Pregnancy and Heart Disease
Pregnancy and labor increase the workload on the heart for several reasons. The chief one is that the heart has to pump more blood to meet the extra requirements of the fetus and the tissues that support it. The total volume of blood during a woman’s first pregnancy increases by about 40% to 50%. With succeeding pregnancies or with twins, the increase is greater. At the end of the eighth month, the blood volume stabilizes and remains high until after delivery. In other words, in terms of cardiac work, a pregnant woman is walking up a hill for 9 months, with no way to stop.
Pregnancy has other effects on the circulation. The body tends to hold salt and water, so that most pregnant women have obvious edema. In the later stages of pregnancy, the pressure of the fetal sac on the veins of the pelvis and legs often leads to congestion of the veins with risk of clots. A healthy woman can adjust to all these changes with little risk to herself or the baby. Some women with heart disease can go through pregnancy with no real increase in risk, while others face a risk so high that pregnancy should be prevented or terminated.
What kind of heart disease is a pregnant woman likely to have? Certainly she will not have coronary artery disease. With the rarest of exceptions, coronary disease is unknown in menstruating women.
Rheumatic heart disease is now extremely rare, but it does emerge occasionally and must be dealt with. Hypertension is much more common and presents some specific hazards. Myocarditis or myocardiopathy is rare but dangerous. One specific kind of myocardiopathy associated with pregnancy is especially malignant. Congenital heart disease should have been corrected by the time a woman reaches childbearing age, but there are lapses when medical care is inadequate. I have personally seen a woman reach her eighth month of pregnancy before she presented with an obvious ductus arteriosus.
Before discussing specifics, it’s necessary to understand the functional classification of heart disease. This system was developed by the New York Heart Association and it has proved remarkably reliable (Fig. 15-1).
Functional Grade I: This group includes patients who have heart disease but can carry out any ordinary and even most heavy activities without symptoms or difficulty. These patients have no limitations on physical activity.
Functional Grade II: This includes heart patients who can carry out ordinary physical activity, such as walking, light athletics, and the work of most day-by-day occupations in our society. However, extraordinary exertion such as mountain climbing, strenuous athletics, running, and the like will produce difficulties and must be avoided.
Functional Grade III: This group of patients will suffer symptoms such as shortness of breath or pain even during light-to-moderate activity. A woman carrying bundles from the supermarket to her car, a man walking eight blocks from his home to work, or a golfer strolling about the links would notice some limitation of activity because of these symptoms.
Functional Grade IV: This is the seriously ill group, with symptoms even at rest in a chair or in bed.
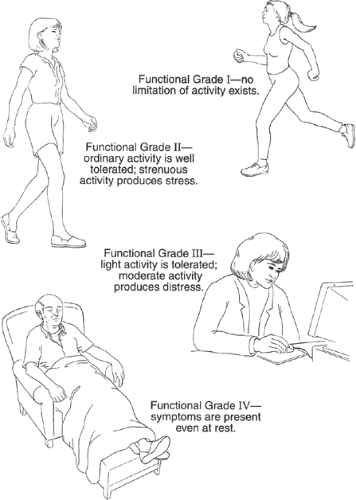 FIGURE 15-1 Functional capacity in heart disease.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|