Improvement of prehospital triage is essential to ensure rapid management of patients with acute myocardial infarction (AMI). This study evaluates the feasibility of prehospital quantitative point-of-care cardiac troponin T (POC-cTnT) analysis, its ability to identify patients with AMI, and its capacity to predict mortality. The study was performed in the Central Denmark Region from May 2010 to May 2011. As a supplement to electrocardiography, a prehospital POC-cTnT measurement was performed by a paramedic in patients with suspected AMI. AMI was diagnosed according to the universal definition of myocardial infarction using the ninety-ninth percentile upper reference level as diagnostic cut point. The paramedics performed POC-cTnT measurements in 985 subjects with a symptom duration of 70 minutes (95% CI, 35 to 180); of whom, 200 (20%) had an AMI. The prehospital sample was obtained 88 minutes (range, 58 to 131) before the sample made on admission to the hospital. The sensitivity for detection of patients with an AMI was 39% (95% CI, 32% to 46%) and the diagnostic accuracy of the POC-cTnT values was 0.67 (95% CI, 0.64 to 0.71). Adjusted survival analysis showed a strong significant association between elevated prehospital POC-cTnT level above the detection level of 50 ng/L and mortality in patients with a suspected AMI irrespective of whether an AMI was diagnosed. In conclusion, large-scale quantitative prehospital POC-cTnT testing by paramedics is feasible. An elevated prehospital POC-cTnT value contains diagnostic information and is highly predictive of mortality in patients with a suspected AMI.
Early and reliable triage of patients with suspected acute myocardial infarction (AMI) is of major importance to promote rapid and appropriate treatment. Prehospital electrocardiographic diagnosis of patients with ST elevation myocardial infarction (STEMI) is a commonly used technology that reduces treatment delay and mortality. However, in many patients with AMI, the electrocardiographic patterns may be ambiguous, and identification of all patients with AMI using the electrocardiogram solely is not possible. Prehospital cardiac troponin T (cTnT) analysis has the potential to accelerate triage and diagnosis of patients with suspected AMI. Large-scale qualitative point-of-care cTnT (POC-cTnT) analysis in ambulances is feasible, but the diagnostic value was limited because of insufficient analytical sensitivity. Quantitative POC-cTnT assays with improved analytical properties are now available, but the prehospital utility has not been evaluated. The purposes of the present study were to (1) evaluate the feasibility of prehospital quantitative POC-cTnT analysis performed by paramedics, (2) determine whether a quantitative prehospital POC-cTnT test is useful for early prehospital identification of AMI, and (3) evaluate the prognostic value of prehospital POC-cTnT analysis in patients with suspected AMI.
Methods
The observational prospective study was performed in ambulances in the eastern part of the Central Denmark Region with a population of approximately 500,000 inhabitants. The paramedics routinely recorded a prehospital electrocardiogram in patients with ongoing or prolonged periods of chest discomfort within the past 12 hours, acute dyspnea in the absence of known pulmonary disease, or a clinical suspicion of AMI. The electrocardiogram was transmitted to the invasive cardiology center at Aarhus University Hospital and interpreted by the cardiologist on call. A telephonic interview was conducted with the patient, and after establishment of a cardiac or a noncardiac tentative diagnosis, the patient was triaged accordingly. During a 1-year period from May 26, 2010 to May 16, 2011, a supplementary prehospital POC-cTnT analysis was performed in consecutive patients having a prehospital electrocardiogram recorded. The study was reviewed by the Regional Ethical Committee and accepted as a quality control study. Oral informed consent for participation in the study was obtained in the ambulance. The study was approved by the Danish Data Protection Agency and the Danish National Board of Health.
Laboratory technicians instructed 9 supervising paramedics in blood sampling and analysis. These paramedics trained the approximately 125 remaining paramedics. Analyses were performed in 25 ambulances. Peripheral intravenous access was obtained as part of routine practice. A blood sample was drawn using a blood collection tube with manually induced vacuum (Sarstedt Lithium-Heparin Coated S-Monovette, 5.5 ml; Sarstedt AG and Co., Nümbrecht, Germany). A 150-μl sample was then analyzed using the Roche Cobas h232 handheld analyzer with the semiquantitative “Cardiac T Quantitative” c-TnT assay (Roche Diagnostics, GmbH, Mannheim, Germany). The analyzer reported the result as negative when the value was <50 ng/L, positive in the interval of 50 to 100 ng/L, and quantitatively positive result at values >100 ng/L. The final result was available after a maximum of 12 minutes. The result of the test was not used for triage. The paramedics performed a daily electronic quality control and 1-monthly control analyses with a dissolved cTnT control material.
