Fig. 14.1
Typical auscultation features of pulmonic regurgitation including a soft systolic, and decrescendo diastolic murmur which varies with respiration
Fig. 14.2
Diastolic murmur in the left lower sternal area that intensifies with inspiration, indicative of a right-sided murmur of pulmonary regurgitation
Test Results
EKG shows right axis deviation (Fig. 14.3).
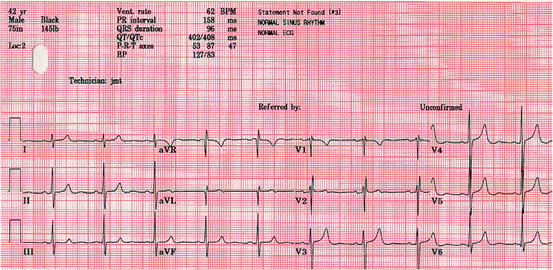
Fig. 14.3
Electrocardiogram showing right axis deviation, and a right ventricular conduction delay, frequent findings in the setting of pathologic lesions affecting the right side of the heart
Key Auscultation Features of the Lesion
Heart sounds relating to pulmonary regurgitation are determined by two factors, the pressure gradient and the degree of regurgitation:
The pressure gradient under which the turbulent flow occurs is determined by the difference between pulmonary diastolic pressure and right ventricular diastolic pressure.
The higher frequency the sound, the higher the pressure difference (e.g., the worse the pulmonary hypertension).
The PR murmur associated with pulmonary regurgitation secondary to pulmonary hypertension is called a Graham Steell murmur (Fig. 14.4).
Fig. 14.4
Compared to healthy patients and patients without a pulmonary regurgitation murmur, the murmur of pulmonary regurgitaton is seen when Doppler evidence of a larger volume and velocity of regurgitation (at least 20 mm on color Doppler) is seen. D: right ventricular diastolic pressure (Used with permission from Takao et al. [4])
In this case, pressure difference is greatest at S2, and gradually diminishes.
This results in a high frequency decrescendo murmur.
The murmur begins at P2, and sounds similar to aortic regurgitation.
A Graham Steell murmur may be differentiated from that of aortic regurgitation by asking the patient to inspire, which increases the amplitude of the murmur.
The S2 split may be narrow or wide.
The murmur is best heard over the pulmonic area.
The P2 may be loud and even palpable at the left second intercostal space.
Low frequency PR murmur is indicative of more normal levels of pulmonary artery pressure.
Initially, during the rapid filling phase, the right ventricular pressure is lower than pulmonary artery pressure. As right ventricular pressure increases with right ventricular filling, the pressure differential decreases.
This results in a short crescendo-decrescendo murmur that sounds like a low-frequency rumble.
The murmur will start after a brief pause following P2.
The S2 split will generally be physiological.
The murmur is best heard over the pulmonic area.
Note that there may also be an associated ejection systolic murmur due to increased right ventricular stroke volume.
Both systolic and diastolic murmurs may be shown to increase in intensity on inspiration.
There may be associated pulmonary ejection clicks.
Degree of regurgitation.
When the degree of regurgitation is severe and long standing, and secondary right ventricular hypertrophy has occurred:
< div class='tao-gold-member'>
Right ventricular diastolic pressure may be increased due to decreased compliance of hypertrophied right ventricle.
This can result in rapid deceleration of regurgitant blood from the pulmonary artery in addition to the flow of blood coming through the tricuspid valve during diastole.
This may produce a right-sided S3.
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


