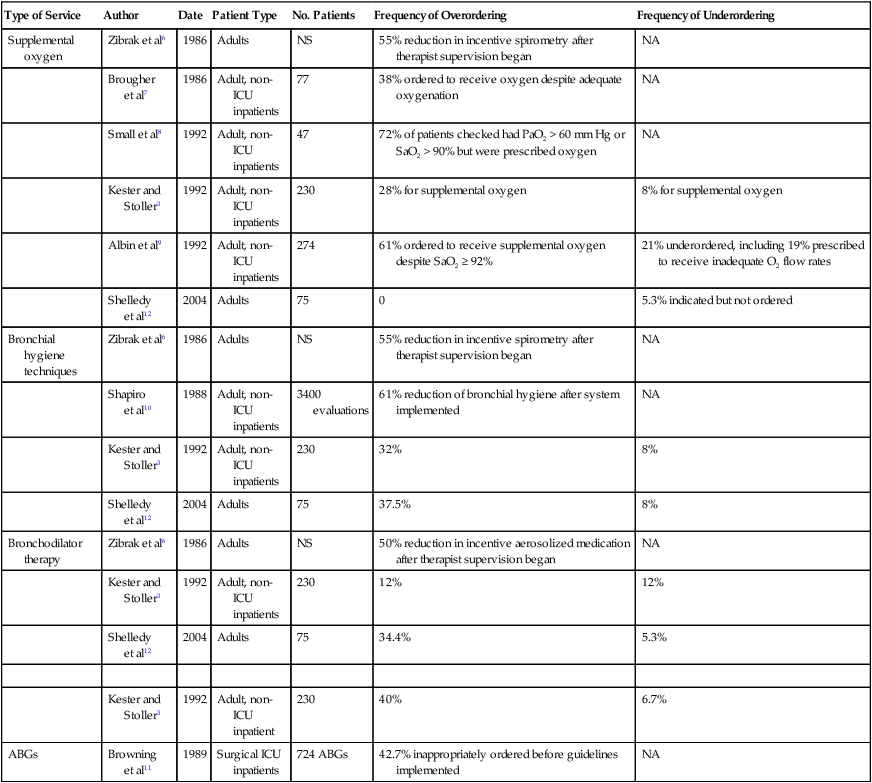
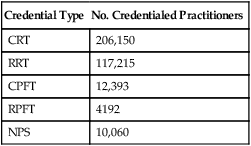
After reading this chapter you will be able to: The medical director of respiratory care is professionally responsible for the clinical function of the department and provides oversight of the clinical care that is delivered (Box 2-1). Medical direction for respiratory care is usually provided by a pulmonary/critical care physician or an anesthesiologist. Whether the role of a respiratory care service medical director is designated as a full-time or part-time position, it is a full-time responsibility; the medical director must be available on a 24-hour basis for consultation with and to give advice to other physicians and the respiratory care staff. The current philosophy of cost containment and cost-effectiveness, dictated by medical care market forces, poses a challenge to the medical and technical leadership of respiratory care services to provide increasingly high-quality patient care at low cost. A medical director must possess administrative and medical skills.1 Perhaps the most essential aspect of providing quality respiratory care is to ensure that the care being provided is indicated and that it is delivered competently and appropriately. Traditionally, the physician has evaluated patients for respiratory care and has written the specific respiratory therapy orders for the respiratory therapist (RT) to follow. However, such traditional practices have often been shown to be associated with misallocation of respiratory care.2–4 This misallocation may consist of ordering therapy that is not indicated, ordering therapy to be delivered by an inappropriate method, or failing to provide therapy that is indicated.5 Table 2-1 reviews studies evaluating the allocation of respiratory care services and the frequency of misallocated care.3,6–12 These studies provide ample evidence that misallocation of respiratory care occurs frequently. Such misallocation has led to the use of respiratory care protocols that are implemented by RTs (as described under Methods for Enhancing the Quality of Respiratory Care). TABLE 2-1 Frequency of Misallocation of Respiratory Care Services in Selected Series NS, Not stated; NA, not assessed. Modified from Stoller JK: The rationale for therapist-driven protocols. Respir Care Clin N Am 2:1–14, 1996. In addition to capable medical direction and the application of well-constructed respiratory care protocols (see p. 26), capable RTs are an indispensable element of a quality respiratory care program. The quality of RTs depends primarily on their training, education, experience, and professionalism. Training teaches students to perform tasks at a competent level, whereas clinical education provides students with a knowledge base they can use in evaluating a situation and making appropriate decisions.13 Both adequate training and clinical education are required to produce qualified RTs for assessment of patients and implementation of respiratory care protocols.14 There are two levels of general practice credentialing in respiratory care: (1) certified respiratory therapists (CRTs) and (2) registered respiratory therapists (RRTs). Students eligible to become CRTs and RRTs are trained and educated in colleges and universities. After completion of an approved respiratory care educational program, a graduate may become credentialed by taking the entry-level examination to become a CRT. A CRT may be eligible to sit for the registry examinations to become a credentialed RRT. Students who complete a 2-year program graduate with an associate degree, and students who complete a 4-year program receive a baccalaureate degree. Some RTs go on to complete a graduate degree (e.g., master or doctorate) with additional study in the areas of respiratory care, education, management, or health sciences. The further development of graduate education in respiratory care has been encouraged by the American Association for Respiratory Care (AARC), and programs are both currently available and under development.15 The primary method of ensuring quality in respiratory care is voluntary certification or registration conducted by the National Board for Respiratory Care (NBRC). The NBRC is an independent national credentialing agency for individuals who work in respiratory care and related services. The NBRC is cooperatively sponsored by the AARC, the ACCP, the ASA, the ATS, and the National Society for Pulmonary Technology. Representatives of these organizations make up the governing board of the NBRC, which assumes the responsibility for all examination standards and policies through a standing committee. The NBRC provides the credentialing process for both the entry-level CRT and the advanced-practitioner RRT. As established in January 2006, to be eligible for either the CRT or the RRT examination, all candidates must have an associate degree or higher. An additional advanced-practitioner credential, the neonatal/pediatric specialist (NPS), has been established for the field of pediatrics. The NBRC also encourages professionals in the field to maintain and upgrade their skills through voluntary recredentialing. Both CRTs and RRTs may demonstrate ongoing professional competence by retaking examinations. Individuals who pass these examinations are issued a certificate