We sought to compare operator radiation exposure during procedures using right femoral access (RFA), right radial access (RRA), and left radial access (LRA) during coronary angiography (CA) and percutaneous coronary intervention (PCI). Because of an increased incidence of long-term malignancy in interventional cardiologists, operator radiation exposure is of rising concern. This prospective study included all consecutive patients who underwent elective or emergency CA ± PCI from September 2014 to March 2015. The primary end point was operator radiation exposure, quantified as the ratio of operator cumulative dose (CD) and patient radiation reported as dose-area product (DAP) (CD/DAP). Secondary end points included CD, DAP, and fluoroscopy time (FT). Overall 830 procedures (457 CA [55%] and 373 PCI [45%]) were performed, 455 (55%) through RFA, 272 (33%) through RRA, and 103 (12%) through LRA. The CD/DAP was lower in RFA (0.09 μSv/Gycm 2 [0.02 to 0.20]) compared with RRA (0.47 μSv/Gycm 2 [0.25 to 0.75], p <0.001). The LRA showed lower CD/DAP compared with RRA (p <0.001). CD was significantly lower in RFA (3 μSv [1 to 7]) compared with RRA (12 μSv [6 to 29], p <0.001). The LRA showed lower CD compared with RRA (p <0.001). There were no significant differences in DAP among the 3 access sites. FT was similar for the 3 groups (RFA 7 ± 7, RRA 5 ± 5, LRA 6 ± 5 minutes, RFA vs RRA: p = 1, RFA vs LRA: p = 0.16, RRA vs LRA: p = 0.52). In conclusion, the use of RFA during CA ± PCI is associated with significantly lower operator radiation exposure compared with RRA. LRA is associated with significantly lower operator radiation exposure compared with RRA.
Because of a presumably increased stochastic risk of cancer induction among interventional cardiologists, especially neoplasms of the unprotected brain, nasopharyngeal tract, and upper extremities, operator radiation exposure during coronary angiography (CA) and/or percutaneous coronary intervention (PCI) is of rising concern. Therefore, we undertook a comparison of operator radiation exposure during right femoral access (RFA), left radial access (LRA), and right radial access (RRA) during CA and CA followed by ad hoc PCI in a real-world population.
Methods
From September 2014 to March 2015 at the University and Hospital Fribourg, all consecutive procedures of elective or emergency CA and CA followed by ad hoc PCI were prospectively considered for operator radiation exposure measurements. Procedures were performed by 5 senior interventional cardiologists with significant experience (>3,000 PCI each) in both femoral and radial access routes. Selection of the percutaneous access site was left to the discretion of the operator. Crossover access site procedures were excluded. This study was part of the Catheterization Registry Fribourg (CardioFR), which was approved by the Ethics Committee of Canton Vaud (protocol no: 339/14).
The primary end point of the study was operator radiation exposure, expressed as the cumulative equivalent dose (in μSv) over the lead apron at chest level, normalized for the patient radiation exposure (dose-area product [DAP] in Gycm 2 ). Secondary end points included cumulative dose (CD), DAP, and fluoroscopy time (FT).
Procedures were performed on a digital single-plane cineangiography unit (Allura FD10; Philips Medical Systems, Hamburg, Germany) with an undertable x-ray tube MRC20025 with a magnification factor leading to a field of view of 21 cm and an acquisition frequency of 15 frames/s. All procedures were performed with respect to current guidelines using either 5Fr or 6Fr hydrophilic sheaths. Conventional diagnostic and guiding catheters were used.
The femoral access was achieved, under local anesthesia with 2% rapidocain, through the anterior wall puncture of the artery; 5Fr or 6Fr Terumo (Pinnacle; Terumo Medical, Tokyo, Japan) introducer was placed in the femoral artery. CA and PCI were performed according to standard practice using catheter and drugs left to the discretion of the operator. Hemostasis was achieved using closure devices (Femoseal; St. Jude Medical, St. Paul, Minnesota) or external mechanical compression (Femostop; St. Jude Medical).