The results of the prehospital POC-cTnT measurements and patient identification details were recorded by the paramedics. The cardiologist on call recorded clinical and baseline data as well as the triage decision using a web-based telemedicine database. Prehospital data were obtained from the Central Denmark Region’s Prehospital Emergency Medical Services. Clinical details were acquired from patient files. Survival data were obtained from The Danish Civil Registration System. Baseline health information was obtained from The National Patient Registry.
All admissions were evaluated by any 2 of 3 primary adjudicators (CS, JTS, or CJT) who were blinded to the decision of the other and the prehospital cTnT levels. A diagnosis was adjudicated based on prehospital electrocardiograms along with clinical, imaging, and biochemical data from the admission and 30 days onwards. In case of discrepancies between the primary adjudicators, 2 additional adjudicators (HEB and KT) reviewed the cases to reach consensus. The definitive diagnosis of AMI was established in accordance with the universal definition of myocardial infarction. Myocardial necrosis was confirmed by detection of at least 1 value above the ninety-ninth percentile upper reference level (14 ng/L) of the routine high-sensitivity cTnT assay (Troponin T hs, Roche Diagnostics GmbH, Mannheim, Germany). The criterion for an increase and/or a decrease in high-sensitivity cTnT values was met at >20% change (>50% if the first cTnT measurement was below the ninety-ninth percentile). Roche Diagnostics has released a technical bulletin regarding a calibration issue with this high-sensitivity cTnT assay. We used recalculated high-sensitivity cTnT data for diagnosis adjudication. Patients with an AMI were classified as STEMI or non-STEMI. The diagnosis of unstable angina pectoris was established in patients with an acute ischemic episode that did not fulfill the AMI criteria. Patients without AMI or unstable angina pectoris were categorized as “nonacute coronary syndrome,” and a primary discharge diagnosis was established for this group.
The chi-square test, Kruskal-Wallis test, 1-way analysis of variance, and 2-sample t test were used to test the distribution of binomial and continuous data as appropriate. Differences of proportions were tested using 2-proportion Z-test. Categorical data are shown as absolute numbers (valid cases, percentages). Continuous variables are presented as medians with interquartile ranges, unless otherwise noted. Diagnostic proportions are presented with 95% confidence intervals (CIs). Time on scene was compared with time on scene from a previously described cohort, in which subjects had no POC-cTnT measurements. Nonparametric receiver operating characteristic curves were generated for the full cohort and by 1-hour interval grouping with the diagnostic accuracy of the POC-cTnT measurements described as the area under the curve. We constructed unadjusted Kaplan-Meier curves and calculated mortality rates, stratified to groups of patients with and without AMI, and with and without an elevated prehospital POC-cTnT value of >50 ng/L in combinations. Cox proportional hazard regression was applied to examine the association of an elevated prehospital POC-cTnT levels of >50 ng/L and the reported baseline clinical covariates and mortality. Variables individually associated with mortality (Wald test: p <0.20) were included in the final multivariate Cox regression model if they contributed significantly to the multivariate model (likelihood ratio test <0.05). A family history of ischemic heart disease was excluded in all analyses because of incomplete documentation. Subjects were only included once in survival analysis at first admission if they had prehospital POC-cTnT analysis performed on more occasions. Tests were considered statistically significant if p values were <0.05 (2-sided test). Statistical analyses were performed by CS, JTS, and CJT using Intercooled Stata, version 11 (StataCorp LP, College Station, Texas).
Results
We studied 1,099 admission cases. Blood sampling in the ambulances was successful in 1,075 cases (98%), and the paramedics performed a successful POC-cTnT analysis in 990 subjects (90%). A diagnosis could not be established in 5 cases because of limitations in performing a valid recalculation of the routine cTnT values, leaving 985 cases representing the study cohort. The median time from symptom onset until prehospital blood sampling was 70 minutes (range, 35 to 180). The prehospital blood sample was drawn a median of 88 minutes (range, 58 to 131) before the cTnT measurements made on admission. Time on scene was 25.4 minutes (95% CI 24.8 to 26.0) compared with 22.8 min (95% CI 22.4 to 23.1) in patients from the historical cohort without prehospital POC-cTnT measurements (p <0.001). AMI was diagnosed in 200 cases; 76 subjects (38%) had STEMI and 124 subjects (62%) had non-STEMI. Baseline characteristics are listed in Table 1 .
