PVOD (Subintimal Recanalization—SAFARI)
NARASIMHAM L. DASIKA
Presentation
A 69-year-old man presented to the clinic with a 2-week history of progressively worsening right foot rest pain. He had multiple bilateral surgical bypass grafts and endovascular procedures in the past 11 years to treat peripheral arterial disease (PAD). Three weeks earlier, he had an unsuccessful thrombolysis of right external iliac artery (EIA) to posterior tibial artery (PTA) composite PTFE and vein graft and an attempted subintimal recanalization of right common femoral artery (CFA) and superficial femoral artery (SFA) from a contralateral left CFA access.
He was advised to have right above-the-knee amputation, but the patient is worried about the prospect of bilateral amputation from his advanced bilateral PAD. His past medical history includes CAD treated with stents, hyperlipidemia, obesity, and sleep apnea. He is a former smoker with a 50-pack-year smoking history. On physical examination, his vital signs are normal. Multiple well-healed groin and lower extremity surgical scars from prior surgeries are seen. He has no leg swelling and no ulcerations and has normal sensory and motor function, except for toe pain on touch. Vascular examination revealed absent palpable right femoral and popliteal pulses, but a dopplerable anterior tibial (AT) artery pulse is present. On the left, he has a feeble but palpable CFA pulse and dopplerable popliteal and pedal pulses.
Differential Diagnosis
Progressively worsening foot pain at rest that is worse in recumbent position with partial relief by standing suggests arterial insufficiency resulting in critical limb ischemia (CLI). Other causes of progressively worsening lower extremity pain include venous disease and peripheral neuropathy. The absence of swelling, relief of pain when the foot is in dependent position, and absence of edema are not in favor of venous disease. The protracted symptoms, rest pain, and examination findings exclude acute limb ischemia (ALI), pseudoclaudication, and neuropathy.
Workup
Workup of a patient with CLI should start with noninvasive vascular evaluation in the clinic. Patients with CLI typically have multilevel vascular lesions and ABI of less than 0.4. Resting segmental waveforms and pressures indicate the level of occlusion and multisegmental involvement. Additional noninvasive imaging with computed tomography angiography (CTA) or magnetic resonance angiography (MRA) is indicated to localize the level and morphology of occlusion, presence of calcium, reconstituted distal arterial anatomy, altered anatomy from prior surgeries, and patency of stents (Figs. 1 and 2). The imaging information allows appropriate treatment decisions to be made. In addition, CTA is very useful in preprocedure endovascular planning in terms of selection of access and devices and thereby reducing the procedure time and contrast load. The blood work should include evaluation of renal function and coagulation profile. Transthoracic echocardiography is recommended when there is history of concomitant ischemic heart disease. Vein mapping for surgical bypass grafts is performed to check for availability of suitable vein conduits for surgical treatment options. Admission and heparinization may have to be considered for patients with limb-threatening ischemia.

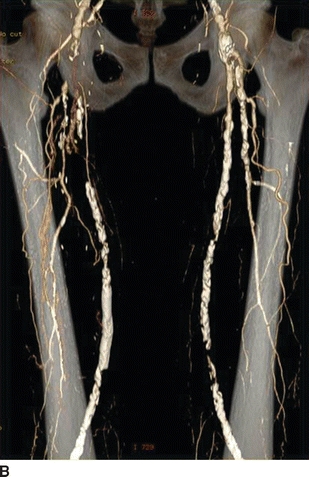

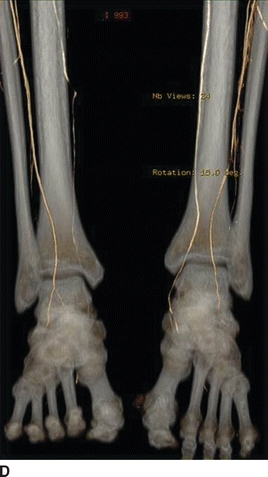
FIGURE 1 CTA reformats showing heavily calcified arterial occlusion of right EIA (A), CFA (B), SFA (C), and popliteal (D) arteries. The anterior tibial artery (D) is reconstituted in the leg. Note bilateral disease that is more severe on the right.

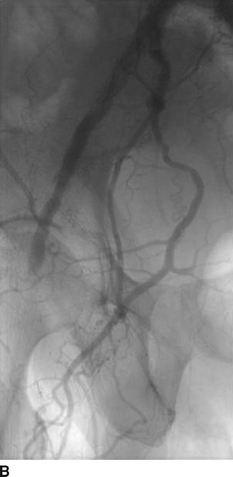
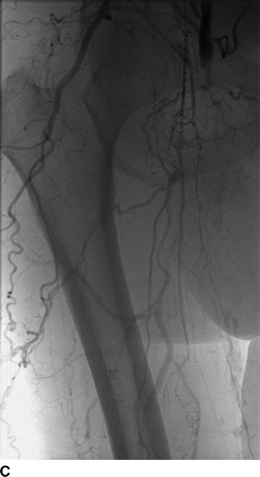


FIGURE 2 Angiogram shows CFA and SFA occlusion (A, B), reconstituted mid profunda femoris artery at mid-thigh (C) from internal iliac artery branches, providing poor collateral arterial supply (D) to AT and peroneal in the leg (E).
Diagnosis and Treatment
Surgical or endovascular revascularizations have to be considered in patients with CLI since medical management is unlikely to give relief from rest pain. When all the surgical options and endovascular options are expended over a period of time, amputation is inevitable. In the presence of advanced arterial disease of the contralateral lower extremity, the prognosis is very poor and the risk of bilateral amputation is high. Patients with CLI from long-segment femoropopliteal occlusions (greater than 15 cm) that are not suitable for surgical or transluminal endovascular options may benefit from PIER procedure (Percutaneous Intentional Extraluminal Recanalization), a technique that has been described by Bolia. PIER procedure is recanalization of an occluded segment made subintimally through the medial layer of the arterial wall. This procedure has a reported success rate of 76% to 84% in revascularization of long-segment chronic total occlusions (CTO). Reentry into the distal patent lumen is the most challenging part of a PIER procedure, resulting in up to 25% technical failure, often due to heavily calcified distal arteries and vascular perforation. Successful reentry can be achieved in some of the failures by the use of reentry devices specifically developed for this purpose. These devices are often difficult to advance through long-segment heavily calcified occlusions from contralateral side and have limited role in reentry into tibial arteries.
A recently introduced technique called SAFARI (Subintimal Arterial Flossing with Antegrade-Retrograde Intervention) significantly improved the success of PIER procedure even in CTOs that extend beyond the popliteal trifurcation into the tibial arteries. SAFARI technique, in principle, is a retrograde PIER procedure performed via retrograde access through a reconstituted distal arterial segment to enter the proximal patent lumen or the subintimal (PIER) channel created from antegrade access. The long retrograde recanalization wire is then grasped and externalized from antegrade access. Further intervention to improve the flow can be performed over both ends of this flossing wire. Even though the early report of this technique was performed through retrograde popliteal access in prone position, AT and PT arteries are most widely selected access arteries for retrograde distal access with the patient in supine position. SAFARI technique has been proven to be invaluable in minimizing the reentry failures and the need for reentry devices during the PIER procedure. The procedure is less invasive than surgery with high technical success and reported patency rates comparable to that of surgical bypass grafts. In addition, the SAFARI technique does not compromise the prospect of a future surgical bypass or the target artery for distal anastomosis. Other advantages of the SAFARI technique are the ability to (1) preserve the patency of large collateral arteries at the proximal and distal end of the CTO; (2) recanalize CTO of additional tibial arteries from antegrade access through the newly created subintimal channel; (3) treat the flow-limiting lesions of the pedal arteries; (4) perform secondary interventions such as plaque debulking if necessary; (5) successful revascularization following a failed PIER procedure in patients with heavily calcified lumen of the distal artery; and (6) recanalize through occluded stents and prior CFA endarterectomy (Figs. 3 and 4).



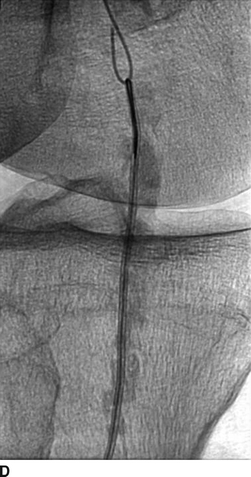
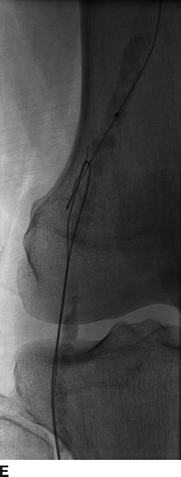
FIGURE 3 Antegrade subintimal recanalization of CFA (A) and SFA (B). SAFARI technique shows the retrograde access from AT in the distal leg (C), retrograde recanalization of popliteal artery (D), and snaring of the retrograde wire from antegrade access to complete recanalization (E). Note the spiraling subintimal channel around the heavily calcified occluded lumen and entering into the fractured overlapping stents in the SFA.



