Fig. 16.1
Echocardiogram. Echocardiogram (apical 4 chamber view) shows an enlarged right ventricle with significant tricuspid regurgitation
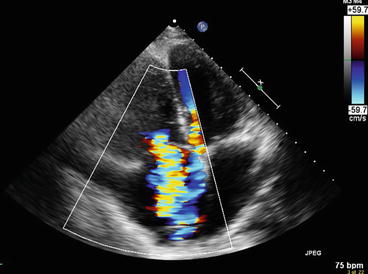
Fig. 16.2
Electrocardiogram. Electrocardiography shows a right bundle branch block with a right axis deviation
Clinical Basics
Normal Anatomy
The right side of the heart receives deoxygenated blood from the body and pumps this blood to the lungs for re-oxygenation.
The blood receives oxygen via gas exchange through blood vessels that course throughout the lungs. Thus, the integrity of these blood vessels is vital in proper functioning of the cardiovascular system.
Because of these functions, the pressure in the pulmonary arteries is lower than in the systemic arteries; at rest, pulmonary artery pressure should be between 10 and 20 mmHg, however this number varies based on a variety of factors, including age and weight. As individuals age, pulmonary artery pressure can be considered normal even in the range of 30–39 mmHg.
When pulmonary artery pressure rises above 40 mmHg, this is a definitive sign of pulmonary hypertension [1].
Definitions
PAH results as a function of increased arterial resistance. This can be associated with a variety of causes, among them lung diseases with affect oxygenation and vascular diseases, which affect vessel tension (Fig. 16.3a, b).
Fig. 16.3
(a, b) Vascular changes seen in pulmonary hypertension. (a) Generalized thickening of vessels of the lung in a case of pulmonary hypertension, magnification 4×. (b) Marked medial wall thickening of a pulmonary vessel in a case of pulmonary hypertension secondary to chronic obstructive pulmonary disease, magnification 10×. (a, b Courtesy of Dr. Deepu Alex and Dr. Mary A. Furlong, Georgetown University, Department of Pathology)
In the setting of PAH, the right ventricle must work harder to pump against the increasing arterial pressure. As opposed to the thick-walled left ventricle, the right ventricle has a thin wall and does not adapt to acute changes in pressure very well. It is more equipped to handle abundant volume than excessive pressure. Over time, this causes hypertrophy and symptoms associated with right-sided heart failure (Fig. 16.4).
Fig. 16.4
Auscultation Features of Pulmonary Hypertension. The schematic portrays the auscultation features that have been affiliated with PAH. Common findings include an ejection click, midsystolic ejection murmur, and an early diastolic decrescendo murmur. Additionally, there is a narrow or single (rare) S2 due to the accentuated P2
Etiology
Pulmonary hypertension can be a sequelae of a variety of conditions.
However, idiopathic pulmonary arterial hypertension (IPAH) exists when an underlying cause cannot be identified.
Potential etiologies.
Genetic – familial pulmonary hypertension is caused by a mutation in BMPR2 [2].
Drugs and toxins.
Connective tissue diseases – these include Systemic Sclerosis, Rheumatoid Arthritis, and Systemic Lupus Erythematosus.
Human Immunodeficiency Virus.
Portopulmonary hypertension.
Congenital heart disease.
Sleep apnea.
Chronic thromboembolic disease.
Chronic advanced lung disease.
Signs and Symptoms
Fatigue.
Dyspnea.
Dizziness.
Syncope.
Bilateral lower extremity edema.
Cyanosis.
Chest pain.
Tachycardia/palpitations.
Prevalence
In the USA, 500–1,000 new cases of primary pulmonary hypertension are diagnosed each year [3].
Key Auscultation Features of the Lesion (Fig. 16.3)
Increased intensity of the pulmonic component of the second heart sound, P2.
The most common cause of an increased P2 sound is pulmonary hypertension of any etiology [4].
The increased intensity of P2 may exceed, or be increased although still overall softer than A2.
Very narrow physiological splitting of S2 due to the early occurrence of P2.
A2 and P2 may still be faintly heard as two distinct sounds upon expiration.
