Cardiac Surgery
Forty to 50 years ago, the idea of operating on the inside of the heart was pure science fiction. Now it happens every day in every major hospital in the Western world. How this all came about is a fascinating study in the way science works: this can’t happen until that’s discovered, and that can’t be discovered until something else is perfected, and so on. For instance, before World War II the only possible kind of heart surgery took place outside the heart. A patent ductus arteriosus could be closed off without invading the heart itself. The operation worked well and it wasn’t dangerous.
The first attack on disease inside the heart was surgery for mitral stenosis. It’s technically easy to insert a finger into the left atrium and break open the adhesions that hold the valve shut (Fig. 21-1). The problem was that there are practically always blood clots in the atrium when mitral stenosis is present. The first attempts at surgery were a disaster because blood clots were loosened and went floating out into the arteries like time bombs.
How to get rid of the clots? In 1941, a researcher at the veterinary school of the University of Wisconsin, Dr. Karl Paul Link, isolated a chemical that kept blood from clotting. It was called dicumarol, and it was the first substance of its kind in human history.
A Swedish physician named J. Eric Jorpes discovered another anticlotting drug, heparin. Now the way was open for heart surgery. After World War II, the operation for mitral stenosis became a standard procedure with very little risk.
Anticoagulant medication is given for a sufficient period before the operation so that there is no danger from clots. All the old clots will “organize,” that is, they will be slowly disintegrated by the natural process of the body and no new ones will form.
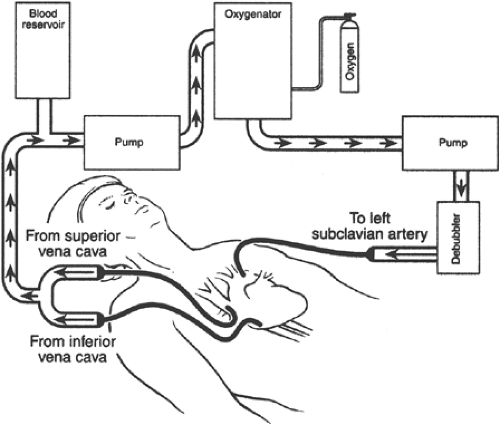
The next technical stride was the invention of the heart-lung machine (Fig. 21-2). Perfected in the fifties and sixties, this machine takes the blood out of the superior and inferior vena cavae and bypasses the heart and lungs, returning the blood to an artery. The machine oxygenates the blood and propels it ahead into the arteries, thus performing the functions of both heart and lungs. Now the surgeon can actually cut open the heart and repair the inner structures. It’s difficult to work on a beating heart, however. That problem is solved by actually stopping the heartbeat with a heavy dose of potassium or by packing the heart in slush. Either way, the heart is still and the surgeon can work precisely.
Valve Replacement
Artificial valves can be implanted in the mitral or aortic position. They can be made of metal and plastic or they may be actual tissue valves called bioprostheses that are usually from a pig (Fig. 21-3). The problem is there is always danger of clotting or infection.
The parts of a mechanical valve can wear out, and the tissue of a bioprosthesis can degenerate or calcify. The perfect valve hasn’t been invented yet, but some patients have excellent results for many years—practically through a normal lifetime.
The parts of a mechanical valve can wear out, and the tissue of a bioprosthesis can degenerate or calcify. The perfect valve hasn’t been invented yet, but some patients have excellent results for many years—practically through a normal lifetime.
Note: There is always danger of endocarditis on an implanted valve. Endocarditis prophylaxis is particularly important. Clotting is another danger: mechanical valves should always be protected by anticoagulants. So should mitral bioprosthetic valves. The only artificial valve that doesn’t present much danger of clotting is an aortic bioprosthetic valve.
Whenever a patient with an artificial heart valve suddenly shows signs of failure, assume the valve is not functioning normally. It may be stuck or it may be leaking. In either case, it’s an emergency. Move fast for corrective surgery.
Repair of Congenital Heart Defects
Septal defects can be closed with patches. Coarctation of the aorta can be repaired with a Dacron prosthesis or, in some cases, by simply cutting out the narrow area and sewing the ends of the vessel together. Practically any congenital abnormality can be corrected, partially or completely, now that the surgeon has a still, bloodless heart to work with.
Coronary Artery Bypass
It hasn’t been possible to “un-harden” an artery. Once an atheromatous mass plugs up a vessel, it’s there to stay. (At least until recently.)
But why not go around the obstruction? How about a detour? Dr. René Favaloro of Buenos Aires decided that might be a good idea. He took a piece of vein out of a patient’s leg and grafted, or tacked, one end of it to the aorta. He then attached the other end to the coronary artery beyond the point of obstruction. The “coronary artery bypass” was thus born (Figs. 21-4 and 21-5).
Coronary artery bypass surgery is now, by far, the most common heart operation in the world. How well does it work? Who needs it? What is the risk?
If the graft system stays open, the results are good. About 20% of grafts will close within the first 6 months and about 4% more will close each year after that. That’s the best anyone’s been able to do. The vein grafts close because of blood clots, new atheromas, or thickening of the lining cells of the vein.
Pluses, Minuses, and Reasonable Expectations
| Annual mortality from coronary disease based on vessels involved: | |
|---|---|
| RCA alone | 2.8% |
| LAD alone | 4% |
| Circumflex alone | 4% |
| Combination of any two of the above | 7% |
| All three of the above | 12% |
| LMCA alone | 12% |
Within these limitations, coronary bypass surgery is useful in the treatment of angina. It can be counted on to relieve pain when medical measures fail; it cannot be counted on to prolong life in more than 15% of patients. Thus, coronary bypass
surgery is a reasonable alternative when angina is so severe that it prevents a patient from living a reasonably normal life and when medical measures have failed. Who can expect to live longer as a result of coronary artery surgery? Obviously, the mortality from single-vessel disease of any of the three branches is so low that it’s not reasonable to expect major heart surgery to improve it, and it doesn’t.
surgery is a reasonable alternative when angina is so severe that it prevents a patient from living a reasonably normal life and when medical measures have failed. Who can expect to live longer as a result of coronary artery surgery? Obviously, the mortality from single-vessel disease of any of the three branches is so low that it’s not reasonable to expect major heart surgery to improve it, and it doesn’t.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree