We undertook this systematic review to determine the prognostic significance of adrenomedullin (ADM) in patients with heart failure and acute myocardial infarction (AMI). Given the difficulty in measuring mature ADM, its surrogate, midregional proadrenomedullin (MRproADM) has been used in most studies. Systematic search of original published studies through MEDLINE and the Cochrane Collaboration databases restricted to reports in English from January 1, 1993, to June 30, 2014, in humans was undertaken. Heterogeneity of studies prohibited a meta-analysis. In patients with heart failure, the area under the curve for prediction of mortality by MRproADM ranged from 0.68 to 0.81 (95% confidence intervals [CI] 0.63 to 0.91) across studies. One nmol/l increase in MRproADM was associated with hazard ratios (HRs) ranging from 1.77 to 2.79 (95% CI 1.29 to 5.95) for death in patients with heart failure. In patients with AMI, the area under the curve for MRproADM predicting MACE ranged from 0.64 to 0.80 (CI 0.51 to 0.87) across studies and death 0.79 to 0.84 (CI 0.73 to 0.90). One nmol/l increase in MRproADM was associated with HR for MACE ranging from 1.78 to 4.10 (CI 1.20 to 10.12), whereas log10 of MRproADM had HRs of 3.63 to 9.75 (CI 1.48 to 26.16) for MACE and 4.86 to 16.68 (CI 4.56 to 60.99) for death across studies in patients with AMI. In conclusion, adrenomedullin is an independent predictor of death in patients with heart failure and of MACE and death in patients who have suffered an AMI. Quantification of this peptide might contribute to improved risk stratification in settings of heart failure and myocardial infarction.
Highlights
- •
This systematic review shows that adrenomedullin is an independent predictor of death in patients with heart failure and of major adverse cardiovascular events and death in patients who have suffered an acute myocardial infarction.
- •
Quantification of this peptide might contribute to improved risk stratification in settings of heart failure and myocardial infarction.
Adrenomedullin (ADM) is produced from a large peptide precursor molecule (preproadrenomedullin) which consists of 185 amino acids through a 2-staged enzymatic process into the mature form with 52 amino acids. The gene encoding for adrenomedullin is located within the short arm of chromosome 11. Measurement of mature ADM as biomarker has been previously hampered by its short plasma half-life of 22 ± 1.6 minutes, the presence of a binding protein called human adrenomedullin-binding protein (AMBP-1) identified as complement factor H, and the immediate binding of ADM to local receptors, which had rendered its accurate measurement difficult to achieve. A possible solution to this problem came from the development of assays to identify midregional proadrenomedullin (MRproADM), which is a more stable nonfunctional fragment of initial precursor peptide, consisting of 45 to 92 amino acids. MRproADM is secreted in stoichiometric amounts to mature ADM and therefore acts as a reliable surrogate of ADM levels. To the best of our knowledge, no study has undertaken a systematic review or meta-analysis of ADM and incident major cardiovascular events or mortality in patients with heart failure or acute myocardial infarction (AMI). We therefore undertook this systematic review with the hope of including a meta-analysis if possible, to determine the prognostic significance of ADM in patients with heart failure and post-AMI.
Methods
The method was guided by Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA). The inclusion criteria were prospective studies published in adult patients with acute or chronic heart failure or AMI or patients presenting with acute dyspnea or acute chest pain or stable or unstable angina. In addition, they must have had adrenomedullin measured at baseline and related to major adverse cardiovascular events (MACE) or mortality. Excluded were review articles, pediatric studies, and animal studies.
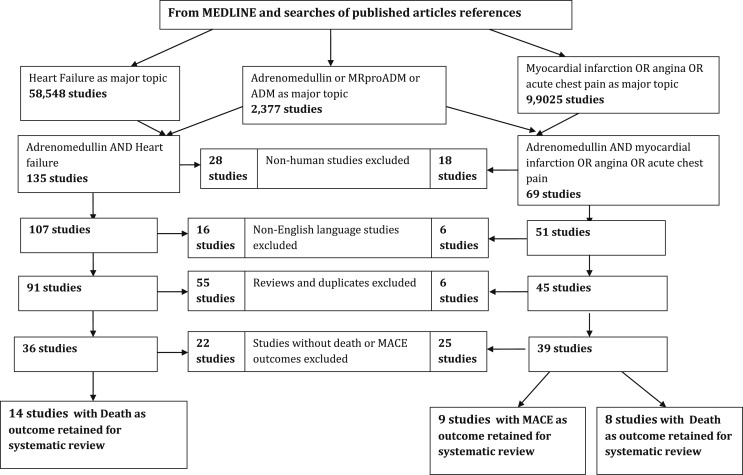
A systematic search of studies was carried out on original published studies using PubMed (MEDLINE) and the Cochrane Collaboration databases using key words and MeSH terms. For patients with heart failure, the MeSH terms or key words were (“Adrenomedullin” OR “ADM” OR “MRproADM”) AND “Heart Failure.” For patients with myocardial infarction, these were (“Myocardial Infarction” OR “Angina Pectoris” OR “Angina, Stable” OR “Angina, Unstable”) AND (“Adrenomedullin” OR “ADM” OR “MRproADM”). Searches of references of published reports obtained from the aforementioned systematic search were also undertaken. The search was restricted to reports published in English from January 1, 1993, to June 30, 2014, in humans. Figure 1 shows the flow chart for selection for this systematic review.
The main outcome measure of this systematic review for patients with heart failure was death. The outcome measure for patients with myocardial infarction was MACE as primary end point measure, with death as secondary end point. The end point, MACE, was defined variably across studies as a composite of myocardial infarction, stroke, hospitalization for heart failure, and all-cause mortality, although in some studies not all these components were present.
Two authors independently perused all the relevant titles and abstracted data from selected reports with any disagreements settled by a consensus or opinion from other co-authors. Some studies had very small sample sizes, but we included given the small number of studies.
Because of the high level of heterogeneity across studies, no quantitative pooling of results from various studies through a meta-analysis was undertaken. This heterogeneity was mainly due to the discrepancy in type of adrenomedullin measured (mature ADM vs its surrogate MRproADM), discrepancy in units of ADM used by different studies, the varying use of ADM as a continuous and a categorical variable across studies, the different cutoffs of ADM when used as a categorical variable, and differing logarithmic transformations or unit change of ADM when used as a continuous variable in various statistical models.
Results
Table 1 lists studies which looked at the relation between ADM and mortality in patients with heart failure. We identified 14 studies in total, and these were mainly cohort studies. Baseline plasma levels of MRproADM were significantly higher in patients who died during follow-up compared with the levels of those who survived. The area under the curve (AUC) for adrenomedullin predicting mortality was only reported for 12 studies using MRproADM in patients with heart failure, and this ranged from 0.68 to 0.81 (95% confidence interval [CI] 0.63 to 0.91) across studies. Overall, the earlier studies using mature adrenomedullin demonstrated a statistically significant association from hazard ratios (HRs) and 95% CIs with all-cause mortality. Subsequent studies using MRproADM showed similar results. When taken as a continuous variable, a 1 nmol/l increase in MRproADM was associated with HRs ranging from 1.77 to 2.79 (95% CI 1.29 to 5.95) for death in patients with heart failure. When taken as a log10 of MRproADM measured in nanomoles per liter, the HRs ranged from 1.82 to 10.26 for death (95% CI 1.26 to 80.50). Various cutoffs were used for categorical adrenomedullin as presented in Table 1 , and these included upper tertile, receiver operating characteristic optimal cutoff, and above the median value. Only one study showed a negative result of MRproADM on mortality in heart failure patients.
| Author | Year | Sample size | Number of Deaths | HR (95% CI) | AUC (95% CI or p-value) | Duration follow-up | Measure of Adrenomedullin | Primary endpoint | Modelled adrenomedullin |
|---|---|---|---|---|---|---|---|---|---|
| Pousset | 2000 | 117 | 14 | 1.56 (1.05-2.32) | NA | 237 days | Mature ADM | Death, cardiac transplant | 1 SD increase, pg/ml |
| Richards | 2001 | 297 | 35 | 3.92 (1.76-8.70) | NA | 300 days | Mature ADM | Death, HF hospitalization | Above median, pmol/l |
| Gegenhuber | 2007 | 137 | 41 | 2.11 (0.93-4.77) | 0.71 (0.63-0.79) | 365 days | MRproADM | Death | Upper tertile > 1.23, nmol/l |
| Adlbrecht | 2009 | 786 | 233 | 1.77 (1.41-2.22) | NA | 24 Months | MRproADM | Death | Continuous, 1 nmol/l |
| Potocki | 2009 | 287 acute dyspnoea 54% AHF | 77 | 10.46 (1.26-80.50) | 0.75 (0.69-0.81) | 1 year | MRproADM | Death | Log10 MRproADM, nmol/l |
| Masson | 2010 | 1237 | 332 | 1.91 (1.29-2.82) | 0.70 (0.67-0.74) | 3.9 yrs | MRproADM | Death | Upper tertile >/= 0.88 ,nmom/l |
| Neuhold | 2010 | 181 | 36 | 2.79 (1.29-5.95) | NA | 24 months | MRproADM | Death | Continuous, 1 nmol/l |
| Haehling | 2010 | 501 | 70 | 1.82 (1.24-2.66) | 0.72 (0.67-0.76) | 1 year | MRproADM | Death | Log10 MRproADM, nmol/l |
| Maisel | 2011 | 568 AHF | 65 | 2.4 (1.40-4.40) | 0.67 (NA) | 90 days | MRproADM | Death | Log10 MRproADM, nmol/l |
| Shah | 2012 | 560 acute dyspnoea 180 AHF | 189 | 1.51 (1.03-2.20) | 0.77 (p<0.001) | 4 years | MRproADM | Death | ROC curve optimal cut-off value of 0.77, nmol/l |
| Cinar | 2012 | 154 acute dyspnoea 42.2 % AHF | 15 | 8.5 (2.50-28.50) | 0.81 (0.71-0.91) | 30 days | MRproADM | Death | Cut-off 1.5, nmol/l |
| Bosselmann | 2013 | 424 | 252 | 2.37 (1.66-3.38) | NA | 4.9 years | MRproADM | Death | Continuous 1 nmol/l |
| Xue | 2013 | 724 | 195 | 2.307 (P<0.001) | 0.68 (P<0.00001) | 6 years | MRproADM | Death | ROC curve optimal cut-off value of 0.72, nmol/l |
| Travaglino | 2014 | 441 acute dyspnoea 162 AHF | 21 | NA | 0.66 (p<0.001) | 90 days | MRproADM | Death | AUC for baseline MRproADM, nmol/l |
Table 2 depicts studies which looked at the relation between adrenomedullin and MACE in patients with acute coronary syndrome. We identified 9 cohort studies in total. Baseline plasma levels of MRproADM were significantly higher in patients who experienced a MACE during follow-up compared with the levels of those who did not. The AUC for MRproADM predicting MACE ranged from 0.64 to 0.80 (95% CI 0.51 to 0.87) across studies in patients with AMI. When taken as a continuous variable, 1 nmol/L increase in MRproADM was associated with HRs for MACE ranging from 1.78 to 4.10 (95% CI 1.20 to 10.12), whereas log10 of MRproADM had HRs of 3.63 to 9.75 (95% CI 1.48 to 26.16) for MACE across studies in patients with AMI. Only 1 study showed a negative result of MRproADM on MACE in patients with AMI. This review also identified studies which have shown that MRproADM significantly enhances the integrated discrimination improvement (IDI) and the net reclassification improvement (NRI) when added to other risk markers such as brain natriuretic peptide and the GRACE score in patients with AMI. For example, 1 study showed an NRI of 34.1% (range 18.6% to 49.5%) for 30-day mortality when MRproADM was added to the GRACE score.
| Author | Year | Sample size | MACE | HR MACE (95% CI) | AUC (95 % CI) | Duration of follow-up | Measure of Adrenomedullin | Primary endpoint | Modelled adrenomedullin |
|---|---|---|---|---|---|---|---|---|---|
| Khan | 2007 | 983 | 150 | 3.63 (1.48-8.90) | 0.77 (0.72-0.81) | 2.1 years | MRproADM | Death, HF | Log Base10 MRproADM, nmol/l |
| Behnes | 2008 | 30 | 11 | 2.80 (1.20-6.90) | 0.71 (0.51-0.86) | 10 months | MRproADM | Death, HF, PCI, CABG | Continuous 1, nmol/l |
| Dhillon | 2010 | 745 | 262 | 9.75 (3.60-26.16) | 0.72 (0.67-0.77) | 2 years | MRproADM | Death, HF, AMI | Log Base10 MRproADM, nmol/l |
| Walter | 2010 | 30 | 11 | 2.80 (1.20-6.90) | 0.71 (0.51-0.86) | 10 months | MRproADM | Death, HF, PCI, CABG | Continuous, 1 nmol/l |
| Klip | 2011 | 214 | 61 | 1.78 (0.94-3.35) | 0.66 (0.58-0.75) | 2.5 years | MRproADM | Death, AMI, Stroke, resuscitated CA | Doubling of MRproADM, nmol/l |
| Dzielinska | 2011 | 127 | 12 | 2.12 (1.18-3.81) | NA | 6 months | Mature ADM | Death, AMI, Stroke | Every 10 pmol/l increase |
| Wild | 2012 | 1355 stable angina | 90 | 3.40 (1.06-10.92) | 0.64 (0.57-0.71) | 3.6 years | MRproADM | Nonfatal AMI or CVD death | Continuous, 1 nmol/l |
| Wild | 2012 | 885 ACS | 102 | 4.10 (1.66-10.12) | 0.64 (0.57-0.70) | 3.6 years | MRproADM | Nonfatal AMI or CVD death | Continuous 1 nmol/l |
| Meune | 2012 | 1247 acute chest pain | 21 | 8.70 (1.10-69.4) 3rd quartile to 1st & 10.90 (1.40-85.4) 4th quartile to 1st | 0.71 (0.62-0.81) | 22 Months | MRproADM | Death, AMI | 3rd quartile compared to 1st, nmol/l & 4th quartile compared to 1st, nmol/l |
| Tzikas | 2013 | 1386 acute chest pain | 132 | 1.26 (1.06-1.49) | 0.80 (0.73-0.87) | 6 months | MRProADM | Death, AMI, Revascularization, Stroke, HF | 1 SD log-transformed MRproADM, nmol/l |
Table 3 depicts studies which looked at the relation between adrenomedullin and death in patients with AMI. We identified 8 cohort studies in total. The AUC for MRproADM predicting death ranged from 0.79 to 0.84 (95% CI 0.73 to 0.90) across studies in patients with AMI. When taken as a log10 of MRproADM measured in nanomoles per liter, death was associated with HRs ranging from 4.86 to 16.68 (95% CI 4.56 to 60.99) across studies in patients with AMI. One study showed a negative result of MRproADM on mortality in patients with AMI.
| Author | Year | Sample size | Number of Deaths | HR Death (95% CI or P value) | AUC (95% CI) | Duration follow-up | Measure of Adrenomedullin | Primary endpoint | Modelled adrenomedullin |
|---|---|---|---|---|---|---|---|---|---|
| Richards | 1998 | 121 | 27 | 1.21 (not significant) | NA | 2 4 month | Mature ADM | Death, HF | Continuous, 1 pmol/l |
| Richards | 2001 | 297 | 35 | 3.92 (1.76-8.70) | NA | 18 months | Mature ADM | Death, HF | Above median, pmol/l |
| Nagaya | 1999 | 113 | 16 | 1.04 (1.01-1.08) | NA | 25 months | Mature ADM | Cardiovascular death | Continuous, 1 pmol/l |
| Katayama | 2005 | 124 | 9 | 10.63 (1.06-107.06) | NA | 90 days | Mature ADM | Death | Continuous 1, fmol/l |
| Khan | 2007 | 983 | 101 | 4.86 (p=0.001) | NA | 2.1 years | MRproADM | Death, HF | Log Base10 MRproADM, nmol/l |
| Dhillon | 2010 | 745 | 120 | 16.68 (4.56-60.99) | 0.79 (0.74-0.84) | 2 years | MRproADM | Death, HF, AMI | Log Base10 MRproADM, nmol/l |
| Klip | 2011 | 214 | 31 | 3.51 (1.38-5.49) | 0.81 (0.73-0.90) | 2.5 years | MRproADM | Death, AMI, Stroke, resuscitated CA | Doubling of MRproADM, nmol/l |
| Haaf | 2013 | 1179 Acute chest pain | 79 | 2.79 (1.81-4.33) | 0.84 (0.81-0.86) | 2 years | MRproADM | Death | Continuous, 1 nmol/l |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


