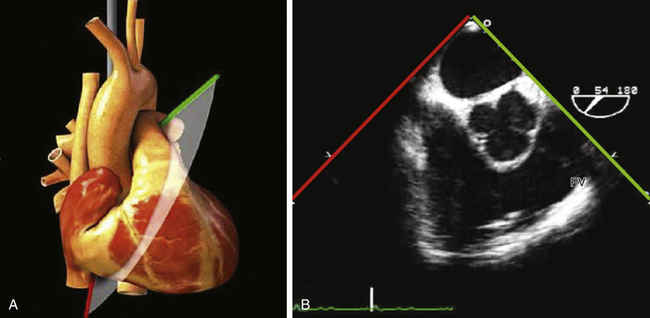
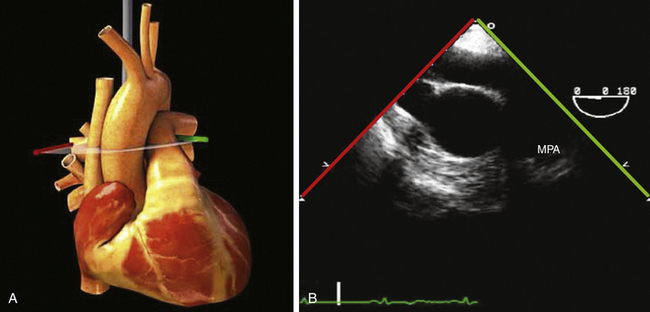
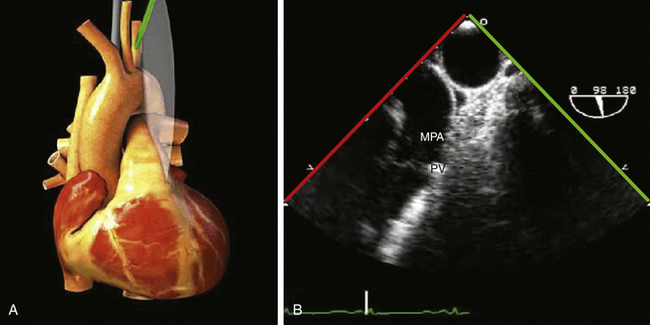
17 Pulmonary valve stenosis is defined as obstruction at the level of the PV and is found in 80% to 90% of all patients with RVOT obstruction. It is the fourth most common congenital heart lesion, occurring in approximately 53 (35-83) per 100,000 live births. 1 The recurrence risk of cardiac disease (pulmonary stenosis [PS] or TOF) in siblings of patients with PS has been reported as 2.1%. 2 The second natural history study of congenital heart defects reported an incidence of definite and possible congenital cardiac defects as 1.1% and 2.1%, respectively. 3 The associated genetic abnormalities include Noonan, Williams, and Alagille syndromes. The MPA and left pulmonary artery are often dilated with isolated PV stenosis. Absence of MPA dilation is seen in conjunction with a dysplastic PV or isolated supravalvar stenosis. Primary fibromuscular narrowing limited to the RVOT is an extremely rare phenomenon that is probably part of the spectrum of illness associated with a double-chambered RV. 4 In comparison, varying degrees of secondary outflow tract narrowing are commonly seen as part of the overall muscular hypertrophy of the RV induced by PS. This secondary obstruction often regresses following valvotomy or valvuloplasty. 5 Supravalvular pulmonic stenosis—isolated or multiple areas of narrowing of the MPA or branches—has been described but is a rare de novo finding in the adult. 6 The most common morphology seen in isolated PS is that of a normal PV that is trileaflet, with a normal annulus dimension and three commissures with varying degrees of fusion. 7 Rarely, bicuspid and unicuspid valves are seen in isolated PS, though these are a more common finding in association with TOF. A small proportion of patients (particularly those with Noonan syndrome) have a markedly dysplastic valve with myxomatous and thickened leaflets, little commissural fusion, and often a hypoplastic annulus and proximal pulmonary artery. 8 These valves are often severely stenotic and usually require repair during childhood. Secondary changes typical of patients with long-standing valvar stenosis include poststenotic dilation of the pulmonary artery, varying degrees of right ventricular hypertrophy, and ultimately, right ventricular dysfunction and dilation. 1. ME RV inflow-outflow view. In the RV inflow-outflow (RVOT) view (60-75 degrees), the imaging plane is directed through the left atrium to image the RV inflow from the tricuspid valve (displayed on the left) and RV outflow through the PV (displayed on the right) in a single view ( Fig. 17-1). Two-dimensional (2D) long-axis imaging of the PV, MPA, and RVOT in a single view is best imaged using this plane. This plane is excellent for assessing additional levels of obstruction involving both the supravalvar and infundibular regions, and in assessment of pulmonary regurgitation (PR). 9 Figure 17-1 A, Midesophageal (ME) right ventricular (RV) inflow-outflow view simulation on three-dimensional heart model. B, ME RV inflow-outflow view. PV, Pulmonary vein. 2. ME ascending aorta short axis (SAX). From ME RV inflow-outflow (60 degrees), withdraw probe from the ascending aorta (AAo) SAX, and rotate the omniplane angle back to 0 degrees. 2D imaging of the right pulmonary artery (RPA) and MPA in long axis is performed using this plane ( Fig. 17-2). The left pulmonary artery (LPA) arches over the left mainstem bronchus after originating from the MPA and is often difficult to visualize because of the interference of the airway ( Figure 17-2 A, Midesophageal (ME) ascending aorta short-axis (SAX) three-dimensional simulation on heart model. B, ME ascending aorta SAX. MPA, Main pulmonary artery. 3. Upper esophageal (UE) aortic arch SAX. From the ME AAo SAX (0 degrees), withdraw probe to obtain the UE aortic arch LAX (0 degrees) view, rotate the omniplane angle to 60 to 90 degrees, and turn the probe to the left to bring the PV and MPA into view ( Fig. 17-3). Retroflexion of the probe at this level will improve the view of the PV. This is also a good imaging plane to align the continuous wave Doppler parallel to flow through the PV and MPA and is useful in assessment of severity of obstruction at these levels. Figure 17-3 A, Upper esophageal (UE) aortic arch short-axis (SAX) simulation on three-dimensional heart. B, UE aortic arch SAX. MPA, Main pulmonary artery; PV, pulmonary vein. 4. Transgastric (TG) LAX. From the deep TG view, with hard antiflexion, rotate the omniplane angle between 70 and 110 degrees (usually at 90 degrees) with rightward flexion to profile the RVOT ( Fig. 17-4
Pulmonic Valvular Disease
![]() Pulmonary Valve Stenosis
Pulmonary Valve Stenosis
Subvalvar Pulmonary Stenosis
Morphology
![]() Transesophageal Echocardiography for Pulmonary Valve Assessment
Transesophageal Echocardiography for Pulmonary Valve Assessment
Imaging Planes Used to Evaluate Right Ventricular Outflow Tract and Pulmonary Valve
![]() Videos 17-1 and 17-2).
Videos 17-1 and 17-2).
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Pulmonic Valvular Disease
