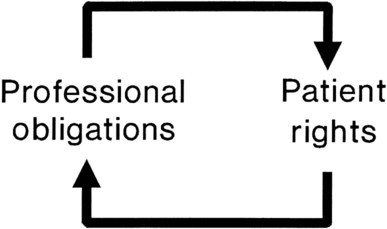
After reading this chapter you will be able to: Although an in-depth discussion of philosophy is beyond the scope of this chapter, it is important to note that ethics has its origins in philosophy. Philosophy may be defined as the love of wisdom and the pursuit of knowledge concerning humankind, nature, and reality.1 Ethics is one of the disciplines of philosophy, which include ontology (the nature of reality), metaphysics (the nature of the universe), epistemology (the nature of knowledge), axiology (the nature, types, and criteria of values), logic, and aesthetics. Ethics is primarily concerned with the question of how we should act. Although ethics may share common origins with the disciplines of law, theology, and economics, as an applied practice, ethics is clearly different from these disciplines.1 Ethics can be described philosophically as a moral principle that supplements the golden rule and can be summed up by a commitment to “respect the humanity in persons.”2 The approaches used to address ethical issues in health care range from the specific to the general. Specific guidance in resolving ethical dilemmas is usually provided by a professional code of ethics. General approaches involve the use of ethical theories and principles to reach a decision.3 A code of ethics is an essential part of any profession that claims to be self-regulating. The adoption of a code of ethics is one way in which an occupational group establishes itself as a profession. A code may try to limit competition, restrict advertisement, or promote a particular image in addition to setting forth rules for conduct.4 The American Association for Respiratory Care (AARC) has also adopted a Statement of Ethics and Professional Conduct. The current code appears in Box 5-1. This code represents a set of general principles and rules that have been developed to help ensure that the health needs of the public are provided in a safe, effective, and caring manner. Codes for different professions might differ from the code governing respiratory care because they may seek different goals. However, all codes of ethics seek to establish parameters of behavior for members of the chosen profession. Professional codes of ethics often represent overly simplistic or prohibitive notions of how to deal with open misbehavior or flagrant abuses of authority. Ethical theories and principles provide the foundation for all ethical behavior. Contemporary ethical principles have evolved from many sources, including Aristotle’s and Aquinas’ natural law, Judeo-Christian morality, Kant’s universal duties, and the values characterizing modern democracy.5,6 Although controversy exists, most ethicists agree that autonomy, veracity, nonmaleficence, beneficence, confidentiality, justice, and role fidelity are the primary guiding principles in contemporary ethical decision making.1,5 Each of these ethical principles, as applied to professional practice, consists of two components: a professional duty and a patient right (Figure 5-1). The principle of autonomy obliges health care professionals to uphold the freedom of will and freedom of action of others. The principle of beneficence obliges health care professionals to further the interests of others either by promoting their good or by actively preventing their harm. The principle of justice obliges health care professionals to ensure that others receive what they rightfully deserve or legitimately claim. When the physician decides to withhold the truth from a conscious, well-oriented adult, the decision affects the interactions between health care providers and the patient and has a chilling effect on the rapport that is so necessary for good care. In a poll conducted by the Louis Harris group, 94% of Americans surveyed indicated that they wanted to know everything about their cases, even the dismal facts. Other than with pediatrics and rare cases in which there is evidence that the truth would lead to a harm (e.g., suicide), the truth, provided in as pleasant a manner as possible, is probably the best policy.7 The principle of nonmaleficence obligates health care providers to avoid harming patients and to prevent harm actively where possible. It is sometimes difficult to uphold this principle in modern medicine because in many cases drugs and procedures have secondary effects that may be harmful in varying degrees. For example, an RT might ask whether it is ethical to give a high dose of steroids to an asthmatic patient, knowing the many harmful consequences of these drugs. One solution to these dilemmas is based on the understanding that many helping actions inevitably have both a good and a bad effect, or double effect. The key is the first intent. If the first intent is good, the harmful effect is viewed as an unintended result. The double effect brings us to the essence of the definition of the word dilemma. The word comes from the Greek terms di, meaning “two,” and lemma, meaning “assumption” or “proposition.”8 In these cases, some individuals interpret the principle of beneficence to mean that they must do