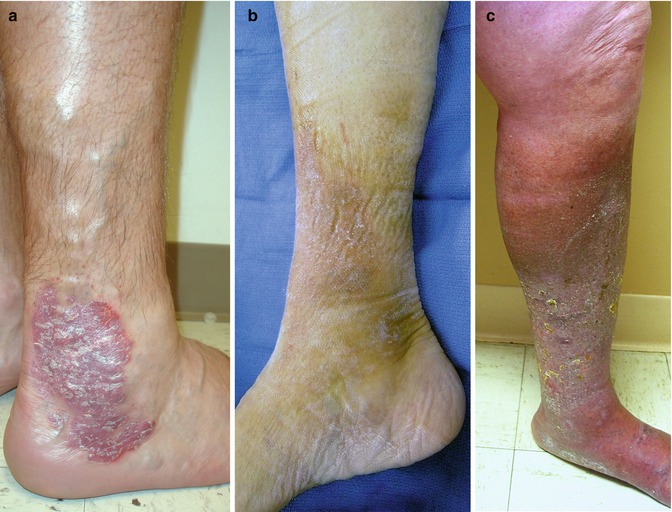
Fig. 3.1
(a) Before treatment Clinical C4 – VCSS 16. (b). Four months after treatment, patient remains Clinical C4. Now C4 – V9
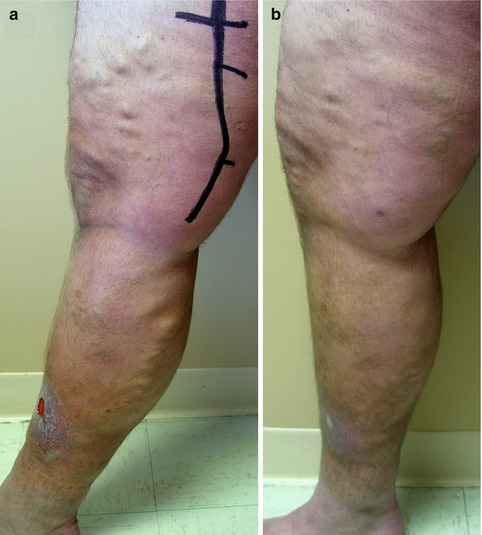
Fig. 3.2
(a) Prior to treatment Clinical C6 – V18. (b). One month after treatment Clinical C5 – V11
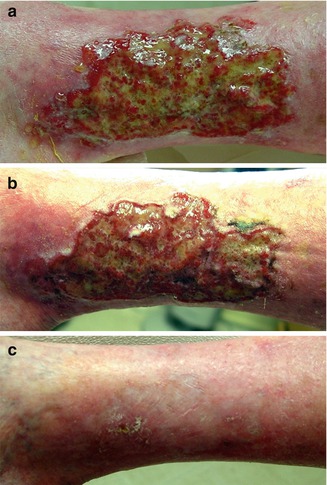
Fig. 3.3
The broadened language of uniting VCSS with CEAP in CVD. Substantial information is relayed in stating C6 – V25 to C6 – V21 and at last C5 – V7. (a) Pre‐treatment. (b) One week post treatment. (c) Two months post treatment
3.3 Venous Clinical Severity Score
The VCSS is a longitudinal measure of nine categories considered universally relevant in the diagnosis and management of CVD. It was designed to supplement CEAP and to provide an evaluative longitudinal assessment of change following treatment and disease progression [16]. It was also designed to give additional weight to more severe manifestations of CVD [18].
The VCSS is generated by the clinician during the course of patient examination and can be followed up readily. It can be used to assess the broader spectrum of CVD, as well as to compare patients with post-thrombotic syndrome and those undergoing different treatment modalities of saphenous venous ablation, stenting for venous obstruction, and pharmacomechanical thrombolysis. Although useful, the original VCSS had drawbacks. Ambiguity in the clinical descriptors was identified as a primary shortcoming of the instrument [19]. In response to these issues, the VCSS has recently been revised [20]. The specific language of proven quality-of-life instruments was used to better address the issues of patients at the lower end of the venous disease spectrum. The language that patients use in describing their symptoms has been considered as well. This revision is designed primarily to clarify the clinical descriptors and make the instrument more precise (Tables 3.1 and 3.2). It has demonstrated good correlation with the results of ultrasonography, and its simplicity makes it easy to administer and score [4]. Recently, a valuable application for the VCSS has arisen in the form of its visual descriptive power. The “visual language of VCSS” is a common framework for consistent physician scoring of venous disease (Fig. 3.4). Similarity in scoring and in descriptions of venous sequelae adds to the structure of the language of CVD.


Fig. 3.4
(a) The “visual language” of VCSS. Consistency in physician scoring and reporting allows a common language of venous disease to emerge. Basic Clinical CEAP 3 – VCSS 7. (b) After treatment scoring changes to Clinical CEAP 2 – VCSS 3
Pain | None: 0 | Mild: 1 | Moderate: 2 | Severe: 3 |
Or other discomfort (i.e., aching, heaviness, fatigue, soreness, burning) | Occasional pain or other discomfort (i.e., not restricting regular daily activity) | Daily pain or other discomfort (i.e., interfering with but not preventing regular daily activities) | Daily pain or discomfort (i.e., limits most regular daily activities) | |
Presumes venous origin | ||||
Varicose veins | None: 0 | Mild: 1 | Moderate: 2 | Severe: 3 |
“Varicose” veins must be ≥3 mm in diameter to qualify | Few: scattered (i.e., isolated branch varicosities or clusters) | Confined to calf or thigh | Involves calf and thigh | |
Also includes corona phlebectatica (ankle flare) | ||||
Venous edema | None: 0 | Mild: 1 | Moderate: 2 | Severe: 3 |
Presumes venous origin | Limited to foot and ankle area | Extends above ankle but below knee | Extends to knee and above | |
Skin pigmentation | None: 0 | Mild: 1 | Moderate: 2 | Severe: 3 |
Presumes venous origin | None or focal | Limited to perimalleolar area | Diffuse over lower third of calf | Wider distribution above lower third of calf |
Does not include focal pigmentation over varicose veins or pigmentation due to other chronic diseases (i.e., vasculitis purpura) | ||||
Inflammation | None: 0 | Mild: 1 | Moderate: 2 | Severe: 3 |
More than just recent pigmentation (i.e., erythema, cellulitis, venous eczema, dermatitis) | Limited to perimalleolar area | Diffuse over lower third of calf | Wider distribution above lower third of calf | |
Induration | None: 0 | Mild: 1 | Moderate: 2 | Severe: 3 |
Presumes venous origin of secondary skin and subcutaneous changes (i.e., chronic edema with fibrosis, hypodermitis) | Limited to perimalleolar area | Diffuse over lower third of calf | Wider distribution above lower third of calf | |
Includes white atrophy and lipodermatosclerosis | ||||
Active ulcer number | 0 | 1 | 2 | ≥3 |
Active ulcer duration (longest active) | N/A | <3 months | >3 months but <1 year | Not healed for >1 year |
Active ulcer size (largest active) | N/A | Diameter <2 cm | Diameter 2–6 cm | Diameter >6 cm |
Use of compression therapy | 0 | 1 | 2 | 3 |
Not used | Intermittent use of stockings | Wears stockings most days | Full compliance: stockings |
On a separate form, the clinician will be asked to: “For each leg, please check 1 box for each item (symptom and sign) that is listed below” | |
Pain or other discomfort (i.e., aching, heaviness, fatigue, soreness, burning) | |
The clinician describes the four categories of leg pain or discomfort that are outlined below to the patient and asks the patient to choose, separately for each leg, the category that best describes the pain or discomfort the patient experiences | |
None = 0 | None |
Mild = 1 | Occasional pain or discomfort that does not restrict regular daily |
Moderate = 2 | Daily pain or discomfort that interferes with, but does not prevent, regular daily activities |
Severe = 3 | Daily pain or discomfort that limits most regular daily activities |
Varicose veins | |
The clinician examines the patient’s legs and, separately for each leg, chooses the category that best describes the patient’s superficial veins | |
Veins must be ≥3 mm in diameter to qualify as “varicose veins” | |
None = 0 | None |
Mild = 1 | Few, scattered, varicosities that are confined to branch veins or clusters. Includes “corona phlebectatica” (ankle flare), defined as >5 blue telangiectases at the inner or sometimes the outer edge of the foot |
Moderate = 2 | Multiple varicosities that are confined to the calf or the thigh |
Severe = 3 | Multiple varicosities that involve both the calf and the thigh |
Venous edema | |
The clinician examines the patient’s legs and, separately for each leg, chooses the category that best describes the patient’s pattern of leg edema. The clinician’s examination may be supplemented by asking the patient about the extent of leg edema that is experienced | |
None = 0 | None |
Mild = 1 | Edema that is limited to the foot and ankle |
Moderate = 2 | Edema that extends above the ankle but below the knee |
Severe = 3 | Edema that extends to the knee or above |
Skin pigmentation | |
The clinician examines the patient’s legs and, separately for each leg, chooses the category that best describes the patient’s skin pigmentation. Pigmentation refers to color changes of venous origin and not secondary to other chronic diseases (i.e., vasculitis purpura) | |
None = 0 | None, or focal pigmentation that is confined to the skin over varicose veins |
Mild = 1 | Pigmentation that is limited to the perimalleolar area |
Moderate = 2 | Diffuse pigmentation that involves the lower third of the calf |
Severe = 3 | Diffuse pigmentation that involves more than the lower third of the calf |
Inflammation | |
The clinician examines the patient’s legs and, separately for each leg, chooses the category that best describes the patient’s skin inflammation. Inflammation refers to erythema, cellulitis, venous eczema, or dermatitis, rather than just recent pigmentation | |
None = 0 | None |
Mild = 1 | Inflammation that is limited to the perimalleolar area |
Moderate = 2 | Inflammation that involves the lower third of the calf |
Severe = 3 | Inflammation that involves more than the lower third of the calf |
Induration | |
The clinician examines the patient’s legs and, separately for each leg, chooses the category that best describes the patient’s skin induration. Induration refers to skin and subcutaneous changes such as chronic edema with fibrosis, hypodermitis, white atrophy, and lipodermatosclerosis | |
None = 0 | None |
Mild = 1 | Induration that is limited to the perimalleolar area |
Moderate = 2 | Induration that involves the lower third of the calf |
Severe = 3 | Induration that involves more than the lower third of the calf |
Active ulcer number | |
The clinician examines the patient’s legs and, separately for each leg, chooses the category that best describes the number of active ulcers | |
None = 0 | None |
Mild = 1 | 1 ulcer |
Moderate = 2 | 2 ulcers |
Severe = 3 | ≥3 ulcers |
Active ulcer duration | |
If there is at least one active ulcer, the clinician describes the four categories of ulcer duration that are outlined below to the patient and asks the patient to choose, separately for each leg, the category that best describes the duration of the longest unhealed ulcer | |
None = 0 | No active ulcers |
Mild = 1 | Ulceration present for <3 months |
Moderate = 2 | Ulceration present for 3–12 months |
Severe = 3 | Ulceration present for >12 months |
Active ulcer size | |
If there is at least one active ulcer, the clinician examines the patient’s legs, and separately for each leg, chooses the category that best describes the size of the largest active ulcer | |
None = 0 | No active ulcer |
Mild = 1 | Ulcer <2 cm in diameter |
Moderate = 2 | Ulcer 2–6 cm in diameter |
Severe = 3 | Ulcer >6 cm in diameter |
Use of compression therapy | |
Choose the level of compliance with medical compression therapy | |
None = 0 | Not used |
Mild = 1 | Intermittent use |
Moderate = 2 | Wears stockings most days |
Severe = 3 | Full compliance: stockings |
The pain component has been adapted to include patient-reported symptoms, such as ache, heaviness, fatigue, soreness, and burning. These symptoms are often found in communicating pain of venous origin. The varicose vein category has been changed to mirror the revised CEAP classification. Corona phlebectatica has been added to this category as a mild finding (Fig. 3.5). The venous edema and skin pigmentation categories (Fig. 3.6) have been changed to reflect the extent of the findings over the surface of the leg. The inflammation category was changed to include terms that indicate acute changes, namely, erythema, cellulitis, venous eczema, and dermatitis (Fig. 3.7). The induration category added the terms chronic edema with fibrosis, hypodermitis, white atrophy, and lipodermatosclerosis to indicate severity and chronicity (Fig. 3.8). Ulcer categories were refined in regard to ulcer size and duration (Fig. 3.9). The category on the use of compression therapy eliminated leg elevation and addresses only the wearing of compression garments [20].


Fig. 3.5
Corona phlebectatica