After sterile preparation and anesthesia with 2% rapidocain infiltration, radial artery was punctured with a 20-gauge needle. A 0.021 Teflon-sheathed short guidewire was inserted in the needle. A 3.2-section BD Venflon was then inserted in the artery. A Terumo (Pinnacle; Terumo Medical) 0.021 hydrophilic guidewire was advanced through the radial and brachial artery. A 5Fr introducer was then inserted in the radial artery. Vasodilator cocktail consisting of verapamil 3 mg and enoxaparin 3,400 units was administered after sheath insertion. Specific catheters were used for CA and PCI. Exchange to a 6Fr sheath was possible when technically necessary. At the end of the procedure, the sheath was removed and an inflatable pressure band placed to the access site. All radial accesses were performed at the right side of the patient.
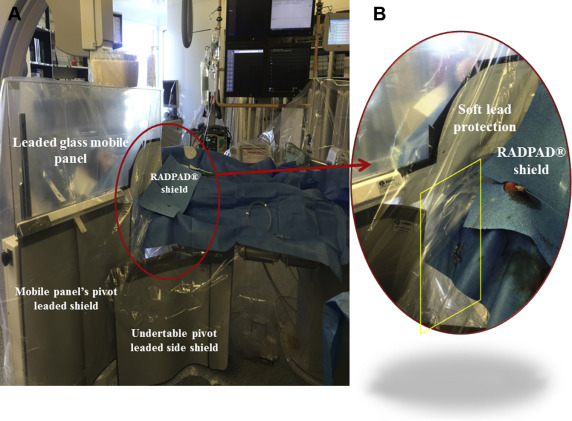
Operator protection was ensured with the same equipment for all procedures. A leaded glass mobile panel with a patient contour cutout (0.5 lead equivalent; MAVIG, Munich, Germany) was positioned at the left side of the operator. An undertable pivot-leaded side shield (0.5-mm lead equivalent) was mounted to the side of the table. An additional soft lead shield was adjusted in the contour cut of the leaded glass mobile panel to minimize radiation exposure. The 37 × 42 cm upper-shield flap (RADPAD, Worldwide Innovations & Technologies, Inc, Kansas City, USA) was placed over the access site in each procedure to reduce scatter radiation ( Figure 1 ). Additional radiation protection materials were standardized for all operators and included a lead apron, thyroid lead collar, and leaded glasses. All procedures were performed from the patients’ anatomical right side.
Operator radiation was measured using individual electronic dosimeters (DoseAware; Philips Healthcare, Best, The Netherlands) positioned on the sternum, outside the lead apron. The dosimeters are silicon-based semiconductor detectors with a dose-response between 1 μSv and 10 Sv, in steps of 1 μSv (calibrated in ambient equivalent dose Hp(10)) and a temporal resolution of 1 second. The following parameters were recorded for each procedure: (1) operator CD through the use of dedicated readout software (DoseView), measured by the individual dosimeters; (2) FT; (3) number of cine angiograms (NC); and (4) the DAP-normalized CD defined as the dose (μSv) received by the operator with each Gycm 2 applied to the patient (known as the exposure factor) has been advocated and applied to our study as it isolates differences in patient radiation among the 3 vascular access sites. Patient radiation dose was expressed as DAP. Furthermore, radiation exposure of the assistant nurse, the first nurse on the operator’s right side, was assessed using similar dosimeters, in a subgroup of consecutive procedures, with the aim to compare radiation exposure of the operator versus assistant nurse.
All statistical analyses were performed using dedicated software (Stata, version 13; StataCorp LP, College Station, Texas) at a 2-tailed significance level of alpha <0.05. Baseline patient and procedural characteristics, and variables assessing radiation exposure of the operator, were compared among the 3 vascular access sites. Categorical variables are reported as counts and percentages; continuous variables are reported as mean and SD or as median with 25% to 75% interquartile range according to their distribution. Normality was assessed by visual inspection of histograms, the computation of Q-Q plots and the Shapiro-Wilk test. Categorical variables were compared using the chi-square or Fisher’s exact test as appropriate. Continuous variables were analyzed using the 1-way ANOVA or the Wilcoxon rank-sum test according to their distribution. To account for differences of the individual operators on radiation exposure according to access site, we computed a generalized linear model including the individual operators as potential confounders of the overall treatment effect. To account for multiple comparisons, p values are Bonferroni adjusted, that is, multiplied by the number of comparisons. Comparison of radiation exposure between the operator and the first assistant was assessed using the paired student’s t test or the signed-rank Wilcoxon test according to distribution.
