platelets, monocytes, neutrophil counts, hsCRP, and MHR values. In contrast, these groups have significantly lower lymphocyte counts. As shown in Figure 1 , the patients with isolated CAE had significantly greater MHR values compared to the others. In univariate logistic regression analyses, age, male gender, diabetes mellitus, white blood cell and neutrophil counts, hsCRP, and MHR were significantly associated with isolated CAE. When these 7 parameters were included in a multivariate logistic regression analyses, MHR and hsCRP were independently and significantly associated with isolated CAE ( Table 3 ). In addition, there was a positive correlation between hsCRP and MHR levels ( r = 0.435, p <0.001, Figure 2 ).
| Variable | Coronary Arteries | p Value | ||
|---|---|---|---|---|
| Ectatic (n=135) | Obstructive (n=135) | Normal (n=135) | ||
| Men | 64 (47.4%) | 69 (51.1%) | 56 (41.4%) | 0.007 ∗ |
| Age (Years) | 65 ± 11 | 64 ± 14 | 58 ±12 | 0.001 ∗ |
| Diabetes mellitus | 28 (20.7%) | 41 (30.3%) | 23 (17.0%) | <0.001 ∗ |
| Smoker | 26 (19.2%) | 28 (20.7%) | 25 (18.5%) | 0.256 |
| Hypertension | 65 (48.1%) | 67 (49.6%) | 62 (45.9%) | 0.185 |
| Hypercholesterolemia | 58 (42.9%) | 55 (40.7%) | 46 (37.1%) | 0.155 |
| Family history of coronary artery disease | 30 (22.2%) | 28 (20.7%) | 28 (20.7%) | 0.455 |
| Left ventricular ejection fraction | 60 ± 10 | 59 ± 11 | 60 ± 10 | 0.768 |
| Prior Medication | ||||
| Beta-blocker | 55 (40.7%) | 56 (41.5%) | 51 (37.8%) | 0.373 |
| Angiotensin converting enzyme inhibitor or Angiotensin receptor blocker | 53 (39.2%) | 56 (41.4%) | 52 (38.5%) | 0.115 |
| Statin | 41 (29.1%) | 46 (32.7%) | 30 (27.2%) | 0.245 |
| Markis Classification | ||||
| Type 1 | 43 (31.9%) | |||
| Type 2 | 24 (17.7%) | |||
| Type 3 | 19 (14.1%) | |||
| Type 4 | 51 (37.7%) | |||
| Ectatic Coronary Artery | ||||
| Left anterior descending | 84 (62.2%) | |||
| Left circumflex | 64 (47.4%) | |||
| Right | 106 (78.5%) | |||
Variable | Coronary Arteries | p Value | ||
|---|---|---|---|---|
| Ectatic (n=135) | Obstructive (n=135) | Normal (n=135) | ||
| White blood cell (10 9 /μL) | 8355 ± 3970 | 8375 ± 3445 | 7290 ± 3760 | 0.045 ∗ |
| Neutrophil (10 9 /μL) | 6560 ± 3810 | 6280 ± 4560 | 5270 ± 3485 | 0.006 ∗ |
| Lymphocyte (10 9 /μL) | 2105 ± 1100 | 1980 ± 1250 | 2200 ± 1180 | 0.030 ∗ |
| Monocyte (10 9 /μL) | 632 ± 336 | 585 ± 310 | 525 ± 345 | <0.001 ∗ |
| Platelet (10 9 /μL) | 257500 ± 65050 | 244500 ± 63200 | 231700 ± 58500 | <0.001 ∗ |
| High sensitivity C- reactive protein (mg/L) | 0.72 ± 0.16 | 0.53 ± 0.13 | 0.41 ± 0.10 | <0.001 ∗ |
| Total cholesterol (mg/dL) | 175 ± 59 | 179±58 | 180 ± 57 | 0.453 |
| Low density lipoprotein cholesterol (mg/dL) | 111 ± 37 | 118 ± 36 | 114 ± 39 | 0.465 |
| High density lipoprotein cholesterol (mg/dL) | 39 ± 14 | 41 ± 12 | 42 ± 11 | 0.140 |
| Creatinine (mg/dL) | 1.1 ± 0.4 | 1.1 ± 0.3 | 1.1 ± 0.3 | 0.655 |
| Total bilirubin (mg/dL) | 0.65 ± 0.4 | 0.58 ± 0.3 | 0.61 ± 0.3 | 0.773 |
| Monocyte to high density lipoprotein cholesterol ratio | 14.8 (11.6-19.8) | 11.4 (9.6-13.5) | 9.8 (7.5-11.9) | <0.001 ∗ |