recognizing them as “recredentialed” practitioners. In addition to the certification and registration of RTs, the NBRC provides credentialing in the area of pulmonary function testing for certified pulmonary function technologists (CPFTs) and registered pulmonary function technologists (RPFTs). Since its inception, the NBRC has issued more than 350,000 professional credentials to more than 209,000 individuals. As of 2010, there were approximately 206,150 active RTs, many of whom hold more than one credential. Table 2-2 shows the distribution of these credentialed individuals. TABLE 2-2 Distribution of Credentialed Practitioners Licensure and certification help ensure that only qualified RTs participate in the practice of respiratory care. Many institutions conduct annual skills checks or competency evaluations in compliance with TJC requirements. Beyond TJC–required skills checks, experience with respiratory care protocols suggests the need to develop and monitor additional skills among RTs (Box 2-2). Assurance and maintenance of these skills require ongoing training and quality review programs, which are discussed in the section on Monitoring Quality Respiratory Care. By definition, professionalism is a key attribute to which all RTs should aspire and that must guide respiratory care practice. Webster’s New Collegiate Dictionary defines a profession as “a calling that requires specialized knowledge and often long and intensive academic preparation.” A professional is characterized as an individual conforming to the technical and ethical standards of a profession. RTs demonstrate their professionalism by maintaining the highest practice standards, by engaging in ongoing learning, by conducting research to advance the quality of respiratory care, and by participating in organized activities through professional societies such as the AARC and associated state societies. Box 2-3 lists the professional attributes of the RT. We emphasize the importance of these attributes because the continued value and progress of the field depend critically on the professionalism of each practitioner.16 In the highly regulated careers of health care, professionalism also requires compliance with external standards, such as the standards set by TJC and by the government. One such standard is defined by the Health Insurance Portability and Accountability Act (HIPAA) of 1996. HIPAA sets standards regarding the way sensitive health care information is communicated and revealed in the transmission of medical records and in the written and verbal communication of information in the hospital. Some specific provisions of HIPAA are presented in Box 2-4. As with all hospital and health care personnel, standards of respiratory therapy professionalism require knowledge of HIPAA and compliance with its terms.
Quality and Evidence-Based Respiratory Care
 Describe the elements that constitute quality respiratory care.
Describe the elements that constitute quality respiratory care.
 Explain methods used for monitoring the quality of respiratory care that is provided.
Explain methods used for monitoring the quality of respiratory care that is provided.
 Explain how respiratory care protocols enhance the quality of respiratory care services.
Explain how respiratory care protocols enhance the quality of respiratory care services.
Elements of A Hospital-Based Respiratory Care Program: Roles Supporting Quality Care
Medical Direction
Type of Service
Author
Date
Patient Type
No. Patients
Frequency of Overordering
Frequency of Underordering
Supplemental oxygen
Zibrak et al6
1986
Adults
NS
55% reduction in incentive spirometry after therapist supervision began
NA
Brougher et al7
1986
Adult, non-ICU inpatients
77
38% ordered to receive oxygen despite adequate oxygenation
NA
Small et al8
1992
Adult, non-ICU inpatients
47
72% of patients checked had PaO2 > 60 mm Hg or SaO2 > 90% but were prescribed oxygen
NA
Kester and Stoller3
1992
Adult, non-ICU inpatients
230
28% for supplemental oxygen
8% for supplemental oxygen
Albin et al9
1992
Adult, non-ICU inpatients
274
61% ordered to receive supplemental oxygen despite SaO2 ≥ 92%
21% underordered, including 19% prescribed to receive inadequate O2 flow rates
Shelledy et al12
2004
Adults
75
0
5.3% indicated but not ordered
Bronchial hygiene techniques
Zibrak et al6
1986
Adults
NS
55% reduction in incentive spirometry after therapist supervision began
NA
Shapiro et al10
1988
Adult, non-ICU inpatients
3400 evaluations
61% reduction of bronchial hygiene after system implemented
NA
Kester and Stoller3
1992
Adult, non-ICU inpatients
230
32%
8%
Shelledy et al12
2004
Adults
75
37.5%
8%
Bronchodilator therapy
Zibrak et al6
1986
Adults
NS
50% reduction in incentive aerosolized medication after therapist supervision began
NA
Kester and Stoller3
1992
Adult, non-ICU inpatients
230
12%
12%
Shelledy et al12
2004
Adults
75
34.4%
5.3%
Kester and Stoller3
1992
Adult, non-ICU inpatient
230
40%
6.7%
ABGs
Browning et al11
1989
Surgical ICU inpatients
724 ABGs
42.7% inappropriately ordered before guidelines implemented
NA
Respiratory Therapists
Designations and Credentials of Respiratory Therapists
Credential Type
No. Credentialed Practitioners
CRT
206,150
RRT
117,215
CPFT
12,393
RPFT
4192
NPS
10,060
Professionalism
Thoracic Key
Fastest Thoracic Insight Engine