everything to promote a patient’s life, regardless of how useful the life might be to that individual. Other professionals in the same situation might believe they are allowing the principle to be better served by doing nothing and allowing death to occur without taking heroic measures to prevent it. In an attempt to allow patients to participate in resolving this dilemma, legal avenues, called advance directives, have been developed.9 Advance directives allow a patient to give direction to health care providers about treatment choices in circumstances in which the patient may no longer be able to provide that direction. The two types of advance directives available at the present time and widely used are the living will and the durable power of attorney for health care. A durable power of attorney for health care allows the patient to identify another person to carry out his or her wishes with respect to health care, whereas a living will states a patient’s health care preferences in writing. As a result of the Patient Self-Determination Act of 1990, most states require that all health care agencies receiving federal reimbursement under Medicare/Medicaid legislation provide adult clients with information on advance directives.9,10 The principle of confidentiality is founded in the Hippocratic Oath; it was later reiterated by the World Medical Association in 1949. It obliges health care providers to “respect the secrets which are confided even after the patient has died.”11 Confidentiality, as with the other axioms of ethics, must often be balanced against other principles, such as beneficence. Confidentiality is usually considered a qualified, rather than an absolute, ethical principle in most health care provider–patient relationships. These qualifications are often written into codes of ethics. The American Medical Association Code of Ethics, Section 9, provides the following guidelines: “A physician may not reveal the confidences entrusted to him in the course of medical attendance or the deficiencies he may observe in the character of patients, unless he is required to do so by law or unless it becomes necessary in order to protect the welfare of the community or a vulnerable individual.” Under the requirements of public health and community welfare, there is often a legal requirement to report such things as child abuse, poisonings, industrial accidents, communicable diseases, blood transfusion reactions, narcotic use, and injuries caused with knives or guns.12 In many states, child abuse statutes protect the health care practitioner from liability in reporting even if the report should prove false as long as the report was made in good faith. Failure to report a case of child abuse can leave the practitioner legally liable for additional injuries that the child may sustain after being returned to the hostile environment.
Ethical and Legal Implications of Practice
 Summarize the philosophical foundations of ethics.
Summarize the philosophical foundations of ethics.
 Explain what constitutes an ethical dilemma and how such dilemmas arise in health care.
Explain what constitutes an ethical dilemma and how such dilemmas arise in health care.
 Describe how professional codes of ethics apply to ethical decision making.
Describe how professional codes of ethics apply to ethical decision making.
 Explain how traditional ethical principles are useful in resolving ethical dilemmas.
Explain how traditional ethical principles are useful in resolving ethical dilemmas.
 Describe the information that should be gathered before making an ethical decision.
Describe the information that should be gathered before making an ethical decision.
 Explain how the systems of civil and criminal law differ.
Explain how the systems of civil and criminal law differ.
 Describe what constitutes professional malpractice and negligence.
Describe what constitutes professional malpractice and negligence.
 Explain how a respiratory therapist can become liable for wrongful acts.
Explain how a respiratory therapist can become liable for wrongful acts.
 List the elements that constitute a practice act.
List the elements that constitute a practice act.
 Explain how licensing affects legal responsibility and liability.
Explain how licensing affects legal responsibility and liability.
 Describe how changes in health care delivery have shaped the ethical and legal aspects of practice.
Describe how changes in health care delivery have shaped the ethical and legal aspects of practice.
 Summarize the basic elements of the Health Insurance Portability and Accountability Act of 1996 (HIPAA)
Summarize the basic elements of the Health Insurance Portability and Accountability Act of 1996 (HIPAA)
 Describe the role of advance directives and living wills in health care.
Describe the role of advance directives and living wills in health care.
Philosophical Foundations of Ethics
Ethical Dilemmas of Practice
Codes of Ethics
Ethical Theories and Principles
Veracity
Nonmaleficence
Beneficence
Confidentiality
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Ethical and Legal Implications of Practice