Fig. 17.2 An ECG from a patient with syncope on QT interval prolonging psychotropic medication: sinus rhythm, unremarkable P wave shape, PR interval. The QRS complex is increased (in lead aVL 14 mm, normal ≤ 11 mm; S lead V2 + R lead V5 = 49 mm, normal ≤ 35 in this age group) suggesting left ventricular hypertrophy (LVH). Note the bizarre T waves, inverted anterolaterally, in a very odd pattern, and with a prominent late ‘hump’ (?U wave) in lead III. The heart rate is 68 b/min, the QT interval 620 ms, with Bazett’s correction (see text) 661 ms (normal ≤ 440 ms) and with Fridericia’s correction (see text) 646 ms. Syncope was due to torsade-de-pointes (TDP).
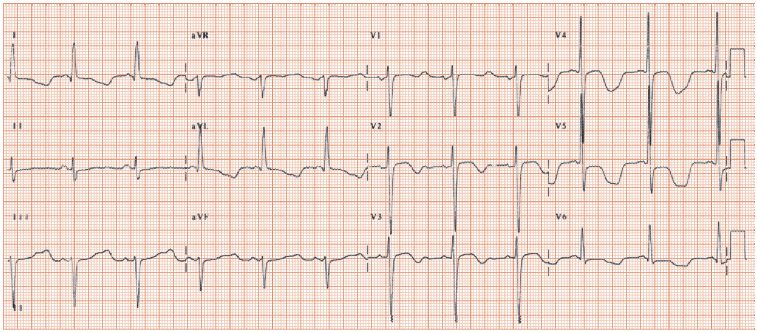
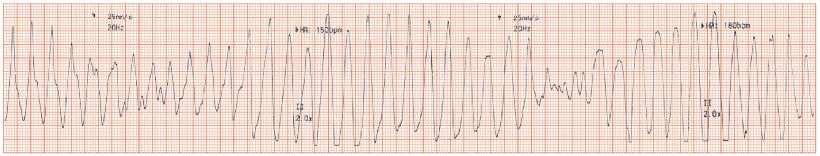
Fig. 17.3 A typical example of torsade-de-pointes (TDP; French, ‘twisting of the points’) type ventricular tachycardia. Fast heart rate, broad QRS complexes, which increase then decrease in size over 10–15 beats. The arrhythmia substantially reduces but usually does not remove cardiac output. Episodes terminate spontaneously (the usual outcome), usually after < 20–30 s, or degenerate into ventricular fibrillation. Typical TDP starts with a short–long–short RR interval sequence, e.g. a premature ventricular ectopic (premature, hence short RR interval), which induces a physiological pause (long RR interval), which results in further QT interval lengthening, and TDP (the first beat occurs early on, so there is a short RR interval). Suppressing any tendency the heart may have towards pauses (using a pacemaker, or isoprenaline), and hence QT prolongation, can suppress TDP.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