| Variable | Valid Cases | Cases With Unstable Angina Pectoris (%) | Cases With Acute Myocardial Infarction (%) | Cases Without Acute Coronary Syndrome (%) | p Value |
|---|---|---|---|---|---|
| Total | 985 | 31 (3) | 200 (20) | 754 (77) | |
| Age (yrs) (95% CI) | 985 | 63 (59–66) | 70 (67–71) | 65 (64–66) | <0.0001 |
| Men | 985 | 28 (90) | 142 (71) | 413 (55) | <0.001 |
| Risk factors | |||||
| Hypercholestrolemia | 985 | 28 (90) | 166 (83) | 624 (83) | 0.55 |
| Diabetes | 985 | 7 (23) | 31 (16) | 143 (19) | 0.44 |
| Hypertension | 985 | 20 (65) | 113 (57) | 405 (54) | 0.42 |
| Smoking | 848 | ||||
| Current | 10 (37) | 70 (42) | 210 (32) | 0.05 | |
| Previous | 10 (37) | 59 (36) | 208 (32) | 0.58 | |
| Total | 20 (74) | 129 (78) | 418 (64) | 0.002 | |
| History | |||||
| Previous IHD | 985 | 20 (65) | 86 (43) | 356 (47) | 0.08 |
| Previous AMI | 985 | 14 (45) | 68 (34) | 206 (27) | 0.03 |
| Previous PCI | 985 | 16 (52) | 57 (29) | 179 (24) | 0.001 |
| Previous CABG | 985 | 4 (13) | 17 (9) | 33 (4) | 0.01 |
| Clinical characteristics | |||||
| Symptom duration (minutes) | 923 | 60 (34–219) | 71 (39–152) | 70 (35–197) | 0.98 |
| Systolic blood pressure (mm Hg) | 963 | 150 (138–159) | 150 (131–170) | 145 (129–165) | 0.25 |
| Heart rate (beats/min) | 964 | 76 (74–100) | 85 (70–100) | 84 (70–99) | 0.86 |
| Admission biochemical values | |||||
| eGFR (ml/min) | 770 | 79 (68–85) | 70 (58–83) | 73 (58–87) | 0.08 |
| Creatinine (μmol/L) | 922 | 85 (80–93) | 80.5 (68–100) | 78 (65–95) | 0.03 |
The prehospital POC-cTnT measurements were positive in 113 cases (11%), and 39% (95% CI 32 to 46) of the patients with AMI were correctly identified. Of the 785 cases without an AMI, 95% (95% CI 94 to 97) had a negative POC-cTnT test with an associated negative predictive value of 86% (95% CI 84 to 88), Table 2 . Diagnostic accuracy for the prehospital POC-cTnT measurements was 0.67 (95% CI 0.64 to 0.71). Table 2 lists the diagnostic properties of the prehospital POC-cTnT measurement in categories of 1-hour symptom duration intervals in 923 admissions in which information on symptom duration was available. The diagnostic accuracy increased with symptom duration and each additional 1 hour of symptoms resulted in detection of larger proportions of patients with a positive POC-cTnT value (<60 vs 60 to 120 minutes: p = 0.17; <60 vs >120 minutes: p = 0.01; 60 to 120 vs >120 minutes: p = 0.36).
