Hypertensive Heart Disease
Definition of Hypertension
The word hypertension means “high blood pressure.” (It has nothing to do with being nervous or agitated.)
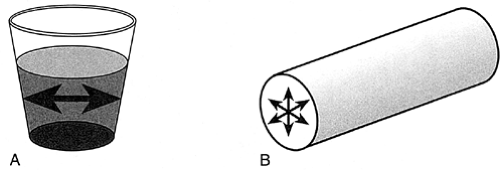
Liquid always exerts pressure on the walls of whatever is holding it. When you fill a glass with water, the water presses against the sides of the glass with a certain measurable force (Fig. 7-1A).
In the same way, the blood presses against the walls of the blood vessels with a definite, measurable force called the blood pressure. The term blood pressure refers to the pressure in the arteries, not the veins (Fig. 7-1B).
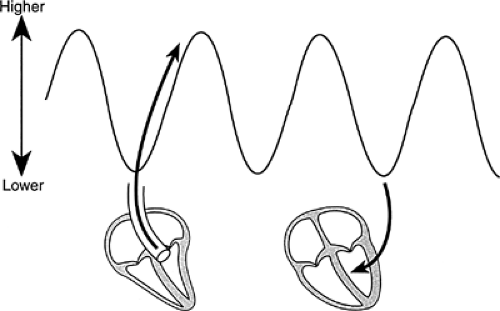
The pressure in the arteries rises and falls with each heartbeat. It rises when the heart contracts, pumping blood into the arteries. It falls during diastole, when no blood is being pumped out of the heart. This change in pressure is what makes it possible to feel a pulse (Fig. 7-2).
With the sphygmomanometer, or blood pressure cuff, it is possible to measure the peak of systolic pressure and the bottom of diastolic pressure. The cuff is inflated with air until it is well over the systolic pressure and then is slowly deflated. When the pressure in the cuff equals the peak pressure in the arteries, a snapping sound will be heard as the blood forces the vessel open at peak pressure only to have it collapse between beats. The sound is produced when the walls of the artery snap shut. All sound will disappear when the pressure in the cuff equals the lowest pressure since the vessel will then stay open throughout the heart cycle. The pressure is described as systolic over diastolic—for example, 120/80.
Question: 120 what? Answer: 120 millimeters of mercury (mm Hg). Blood pressure is measured by the height of a column of mercury in a glass tube that the blood pressure will support.
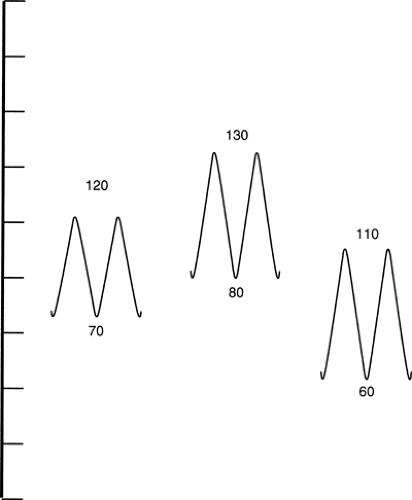
“Normal” blood pressure? You might as well ask “what is a normal height?” There’s a wide range of normal, and everyone’s blood pressure changes from minute to minute. It will rise with excitement or exercise; it may fall during sleep or rest or even on standing from a sitting position. For an average adult, a systolic pressure between 100 and 140 is normal. Diastolic pressure will lie between 60 and 90. A thin, young female or a
highly trained athlete might have a systolic pressure under 90 with no ill effects while a healthy 60-year-old might have a pressure of 156/90 as a normal finding (Fig. 7-3).
highly trained athlete might have a systolic pressure under 90 with no ill effects while a healthy 60-year-old might have a pressure of 156/90 as a normal finding (Fig. 7-3).
Kinds of Hypertension
The arteries aren’t just passive tubes. They are living organs with nerves and strong muscles: they can expand or constrict with the speed and power of a snake. Normal arteries are elastic; they have a lot of “give.” By expanding when blood is pumped out of the heart and contracting during diastole, they help to equalize pressure during the heart cycle.
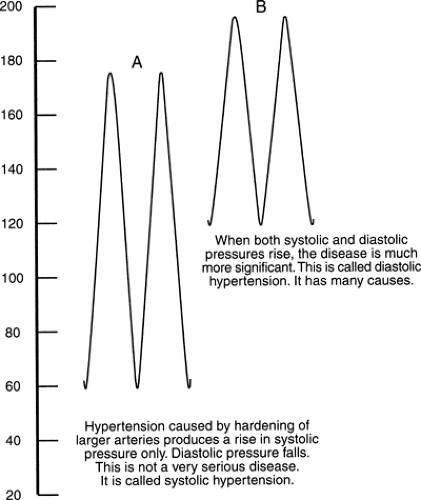
In older patients, the arteries may become rigid and pipelike. Now the vessels are like a boxer who can’t “roll with the punches.” With no give in the system, the systolic pressure will be abnormally high. The diastolic pressure will remain normal. This is systolic hypertension; it was formerly thought to be harmless, but we now know that it isn’t (Fig. 7-4A).
If the arteries become constricted and stay that way, the blood pumped out of the heart is forced into a smaller container. The pressure has to rise. Both systolic and diastolic pressures go up. This is diastolic hypertension—it may be dangerous and it always needs treatment (Fig. 7-4B).
Complications of Hypertension
Hypertension is a dangerous disease because it can produce three major, potentially lethal complications.
Congestive Heart Failure
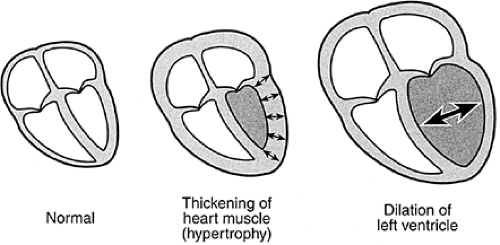
Imagine a worker who has the job of pumping water up a 20-foot (ft) pipe. He can do this easily. Suddenly he’s asked to pump water up a 10-story building. The effort of pumping against the enormous increase in pressure will wear him out. For a time his muscles will enlarge as he struggles with the abnormal load, but finally, he’ll be exhausted and he won’t be able to pump water out of his pipe as fast as it flows in. The water will back up and there will be flooding somewhere in the system. This is exactly what happens to the left ventricle when it has to pump against a high pressure. At first the muscle wall thickens in an attempt to compensate (Fig. 7-5), but finally the heart fails: it can’t pump blood out into the aorta as fast as it runs in from the lungs, and the pressure backs up into the lungs with congestive heart failure. This can happen abruptly: it is common to see a hypertensive patient who has been substantially free of symptoms suddenly go into massive pulmonary edema. Most cardiologists would probably tell you this is statistically the commonest cause of abrupt, life-threatening left heart failure. It is not clear why the break in cardiac compensation is so abrupt or
why patients tolerate a high blood pressure so long without warning symptoms, but the phenomenon of sudden, life-threatening pulmonary edema in a hypertensive patient is familiar to every emergency department physician.
why patients tolerate a high blood pressure so long without warning symptoms, but the phenomenon of sudden, life-threatening pulmonary edema in a hypertensive patient is familiar to every emergency department physician.
Stroke
The word stroke is the same as the medical term cerebrovascular accident. It means that the blood supply to some part of the brain has been cut off. This can happen because a blood vessel ruptures and bleeds or because a vessel becomes plugged in
some way. Hypertension puts an enormous strain on the smaller arteries, and they can simply rupture. The result is like having a nosebleed in the brain: a certain amount of brain tissue loses its blood supply and the cells die. When the blood supply to brain cells is cut off, they begin to die within 10 minutes. The effect on the patient, of course, depends on which cells are affected: there may be paralysis of major parts of the body or there may be no more than a temporary blurring of consciousness.
some way. Hypertension puts an enormous strain on the smaller arteries, and they can simply rupture. The result is like having a nosebleed in the brain: a certain amount of brain tissue loses its blood supply and the cells die. When the blood supply to brain cells is cut off, they begin to die within 10 minutes. The effect on the patient, of course, depends on which cells are affected: there may be paralysis of major parts of the body or there may be no more than a temporary blurring of consciousness.
It’s frightening to think that the effects of a stroke are a matter of simple chance—the results depend on which blood vessel ruptures and where in its course the rupture occurs. Hypertension was once the commonest cause of stroke, but with better medical agents and better treatment there has been a very encouraging drop in the occurrence of hypertensive strokes in recent years. In fact, the partial conquest of hypertensive stroke has been one of the major advances of modern medicine, much more important in long-term effect than all the spectacular advances in cardiac surgery.
Coronary Artery Disease
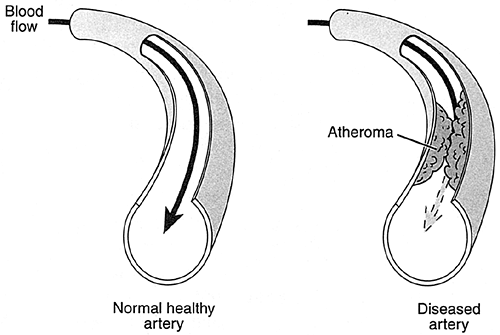
The cells that form the lining of the coronary arteries are often damaged when the pressure within the vessel is abnormally high. They begin to degenerate, and masses of fat, or atheromas, are likely to form, tending to block the flow of blood through the vessel (Fig. 7-6). Patients with hypertension face at least a 200% increase in risk of coronary artery disease. Why does hypertension affect the lining of the coronary arteries? The answer is not at all clear, but the association is established beyond question. Does control of blood pressure prevent coronary disease? It’s reasonable to think so, but the results so far are not as clear-cut as in the prevention of stroke: more data are needed.
Kidney Failure
This is a “chicken-and-egg” situation. High blood pressure can certainly produce damage in the blood vessels of the kidneys, often with severe kidney failure. On the other hand, kidney disease can produce high blood pressure. Sometimes it is hard to tell which caused which.
When an intelligent physician detects high blood pressure, it’s not an end point; it’s the signal for a swift clinical investigation:
What kind of hypertension is present? Mild and relatively benign? Severe and dangerous?
What associated diseases are present?
What complications are present?
Can a specific cause be found?
Note: Practically all these complications can be prevented by controlling high blood pressure.
Varieties of Hypertension: Causes and Treatment
Modern understanding of hypertension began when a physician named Goldblatt put a clamp on the renal artery of a dog, cutting down the blood flow to the kidney. When he did, the dog’s blood pressure went up. Extensive research showed that when the kidney tissue wasn’t receiving an adequate blood supply, a chemical called renin was released into the bloodstream in large amounts. This chemical acts as an enzyme splitting certain proteins to produce a substance called angiotensin I. Still another enzyme converts this substance to angiotensin II, a powerful agent that causes constriction of the small arteries and a rise in blood pressure. While this reaction was first detected when a kidney was deliberately damaged, years of study have shown that this interplay of chemicals is the basis of a great deal of hypertension even when there is no kidney disease. This isn’t the only mechanism of hypertension, but it’s a very important one and will reappear throughout this chapter. Some studies have concentrated on the effect of chemicals released at nerve endings in the walls of small blood vessels, whereas others have correlated changes in the anatomy of arteries with hypertension. All these elements play a role in treatment and outcome.
The great majority of patients with severe kidney disease will suffer from hypertension, but the reverse is not true. Only a small minority of cases of hypertension are caused by kidney disease.
Essential Hypertension
In about 90% of cases, there’s no cause for hypertension anyone can find. The medical profession calls these cases “essential hypertension.” (Beautiful word, essential—it’s mysterious, impressive, and totally insignificant. If a patient had a high fever for no known reason, the diagnosis of essential hyperpyrexia would probably make everyone feel a lot better, but all it really says is that the patient has a fever and the physician doesn’t know why.) In a small minority of cases, a specific cause of hypertension can be detected: kidney disease, tumors of the adrenal gland, or congenital abnormalities; these will be described later. At this point, it’s important to concentrate on the vast majority of cases in the essential group.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree