CHAPTER 2 Radiologic Imaging of Thoracic Abnormalities
MEDIASTINAL ABNORMALITIES
Mediastinal abnormalities have a variety of causes, including congenital malformations, infections, trauma, and neoplasms. Clinical history and prior radiographs are often sufficient to determine the etiology and the necessity for further evaluation. In the absence of prior imaging studies, chest radiographs, CT, or MRI are most commonly used to establish a diagnosis, or to provide a differential diagnosis.1
Aortic Dissection
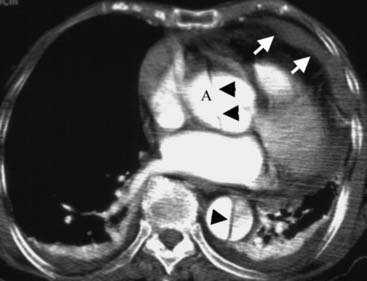
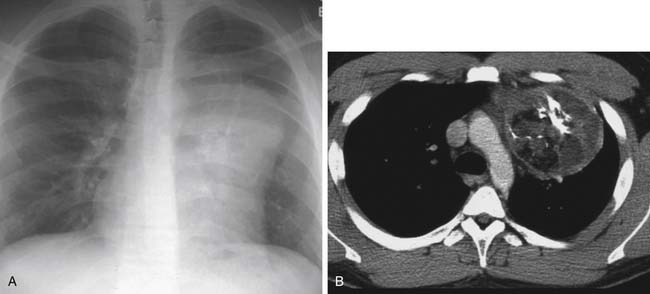
MDCT with intravenous contrast is the modality of choice when an aortic dissection is suspected. The sensitivity and specificity approaches 100%, with an accuracy that is superior to that of angiography.2,3 MDCT can determine the type and extent of the dissection for management decisions. The primary diagnostic finding on CT is an intimal flap separating the true from the false lumen. Type A dissections involve the ascending aorta and originate just above the aortic valve plane, and they are usually considered for surgical repair (Fig. 2-1). Type B dissections, however, originate just below the level of the ligamentum arteriosum, and they spiral down the descending aorta. These patients are often hypertensive and are managed medically.
More recently, if a patient presents with chest pain and the diagnosis is uncertain, the rapid technologic advancement in CT scanners has allowed the use of 64-slice MDCT to image the entire thoracic volume with a high-resolution retrospective electrocardiography (ECG)-gating technique, evaluating not only the aorta but also the coronary and pulmonary arteries in a single study.4
Trauma
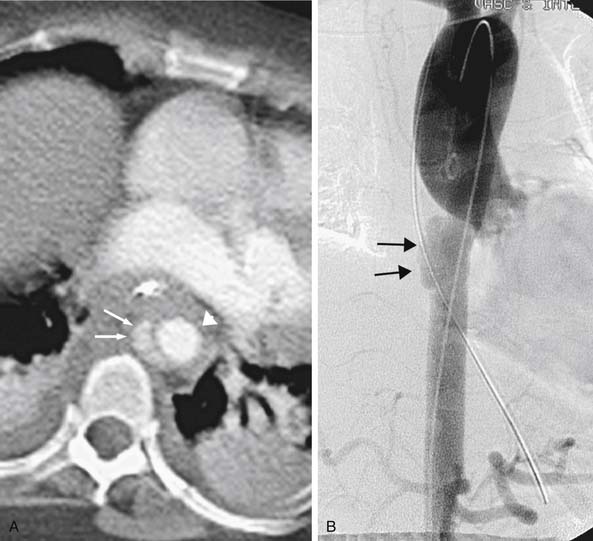
Patients with thoracic trauma usually require imaging evaluation, and the type of study depends on the mechanism of injury and the structures potentially involved. From a radiographic perspective, the chest radiograph is typically the first study performed and often dictates whether additional imaging is warranted. The radiographic findings suggestive of traumatic aortic injury (TAI) are an indistinct aortic arch or descending aorta, a left apical cap, tracheal displacement to the right, displacement of the nasogastric tube to the right of the T4 spinous process, mediastinal widening, and inferior displacement of the left main-stem bronchus (Fig. 2-2).5–7 Less specific findings include a left pleural effusion and widening of the paravertebral stripe.8,9 These features, however, are only suggestive, not indicative, of an aortic injury. In contradistinction, the negative predictive value of a normal chest radiograph for an aortic injury is 94% to 96%.9,10 If there is a chest radiographic abnormality, MDCT is typically the next study of choice. MDCT allows the rapid acquisition of thin slices (1 to 3 mm) and three-dimensional (3D) reconstruction and is now the primary imaging method for the diagnosis of TAI if the chest radiograph is abnormal. The sensitivity for this technique is 100%, and the specificity ranges from 83% to 99.7% (Fig. 2-3).11–15 The absence of a periaortic abnormality and a normal-appearing aorta on MDCT has a negative predictive value of 100%.14,15 Additional thoracic injuries can be identified at the same time, thus limiting investigation of the trauma patient to one study.12 Indirect signs of TAI, most notably a periaortic hematoma, are found in 91% of patients with surgically proven TAI.12 If this finding is present, further evaluation with an aortogram may be required. Aortography is safe and accurate, with a negative predictive value for TAI approaching 100%. Direct signs for TAI include a linear intraluminal filling defect, pseudoaneurysm formation, an abrupt caliber change, and active contrast extravasation.12,16,17
Additional thoracic abnormalities are found in only 7% of patients who do not have an aortic transection on MDCT. Such abnormalities are usually a combination of pneumothoraces, multiple rib fractures, and pulmonary contusions.18
Trauma: Airways and Esophagus
Tracheal and esophageal injuries are uncommon but are typically found after a motor vehicle accident or another penetrating trauma (Fig. 2-4). Many of these injuries are not recognized initially because of subtle or nonspecific clinical and radiologic findings. Delayed or missed diagnosis can result in death or severe complications such as ventilatory failure, mediastinitis, sepsis, airway stenosis, bronchiectasis, recurrent pulmonary infections, and permanent pulmonary function impairment.19
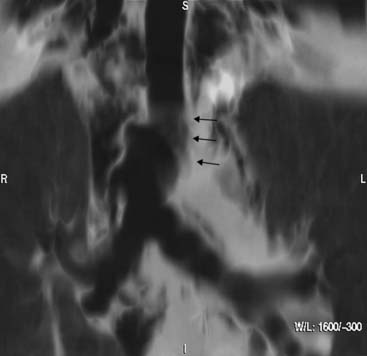
Chest radiographic findings of tracheobronchial and esophageal injury are nonspecific and can include pneumomediastinum, pneumothorax, and progressive subcutaneous emphysema.19–21 MDCT is the imaging modality of choice for visualization of the airways. Patients with tracheal rupture characteristically have an abnormal air collection in the thorax, and air can occasionally be demonstrated in the soft tissues of the neck.22 Success in visualizing the tracheal injury ranges from 71% to 94%, and multiplanar reconstructions can be useful in localizing and defining the extent of injury.20,22 MDCT also provides information about the esophagus, although if pneumomediastinum, with or without mediastinal fluid, is found on chest radiographs or CT after trauma, a barium swallow or endoscopy is usually warranted to exclude an esophageal tear.
Evaluation of Airways: Nontrauma
Focal or diffuse lesions of the central airways are produced by a variety of diseases, including infection, malignancy, trauma, aspiration, collagen vascular disease, and idiopathic entities such as sarcoidosis or amyloidosis. Even though patients may present with significant symptoms, airway abnormalities are frequently not apparent or are overlooked on the chest radiograph. If there is a clinical suspicion of a tracheobronchial abnormality, further evaluation by CT is warranted.23,24 MDCT using thin slices (1 to 3 mm) is preferred, as it produces excellent axial and multiplanar images of complex tracheobronchial anatomy, depicting even web-like stenosis that can easily be missed or underestimated with thicker sections (Fig. 2-5).24,25
Mediastinal Tumors
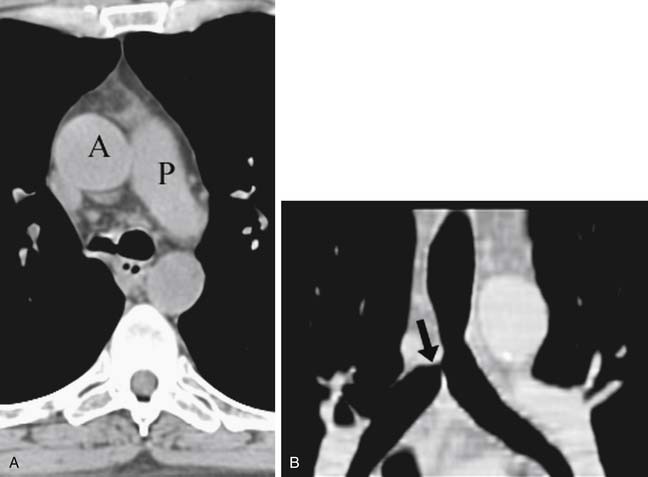
Tumors that occur primarily in the anterior mediastinum include hemangiomas, lymphatic malformations, thymic lesions (cysts, thymolipoma, thymoma, thymic carcinoma), parathyroid adenomas, germ cell tumors, and lymphoma (Fig. 2-6). CT and MRI are particularly useful for showing local soft tissue and vascular invasion of thymomas, local invasion, and early dissemination to regional lymph nodes of thymic carcinomas and, because of the varying composition of soft tissue, fat, calcium, and hemorrhage in teratomas, can occasionally differentiate these tumors from thymomas and lymphomas.26–30
Tumors that occur primarily in the middle mediastinum are foregut malformations, pericardial cysts, and neoplasms arising from the esophagus and trachea. Bronchogenic cysts are the most common mediastinal foregut cysts and are typically located in the subcarinal or right paratracheal region. They appear on CT as a round or spherical masses of water attenuation, although many have increased attenuation from proteinaceous debris or blood.31–33 Esophageal tumors can manifest as middle mediastinal masses, although esophageal carcinoma more frequently manifests as diffuse thickening of the esophagus. Endoscopy and endoscopic-directed ultrasound biopsy are usually used to evaluate locoregional extent and nodal metastases. CT is useful in showing the extent of involvement of adjacent structures such as the airways, aorta, pericardium, and spine, and in revealing distant nodal metastases (celiac, gastrohepatic ligament).