Results
During September 2014 and March 2015, 849 consecutive procedures for elective or emergency CA and CA followed by ad hoc PCI were performed in our catheterization laboratory with a dedicated dosimeter for radiation evaluation. Nineteen procedures (1.8%) were excluded because of a crossover in access sites. No patient was excluded because of lesion or procedural complexity. Finally, 830 consecutive procedures were included in the trial, 457 CA alone (55%) and 373 CA followed by ad hoc PCI (45%). With regard to vascular site, 455 procedures (55%) were carried out using the RFA, 103 (12%) using the LRA, and 272 (33%) using the RRA. Baseline patient characteristics were generally well balanced and depicted in Table 1 . Analysis of procedural characteristics as listed in Table 1 revealed no difference in FT among the groups and showed a significantly greater NC in RFA compared with LRA and RRA group and in RRA compared with the LRA group, probably reflecting higher procedural complexity.
| RFA (N=455) | LRA (N=103) | RRA (N=272) | p-values | |||
|---|---|---|---|---|---|---|
| RFA vs. LRA | RFA vs. RRA | LRA vs. RRA | ||||
| Patients | ||||||
| Age (years±SD) | 68±12 | 69±10 | 65±12 | 1.00 | 0.02 | 0.05 |
| Male | 310 (68%) | 71 (69%) | 181 (67%) | 1.00 | 1.00 | 1.00 |
| Weight (kg±SD) | 80±16 | 80±18 | 81±16 | 1.00 | 1.00 | 1.00 |
| Height (m±SD) | 1.70±0.09 | 1.70±0.09 | 1.70±0.09 | 1.00 | 1.00 | 1.00 |
| BMI (kg/m 2 ±SD) | 27±5 | 27±5 | 28±5 | 1.00 | 1.00 | 1.00 |
| Procedure | ||||||
| CA | 216 (47%) | 65 (63%) | 176 (65%) | 0.01 | <0.01 | 1.00 |
| CA followed by ad hoc PCI | 239 (53%) | 38 (37%) | 96 (35%) | 0.01 | <0.01 | 1.00 |
| Procedural time (min±SD) | 20±19 | 15±11 | 18±12 | 0.05 | 1.00 | 0.08 |
| Fluroscopy time (min±SD) | 7±7 | 5±5 | 6±5 | 0.16 | 1.00 | 0.52 |
| Nb of cine-angiograms (n±SD) | 954±520 | 659±351 | 727±300 | <0.001 | <0.01 | <0.001 |
The radiation exposure of the assistant nurse standing at the operator’s right side was also assessed in a subgroup of first 293 consecutive procedures, 152 CA alone (52%) and 141 CA followed by ad hoc PCI (48%), 164 (56%) through RFA, 49 (17%) through LRA, and 80 (27%) through RRA.
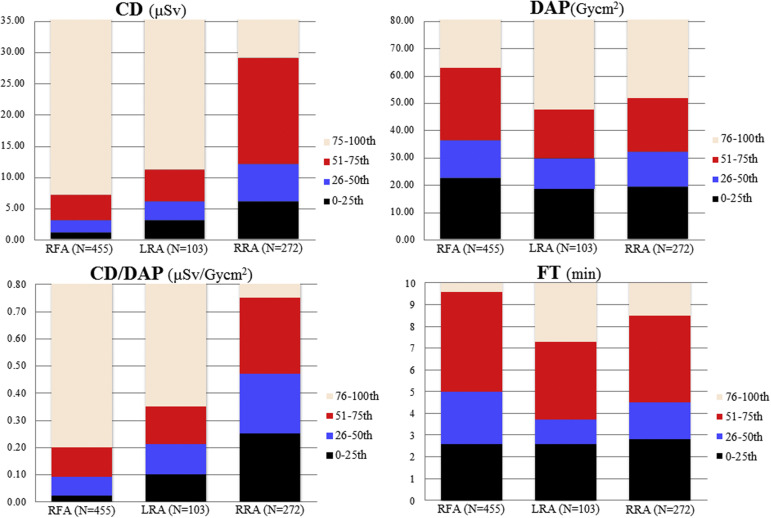
Table 2 and Figure 2 list patient and operator radiation exposure. Adjusted CD was significantly lower in RFA compared with RRA but not to LRA. CD was lower for procedures using LRA than RRA. Patient radiation dose expressed by DAP did not significantly vary among the 3 access sites. Operator radiation dose reported as the DAP-normalized CD was significantly higher in the RRA compared with the RFA and LRA group for all procedures, procedures with CA alone, and procedures with CA followed by ad hoc PCI. There were no significant differences between the RFA and the LRA for any kind of procedure. Table 3 indicates DAP, CD, and DAP-normalized CD for the individual operators. A significantly higher radiation exposure comparing the RRA with the RFA was consistently found for all operators. Significant differences in radiation exposure between RFA and LRA and RRA and LRA were found only for 2 of the 5 operators. Radiation exposure for elective and urgent procedures is provided in Table 4 . During elective procedures, radiation exposure was lower for RFA compared with RRA, but not to LRA. However, LRA showed a lower DAP-normalized CD compared with RRA (p <0.001). In addition to the aforementioned differences, LRA was associated with a higher radiation exposure than RFA, when only urgent procedures were considered (p <0.01). In the subgroup of the first consecutive 293 procedures, operator exposure was significantly higher compared with the assistant nurse’s as listed in Table 5 for all procedures and by access site.
| RFA | LRA | RRA | RFA vs. LRA | RFA vs. RRA | LRA vs. RRA | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| p-value | Adjusted difference (95%CI) | Adjusted p-value | p-value | Adjusted difference (95%CI) | Adjusted p-value | p-value | Adjusted difference (95%CI) | Adjusted p-value | ||||
| CA and CA followed by ad hoc PCI | N=455 | N=103 | N=272 | |||||||||
| DAP (Gycm 2 ) | 36 (22-63) | 30 (18-47) | 32 (19-52) | 0.01 | +4 (-11 to 20) | 0.57 | 0.02 | +6 (-3 to 15) | 0.2 | 0.84 | -1 (-9 to 6) | 0.73 |
| CD (μSv) | 3 (1-7) | 6 (3-11) | 12 (6-29) | <0.001 | +1 (-3 to 5) | 0.63 | <0.001 | -16 (-22 to 11) | <0.001 | <0.001 | -20 (-30 to -10) | <0.001 |
| CD/DAP (μSv/Gycm 2 ) | 0.09 (0.02-0.20) | 0.21 (0.10-0.35) | 0.47 (0.25-0.75) | <0.001 | -0.01 (-0.06 to 0.05) | 0.79 | <0.001 | -0.36 (-0.43 to 0.28) | <0.001 | <0.001 | -0.39 (-0.54 to -0.26) | <0.001 |
| CA alone | N=216 | N=65 | N=176 | |||||||||
| DAP (Gycm 2 ) | 24 (16-39) | 24 (15-35) | 27 (17-42) | 1.00 | -2 (-15 to 12) | 0.81 | 0.81 | -6 (-14-2) | 0.12 | 0.67 | -4 (-11-3) | 0.27 |
| CD (μSv) | 2.5 (1-6) | 5 (2-10) | 10 (6-19) | <0.001 | 1 (-2 to 4) | 0.45 | <0.001 | -14 (-21 to -8) | <0.001 | <0.001 | -10 (-18 to -2) | 0.01 |
| CD/DAP (μSv/Gycm 2 ) | 0.10 (0.03-0.22) | 0.21 (0.11-0.38) | 0.44 (0.24-0.71) | <0.001 | -0.01 (-0.01 to 0.07) | 0.91 | <0.001 | -0.30 (-0.37 to -0.23) | <0.001 | <0.001 | -0.25 (-0.36 to -0.14) | <0.001 |
| CA followed by ad hoc PCI | N=239 | N=38 | N=96 | |||||||||
| DAP (Gycm 2 ) | 54 (34-90) | 45 (29-62) | 49 (26-71) | 0.16 | 2 (-25 to 30) | 0.87 | 0.07 | 7 (-10 to 24) | 0.42 | 1.00 | 3 (-11 to 18) | 0.65 |
| CD (μSv) | 4 (1-10) | 6.5 (3-13) | 24 (9.5-45.5) | 0.21 | -1 (-8 to 6) | 0.83 | <0.001 | -23 (-33 to -13) | <0.001 | <0.001 | -30 (-53 to -7) | 0.01 |
| CD/DAP (μSv/Gycm 2 ) | 0.07 (0.02-0.18) | 0.19 (0.10-0.34) | 0.54 (0.27-0.87) | <0.001 | -0.01 (-0.01 to 0.09) | 0.86 | <0.001 | -0.47 (-0.61 to -0.34) | <0.001 | <0.001 | -0.55 (-0.87 to 0.25) | 0.001 |
| RFA | LRA | RRA | p-values | |||
|---|---|---|---|---|---|---|
| RFA vs. LRA | RFA vs. RRA | LRA vs. RRA | ||||
| CA andCA followed by ad hoc PCI | ||||||
| Operator 1 | N=39 | N=77 | N=88 | |||
| DAP (Gycm 2 ) | 31 (20-59) | 28 (17-41) | 32 (19-55) | 0.28 | 1.00 | 0.16 |
| CD (μSv) | 9 (4-15) | 6 (4-11) | 15.5 (8-33) | 0.08 | <0.01 | <0.001 |
| CD/DAP (μSv/Gycm 2 ) | 0.28 (0.16-0.44) | 0.23 (0.14-0.35) | 0.51 (0.37-0.84) | 0.33 | <0.001 | <0.001 |
| Operator 2 | N=132 | N=3 | N=28 | |||
| DAP (Gycm 2 ) | 44 (31-90) | 67 (37-90) | 36 (18-56) | 1.00 | 0.07 | 0.20 |
| CD (μSv) | 1 (0-2) | 1 (0-3) | 1 (0.5-7.5) | 1.00 | <0.01 | 1.00 |
| CD/DAP (μSv/Gycm 2 ) | 0.01 (0-0.04) | 0.01 (0.00-0.04) | 0.05 (0.00-0.17) | 1.00 | <0.01 | 0.53 |
| Operator 3 | N=98 | N=1 | N=3 | |||
| DAP (Gycm 2 ) | 36 (21-67) | 73 | 135 (14-166) | 0.73 | 0.60 | 1.00 |
| CD (μSv) | 4 (2-10) | 7 | 87 (25-484) | 1.00 | <0.01 | 0.02 |
| CD/DAP (μSv/Gycm 2 ) | 0.10 (0.05-0.19) | 0.09 | 1.78 (0.64-2.90) | 1.00 | <0.01 | 0.36 |
| Operator 4 | N=139 | N=12 | N=69 | |||
| DAP (Gycm 2 ) | 30 (17-54) | 36 (24-128) | 33 (22-50) | 0.23 | 0.49 | 0.82 |
| CD (μSv) | 4 (1-6) | 1.5 (1-3.5) | 12 (7-36) | 0.16 | <0.001 | <0.001 |
| CD/DAP (μSv/Gycm 2 ) | 0.10 (0.05-0.18) | 0.05 (0.01-0.08) | 0.45 (0.24-0.78) | <0.01 | <0.001 | <0.001 |
| Operator 5 | N=47 | N=10 | N=84 | |||
| DAP (Gycm 2 ) | 35 (21-51) | 27 (14-49) | 30 (17-47) | 0.92 | 0.40 | 1.00 |
| CD (μSv) | 7 (4-13) | 12 (11-37) | 12 (8-28) | 0.04 | <0.001 | 0.81 |
| CD/DAP (μSv/Gycm 2 ) | 0.21 (0.12-0.35) | 0.59 (0.44-1.43) | 0.48 (0.32-0.72) | <0.01 | <0.001 | 0.55 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