A single S2 may be heard but it must be noted that a truly single S2 is rare.
Fusion of A2 and P2 without inspiratory splitting may occur.
May be due to a soft pulmonic element.
A single S2 is rare in healthy infants, children adults, and even in elderly although advanced age increases the likelihood of hearing a single S2 during both respiratory phases.
Lung hyperinflation is the most prevalent cause of inability to hear the pulmonic closure.
Emphysema, obesity or pericardial effusion may obscure the auscultation or ability to record the P2.
A late wide splitting of S2 due to conduction disturbances results from the presence of right ventricular failure, subsequently leading to delayed right ventricular ejection.
A diastolic murmur that sounds high-pitched and blowing can result from pathologic pulmonary regurgitation associated with hypertension.
There may be few cases of normal pulmonic regurgitation in thin individuals.
Sustained parasternal or subxiphoid impulse may be present and signify right ventricular enlargement or overload.
Elevated JVP due to tricuspid incompetence.
A single outward systolic movement occurs concurrently with the carotid pulse and diminishes in the early diastole phase, after S2.
With respect to primary pulmonary hypertension or IPAH, unique auscultation features may include.
Vibratory S1.
A short midsystolic murmur after the ejection click.
Auscultation example of pulmonary hypertension.
Click here to listen to an example of heart sounds in pulmonary hypertension and to view an image of the phonocardiogram (Video 16.1).
Auscultation Differential Diagnosis
There are not many clinical syndromes that can resemble primary pulmonary hypertension, however it is unequivocally important to be aware its presence.
Pulmonary stenosis associated with an ejection murmur.
Pulmonary ejection click heard in the left second intercostal space.
Frequently, accompanied by a palpable thrill.
It can mainly be differentiated from primary pulmonary hypertension by its wide S2 split and increased P2 intensity.
As noted before, an accentuated physiologic P2 can be heard in young and thin individuals.
Diagnostic Implications of Auscultation Features (Table 16.1)
Table 16.1
Relevant physical examination findings for PAH: signs and implications
Inspection | |
|---|---|
Signs | Implications |
Left parasternal lift | High right ventricular pressure and hypertrophy |
Jugular venous distension | Right ventricular dysfunction and/or tricuspid regurgitation |
Peripheral edema and ascites | |
Low blood pressure, diminished pulse pressure and cool extremities | Reduced cardiac output, peripheral vasoconstriction |
Palpation | |
Hepatomegaly | Right ventricular dysfunction and/or tricuspid regurgitation |
Pulsatile liver | |
Hepatojugular reflux | High central venous pressure |
Auscultation | |
Accentuated pulmonary component of S2 audible at apex (over 90 %) | High pulmonary pressure increases force of pulmonic valve closure |
Early systolic click | Sudden interruption of opening of pulmonary valve into high-pressure artery |
Midsystolic ejection murmur | Turbulent transvalvular pulmonary outflow |
Right ventricular S4 (38 %) | High right ventricular pressure and hypertrophy present |
Increased jugular “a” wave | Poor right ventricular compliance |
Holosystolic murmur increasing with inspiration | Tricuspid regurgitation |
Increased jugular v waves | |
Diastolic murmur | Pulmonary regurgitation |
Right ventricular S3 (23 %) | Right ventricular dysfunction |
A high index of suspicion is a necessity when diagnosing PAH given that its symptoms are common to other disorders. PAH should be considered in the differential if a patient presents with exertion, fatigue or exercise limitation and a family history of PAH. Symptoms at rest are usually only noticed in severe PAH [5].
An ejection click is due to stiffened pulmonary valve cusps caused by high pressure in the pulmonary artery and a dilated pulmonary artery root [6]. This occurs later in systole as opposed to with the first heart sound in pulmonary valve stenosis [7].
A narrowly split S2 due to an early loud P2 is heard in early pulmonary hypertension, while the split widens in late pulmonary hypertension due to right ventricular failure [6].
Moderate to severe PAH signs include holosystolic murmur that increases with inspiration (due to tricuspid regurgitation), diastolic murmur (due to pulmonary regurgitation) and increased jugular v waves [8].< div class='tao-gold-member'>Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