| Variable | Full Cohort | 923 Cases With Data on Symptom Duration, 196 Cases With AMI | ||
|---|---|---|---|---|
| Symptom Duration, minutes | ||||
| 0–60 | 60–120 | >120 | ||
| Number of cases | 985 | 402 | 200 | 321 |
| Positive result | 113 | 36 | 25 | 49 |
| Sensitivity | 39 (32–46) | 27 (18–38) | 38 (25–52) | 52 (40–65) |
| Positive predictive value | 68 (59–77) | 58 (41–75) | 80 (59–93) | 69 (55–82) |
| Positive likelihood ratio | 8.4 (5.8–12.2) | 5.8 (3.1–10.8) | 11.1 (4.4–28.1) | 8.8 (5.1–15.2) |
| Negative result | 872 | 366 | 175 | 269 |
| Specificity | 95 (94–97) | 95 (93–97) | 97 (92–99) | 94 (90–97) |
| Negative predictive value | 86 (84–88) | 84 (80–88) | 81 (75–87) | 89 (84–92) |
| Negative likelihood ratio | 0.65 (0.58–0.72) | 0.76 (0.67–0.89) | 0.65 (0.52–0.78) | 0.51 (0.39–0.66) |
| Diagnostic accuracy | 0.67 (0.64–0.71) | 0.61 (0.56–0.66) | 0.67 (0.60–0.74) | 0.74 (0.68–0.8) |
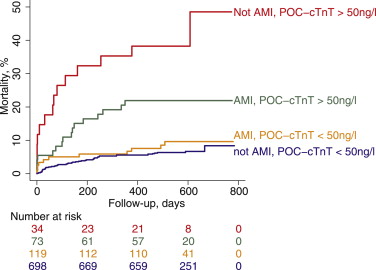
The 985 cases represented 936 subjects. Of these, 9 foreign citizens and 1 who emigrated were lost to follow-up. Status data were not available for 2 subjects, which left 924 subjects for analysis. An elevated POC-cTnT value identified a group with a mortality rate of 23% per year (95% CI 15 to 33) compared with 5% per year (95% CI 4 to 6) for patients without elevated prehospital POC-cTnT values (p <0.001). Kaplan-Meier cumulative mortality curves stratified by groups of patients with or without AMI and with or without elevated prehospital POC-cTnT measurements are shown in Figure 1 . Table 3 lists mortality rates, selected clinical variables, and primary discharge diagnoses for these groups. Of 46 deaths in cases without AMI and a negative POC-cTnT measurement, 26% had a cardiac diagnosis. Of 14 deaths in cases without AMI and a positive POC-cTnT measurement, the diagnosis was cardiac in 71%. Mortality information and complete data for POC-cTnT values and the baseline variables included in the estimated Cox regression model were available for 787 subjects, Table 4 . An elevated prehospital POC-cTnT value above the assay detection limit of 50 ng/L along with age, and a history of AMI were strong independent predictors of death.
| Variable | Valid Cases | POC-cTnT ≤50 ng/L | POC-cTnT >50 ng/L | p Value | ||
|---|---|---|---|---|---|---|
| Not AMI (%) | AMI (%) | Not AMI (%) | AMI (%) | |||
| Total | 698 (76) | 119 (13) | 34 (4) | 73 (8) | ||
| Mortality rate per yr (95% CI) | 924 | 0.04 (0.03–0.06) | 0.06 (0.03–0.11) | 0.38 (0.23–0.65) | 0.17 (0.10–0.27) | <0.001 |
| Age (yrs) (95% CI) | 924 | 65 (63–66) | 69 (67–71) | 76 (72–80) | 71 (68–74) | <0.001 |
| Symptom duration (minutes) | 869 | 69 (35–182) | 65 (33–120) | 71 (37–255) | 102 (56–408) | 0.001 |
| Men | 924 | 377 (54) | 87 (73) | 23 (68) | 48 (66) | <0.001 |
| Previous AMI | 924 | 183 (26) | 46 (39) | 12 (35) | 20 (27) | 0.035 |
| P-creatinine (μmol/L) | 787 | 78 (66–93) | 82 (68–97) | 114 (89–147) | 77 (70–102) | 0.0001 |
| Primary discharge diagnosis | ||||||
| Cardiac | 239 (34) | 22 (65) | ||||
| Unstable angina pectoris | 27 (4) | 0 (0) | 0.24 | |||
| Atrial fibrillation/flutter | 52 (8) | 2 (6) | 0.73 | |||
| Decompensated heart failure | 7 (1) | 3 (9) | <0.0001 | |||
| Stable angina pectoris | 81 (12) | 8 (24) | 0.04 | |||
| Pulmonary embolus | 10 (1) | 3 (9) | 0.001 | |||
| Other cardiac | 62 (9) | 6 (18) | 0.09 | |||
| Noncardiac | 459 (66) | 12 (35) | ||||
| Syncope/dizziness | 39 (6) | 2 (6) | 0.94 | |||
| Pneumonia | 30 (4) | 2 (6) | 0.66 | |||
| Musculoskeletal pain | 52 (8) | 0 (0) | 0.10 | |||
| Nonspecific chest pain | 205 (29) | 4 (12) | 0.03 | |||
| Other noncardiac | 133 (19) | 4 (12) | 0.29 | |||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


