Patients with acute coronary syndromes have a substantial disease burden and are at continued risk of future cardiovascular events. In this setting, the relation between previous myocardial infarction (MI) and the risk of subsequent in-hospital adverse cardiovascular outcomes has not been definitively established. The data were analyzed from 427,778 hospitalized patients presenting with acute MI from July 2002 to December 2006, who were enrolled in the National Registry of Myocardial Infarction 4-5 study. Multivariate logistic regression models were developed to examine the association between a history of MI and in-hospital all-cause mortality, recurrent MI, and congestive heart failure/pulmonary edema. Covariate adjustments were made for demographic characteristics, co-morbidities, prearrival medications, and health status at presentation. Similarly, multivariate linear regression models were used to evaluate the length of stay. Of the 232,927 patients with acute MI included in the present study after exclusions, 24.7% reported a history of MI. In-hospital mortality was not significantly different between the patients with and without a history of MI (adjusted odds ratio 0.99, 95% confidence interval 0.95 to 1.04, p = 0.75). However, patients with a previous MI had a small increased risk of in-hospital recurrent MI (adjusted odds ratio 1.18, 95% confidence interval 1.08 to 1.29, p <0.001) and congestive heart failure/pulmonary edema (adjusted odds ratio 1.23, 95% confidence interval1.19 to 1.28, p <0.001) compared with patients with no history of MI. In conclusion, a history of MI did not significantly affect in-hospital mortality after admission for an acute MI.
Although it is well recognized that patients with recurrent acute myocardial infarction (MI) have an increased risk of subsequent adverse cardiovascular (CV) outcomes, a paucity of analyses of large, nationally representative observational data evaluating the sequelae associated with recurrent acute MI is available. Moreover, few observational studies have evaluated the differences in the short-term in-hospital prognosis after an acute MI according to the patients’ history of MI. The primary objective of the present study was to report the differences in in-hospital adverse clinical outcomes in National Registry of Myocardial Infarction (NRMI) 4-5 patients with and without a reported history of MI. The primary outcome was all-cause mortality; the secondary outcomes included recurrent in-hospital MI, congestive heart failure (CHF)/pulmonary edema, and length of stay (LOS).
Methods
The NRMI was a prospective, observational study of patients presenting with acute MI in the United States that was launched in 1990. It was divided into substudies with varying focus and revisions to the data collected. For the present study, the data from 427,778 patients admitted to 836 hospitals participating in NRMI 4 and 5 and discharged from July 2002 to December 2006 were available for analysis. The study design and data collection detail for NRMI have been previously described. The patients transferred into or out of the participating hospitals were excluded because of the potential for incomplete data on presentation, treatment, or hospital outcome. The patient records without lipid values were also excluded. Thus, 232,927 nontransferred patients with a principle diagnosis of acute MI (“International Classification of Disease, 9th revision,” code 410.x) who were discharged from 823 participating hospitals from July 2002 to December 2006 were included in the present analyses.
The mean values ± SD were calculated for the continuous variables and percentages for the categorical variables. For discrete data, Pearson’s chi-square test was used to detect any differences among the comparison groups. For continuous data, the mean values were compared using 1-way analysis of variance or Wilcoxon nonparametric tests. All hypothesis testing was 2-sided, and p ≤0.05 was considered significant. The selection of variables in the regression models was also based on p ≤0.05. The analyses were conducted using Statistical Analysis Systems, version 9.2 (SAS Institute, Cary, North Carolina).
Multivariate linear and logistic regression models were developed to evaluate the independent association of a history of MI with each of 4 in-hospital clinical outcomes. Two models were analyzed using a backward-elimination approach. The first model assessed the unadjusted main effect of a previous MI on each selected event. In the second model, the candidate covariates for the multivariate model included the baseline demographics (including gender and ethnicity), medical history, prearrival medications, clinical presentation, and reperfusion use and timing. A previous MI as a main effect was retained in these multivariate models. The data were collected as previously described for the NRMI.
The primary in-hospital outcome was all-cause mortality; the secondary outcomes included recurrent MI, CHF/pulmonary edema, and LOS. Adjusted odds ratios and coefficient estimates are presented with the corresponding 95% confidence intervals.
Results
Of the 232,927-patient cohort admitted to the hospital for acute MI, 24.7% had a history of MI. The patients with a history of MI, on average, were significantly older and had significantly greater rates of a reported history of diabetes, hypertension, hypercholesterolemia, peripheral vascular disease, and other CV history ( Table 1 ). At presentation, the patients with a history of MI had minimal differences in systolic blood pressure and heart rate compared with those without. Patients with a history of MI were also less likely to present with ST-segment elevation MI and were more likely to have a lower left ventricular function index at presentation and Killip class III-IV CHF.
| Variable | All Patients (n = 232,927) | Previous MI | |
|---|---|---|---|
| Yes (n = 57,492) | No (n = 175,435) | ||
| Demographics | |||
| Women | 96,075 (41.3%) | 21,979 (38.2%) | 74,096 (42.2%) |
| Age (yrs) ∗ | 69.4 ± 13.9 | 71.4 ± 13.3 | 68.7 ± 14.1 |
| Race | |||
| White | 193,465 (83.1%) | 48,445 (84.3%) | 145,020 (82.7%) |
| Black | 19,363 (8.3%) | 4,738 (8.2%) | 14,625 (8.3%) |
| Hispanic | 7,437 (3.2%) | 1,547 (2.7%) | 5,890 (3.4%) |
| Other † | 12,662 (5.4%) | 2,762 (4.8%) | 9,900 (5.6%) |
| Hypertension | 149,121 (64.0%) | 41,051 (71.4%) | 108,070 (61.6%) |
| Hypercholesterolemia ‡ | 96,465 (41.4%) | 30,196 (52.5%) | 66,269 (37.8%) |
| Family history of CAD § | 56,098 (24.1%) | 13,930 (24.2%) | 42,159 (24.0%) |
| Angina pectoris | 28,777 (12.4%) | 12,064 (21.0%) | 16,713 (9.5%) |
| Stroke | 24,438 (10.5%) | 8,683 (15.1%) | 15,755 (9.0%) |
| Stroke/cerebrovascular disease | 34,792 (14.9%) | 12,104 (21.1%) | 22,688 (12.9%) |
| PCI | 35,191 (15.1%) | 21,346 (37.1%) | 13,845 (7.9%) |
| CABG | 35,164 (15.1%) | 16,846 (29.3%) | 18,318 (10.4%) |
| PVD | 24,670 (10.6%) | 9,310 (16.2%) | 15,360 (8.8%) |
| COPD | 36,646 (15.7%) | 11,663 (20.3%) | 24,983 (14.2%) |
| Smoker || | 66,558 (28.6%) | 15,171 (26.4%) | 51,387 (29.3%) |
| Diabetes mellitus | 71,358 (30.6%) | 22,341 (38.9%) | 49,017 (27.9%) |
| Renal dysfunction ¶ | 28,644 (12.3%) | 10,699 (18.6%) | 17,945 (10.2%) |
| Systolic blood pressure (mm Hg) # | 142.7 ± 33.4 | 141.2 ± 33.2 | 143.2 ± 33.4 |
| Pulse (beats/min) | 87.5 ± 24.4 | 88.4 ± 24.5 | 87.3 ± 24.4 |
| Body mass index (kg/m 2 ) ∗∗ | 28.0 ± 6.5 | 27.9 ± 6.5 | 28.1 ± 6.5 |
| Killip class III-IV | 18,722 (8.0%) | 5,671 (9.9%) | 13,051 (7.4%) |
| STEMI †† | 86,761 (37.2%) | 18,110 (31.5%) | 68,651 (39.1%) |
| Non–STEMI ‡‡ | 146,166 (62.8%) | 39,382 (68.5%) | 106,784 (60.9%) |
| Anterior/septal | 40,951 (17.6%) | 7,545 (13.1%) | 33,406 (19.0%) |
| Prehospital delay ≥2 h | 68,484 (51.6%) | 17,039 (51.1%) | 51,445 (51.8%) |
| Ejection fraction <40% | 52,909 (28.1%) | 17,651 (39.7%) | 35,258 (24.5%) |
| LDL cholesterol (mg/dl) | 104.1 ± 37.8 | 95.4 ± 37.1 | 106.5 ± 37.7 |
| HDL cholesterol (mg/dl) | 40.4 ± 13.7 | 39.3 ± 13.4 | 40.7 ± 13.8 |
∗ Age <45 years set to 45 years old, and (in accordance with the Health Insurance Portability and Accountability Act ) age >90 years set to 90 years old.
† Included Asian/Pacific Islander, American Indian/Native American, and other race/ethnicities.
‡ Defined as a history of, or currently documented, serum cholesterol level >200 mg/dl or previous diagnosis by a physician if the patient could not remember an exact value.
§ Defined as an immediate relative receiving a diagnosis of CAD before 60 years old.
|| Current smoker (smoking within previous year).
¶ Defined as renal insufficiency and/or failure (renal failure was not present in NRMI 4 and was set to “none”).
# Values >250 mm Hg set to “missing.”
∗∗ Defined as weight/(height/39.37) 2 , where weight value of 364 kg and height value of 96 in. set to “missing.”
†† Defined as ST-segment elevation or left bundle branch block (new/unknown/old) on first or subsequent 12-lead electrocardiogram.
The reported preadmission medication use demonstrated that patients with a history of MI were more frequently using guideline-recommended medical therapies for CV disease, including β blockers, angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers, lipid-lowering agents (LLAs), and aspirin than were those patients without a history of MI ( Figure 1 ). However, the use of standard-of-care CV disease pharmacotherapies for patients with a history of MI was reported in only ≤½ of patients. Patients without a history of MI had a significantly lower reported prearrival CV disease medication use across all drug categories ( Figure 1 ).
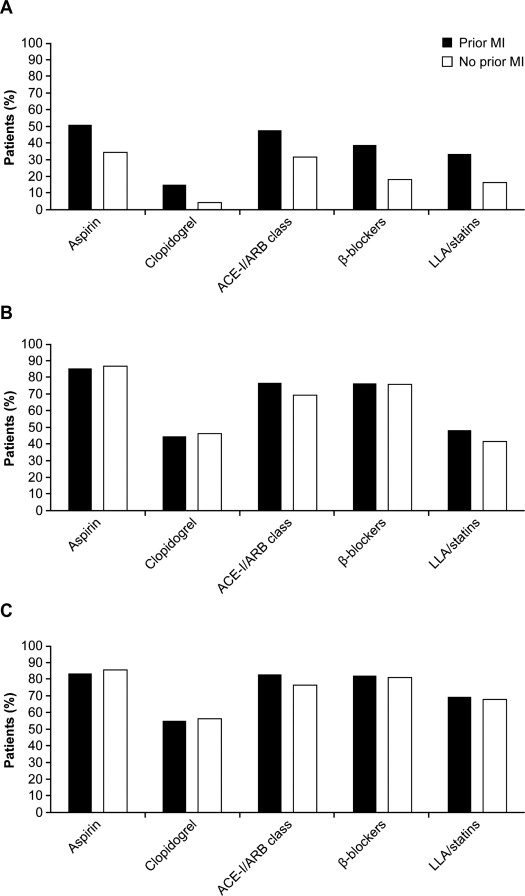
The in-hospital usage of aspirin, β blockers, angiotensin-converting enzyme inhibitors, angiotensin II receptor blockers, and LLAs was greater than the preadmission usage, as expected, and was comparable between the 2 groups ( Figure 1 ). However, although the LLA use was increased in the in-patient setting, the usage rate was only 48% for patients with a previous MI and 42% for those without. The use of coronary revascularization procedures in the NRMI cohort has been previously reported and was not included as a part of the present analysis.
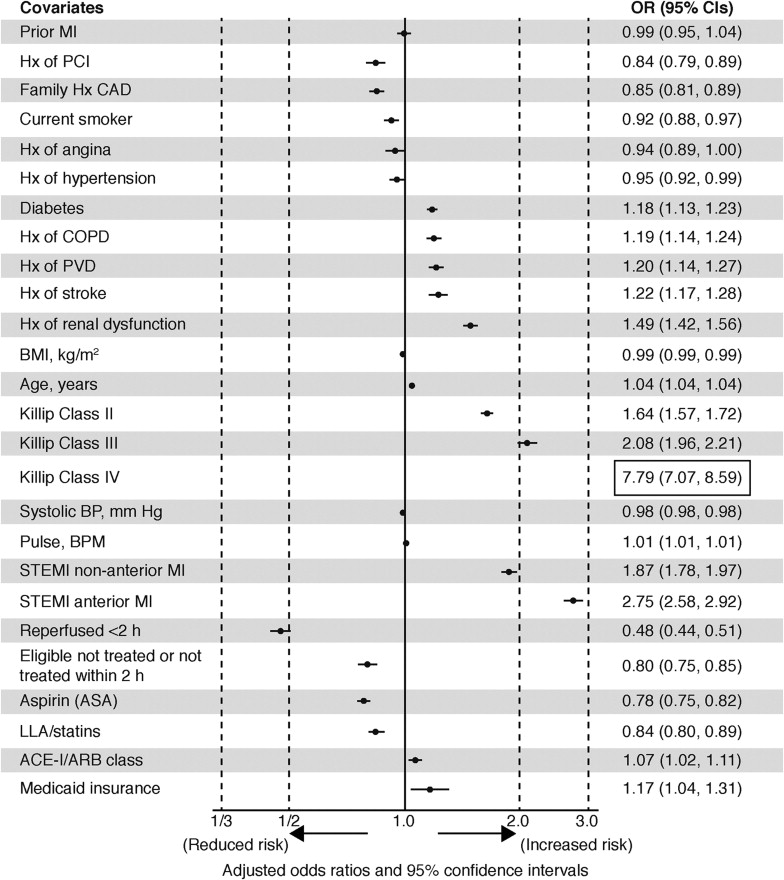
The assessment of in-hospital clinical outcomes with stratification by history of MI included an analysis of in-hospital mortality, recurrent MI, CHF/pulmonary edema, and total LOS ( Table 2 ). No significant difference was found in the risk of in-hospital all-cause mortality in patients with a history of MI compared with those without ( Figure 2 ). The risk of in-hospital all-cause mortality in patients with a history of MI was significantly increased in patients with Killip class III-IV, a history of renal dysfunction, stroke/cerebrovascular disease, peripheral vascular disease, chronic obstructive pulmonary disease, and diabetes.
| Characteristic | All Patients (n = 232,927) | Previous MI | |
|---|---|---|---|
| Yes (n = 57,492) | No (n = 175,435) | ||
| In-hospital mortality | 20,549 (8.8) | 5,368 (9.3) | 15,181 (8.7) |
| Recurrent MI | 3,148 (1.4) | 945 (1.6) | 2,203 (1.3) |
| CHF/pulmonary edema ∗ | 46,578 (20.0) | 14,705 (25.6) | 31,873 (18.2) |
| LOS (d) | |||
| Mean | 5.6 ± 5.6 | 5.7 ± 5.7 | 5.5 ± 5.5 |
| Median | 4.0 | 4.2 | 4.0 |
∗ In National Registry of Myocardial Infarction (NRMI) 4, CHF/pulmonary edema not treated and CHF/pulmonary edema receiving separate treatment in NRMI 5, only 1 variable (CHF/pulmonary edema).
Patients with a history of MI had an 18% increased risk of in-hospital recurrent MI during their in-hospital stay ( Table 3 ), They also had a significantly increased risk of in-hospital CHF/pulmonary edema, with an interaction between a history of MI and diabetes ( Table 3 ).
| Parameter | In-Hospital Recurrent MI | CHF/Pulmonary Edema |
|---|---|---|
| Previous MI ∗,† | 1.18 (1.08–1.29) | – |
| Diabetes ∗,† | 1.14 (1.05–1.24) | – |
| No diabetes with previous MI ∗,† | – | 1.23 (1.19–1.28) |
| Diabetes and no previous MI ∗,† | – | 1.37 (1.33–1.42) |
| Diabetes and previous MI ∗,† | – | 1.57 (1.50–1.64) |
| Family history of CAD | 1.20 (1.10–1.31) | 0.82 (0.80–0.85) |
| History of | ||
| Hypertension | – | 1.08 (1.05–1.11) |
| Angina | 1.54 (1.40–1.70) | 1.16 (1.12–1.21) |
| Stroke/cerebrovascular disease | – | 1.15 (1.11–1.19) |
| PCI | – | 0.90 (0.87–0.94) |
| CABG | – | 1.09 (1.05–1.13) |
| PVD | 1.27 (1.13–1.42) | 1.24 (1.20–1.29) |
| COPD | 1.16 (1.05–1.28) | 1.34 (1.30–1.39) |
| Renal dysfunction ‡ | – | 1.33 (1.29–1.38) |
| Age (yrs) | 1.01 (1.00–1.01) | 1.03 (1.03–1.03) |
| Gender | – | 1.10 (1.07–1.13) |
| Killip class II § | – | 6.15 (5.97–6.34) |
| Killip class III § | – | 10.49 (10.06–10.93) |
| Killip class IV § | – | 3.93 (3.58–4.31) |
| Reperfused <2 h || | 0.50 (0.44–0.57) | 0.72 (0.69–0.76) |
| Eligible but not treated or not treated within 2 h || | 0.89 (0.79–1.00) | 0.86 (0.82–0.91) |
| STEMI ¶ | 3.56 (3.15–4.02) | 1.86 (1.77–1.96) |
| Nonanterior STEMI ¶ | 2.70 (2.43–2.99) | 1.17 (1.13–1.22) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