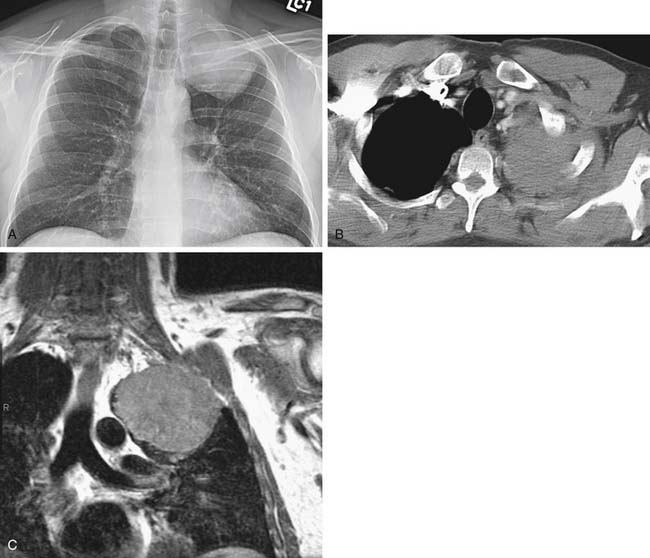
Tumors that occur primarily in the posterior compartment are neurogenic tumors. In fact, 20% of all adult and 35% of all pediatric mediastinal neoplasms are neurogenic tumors, and most are located in the posterior mediastinum.34,35 Neurogenic tumors are classified as tumors of peripheral nerves (neurofibromas, schwannomas, malignant tumors of nerve sheath origin) or sympathetic ganglia (ganglioneuromas, ganglioneuroblastomas, neuroblastomas) and are optimally assessed by MRI. MRI is the preferred modality for evaluating neurogenic tumors, as it can simultaneously assess (1) intraspinal extension, (2) spinal cord abnormalities, (3) longitudinal extent of tumor, and (4) extradural extension.
LUNG ABNORMALITIES
Thoracic imaging is essential in the workup of pulmonary abnormalities, including lung nodules and focal opacities, intrathoracic malignancies, diffuse interstitial lung disease, and infection. Low-dose CT (LDCT) has also been proposed as a screening tool for lung cancer; however, no data have yet shown that this approach reduces lung cancer mortality.36,37 The results of the National Lung Screening Trial (NLST), a randomized study comparing the effectiveness of LDCT to chest radiography in more than 50,000 participants, will, it is hoped, clarify the role of thoracic imaging in screening.
Solitary Pulmonary Opacities
Solitary pulmonary opacities are a common radiologic finding and are usually benign, but because of concern about lung cancer, further evaluation is often suggested. The goal is to differentiate malignant and benign lesions so that those patients who require surgery are correctly identified. Although morphologic features may suggest whether a nodule is benign or malignant, there is considerable overlap, and at least 20% of malignant nodules have a benign appearance.38–40 Specific patterns of calcification and stability in size for 2 years have historically been the only reliable findings useful in determining benignity. More recently, the ability to distinguish between benign and malignant opacities has improved with assessment of perfusion using contrast-enhanced CT41 and assessment of metabolism using PET imaging with fluorodeoxyglucose labeled with radioactive fluoride (18F) (FDG).
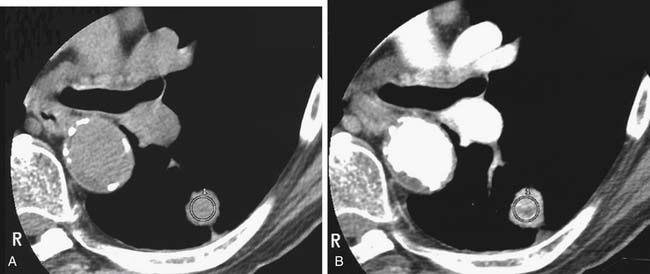
Contrast-enhanced CT can be used to differentiate benign and malignant nodules because the intensity of enhancement is directly related to the vascularity of the nodule and to the likelihood of malignancy.42,43 Typically, malignant nodules enhance more than 20 Hounsfield units (HU), whereas benign nodules enhance less than 15 HU (Fig. 2-7).44 Nodule-enhancement CT has a very high negative predictive value but poor specificity. FDG-PET has a lower sensitivity but a higher specificity and may be helpful to further evaluate a patient who has a nodule that enhances 20 HU or more on CT.45
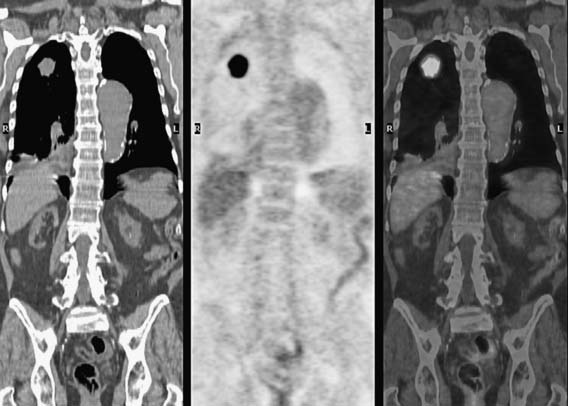
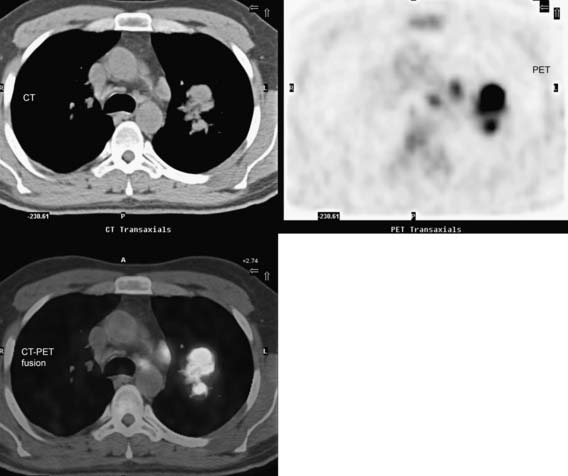
PET imaging also allows differentiation of malignant and benign nodules that are indeterminate after conventional imaging (Fig. 2-8). A meta-analysis of 40 studies on the accuracy of FDG-PET reports a sensitivity of 97% and a specificity of 78% when used in the evaluation of 10-mm or larger nodules.46 However, a recent prospective integrated PET-CT evaluation of 585 patients (496 malignant, 89 benign nodules) showed that although a high standardized uptake value (SUV) (>4.1) was associated with a 96% likelihood of malignancy, the likelihood of malignancy was still 25% when the SUV was 0 to 2.5.47 It has been shown that the maximal SUVs on integrated FDG-PET/CT are useful in differentiating benign and malignant pulmonary nodules.47 Furthermore, in malignant nodules that are smaller than 1 cm in diameter or have ground-glass or partially solid morphology, FDG uptake is variable and unreliable in differentiating benign from malignant nodular opacities.48
The Fleischner Society has guidelines for the management of small, indeterminate pulmonary nodules detected incidentally on routine chest CT.49
Staging Lung Cancer
Staging, the assessment of the anatomic extent of non–small cell lung cancer (NSCLC), usually determines treatment and prognosis. Clinical staging typically includes CT and, more recently, PET-CT. The current tumor (T), node (N), and metastasis (M) staging system is being modified, and the greater emphasis on the importance of the size of the primary tumor will require CT for accurate determination.50,51 CT is also usually used to define chest wall or mediastinal invasion but is inaccurate in differentiating between anatomic contiguity and subtle invasion.52–56 Although MRI has better soft-tissue contrast resolution than CT, the two modalities have the same limitations for assessing local disease (Fig. 2-9).52,54,57,58
The presence of nodal metastases and their locations are important for determining management and prognosis (Fig. 2-10).50,59 CT is most commonly used to assess the size of nodes (>10 cm in short-axis diameter), and size is the only criterion used to suggest nodal metastases.60 PET imaging improves the accuracy of nodal staging. In a meta-analysis of 17 studies comprising 833 patients, the overall sensitivity of PET for detecting nodal metastases was 83% and the specificity was 92%, whereas the sensitivity and specificity of chest CT were 59% and 78%, respectively.61 Interestingly, in the presence of enlarged lymph nodes, PET and PET-CT become less specific and less accurate but more sensitive in detecting nodal metastases.62,63
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree